Orange Substance on Tissue Paper after Wiping: Likely Cause
Did you just collect an orange substance on the tissue paper from wiping yourself after urinating?
Why’s It OK to Call a Thin Woman Unhealthy but not a Fat One?
Followers of obese influencers get furious when someone says “Obesity is not healthy,” but these same followers will call a thin woman unhealthy. (more…)
Why Do Older Men Let Their Butts Fly up with Lat Pull-downs?
Ever notice that nearly every senior age man does lat pull-downs by lifting his butt off the seat before each pull?
Big Toenail Subungual Hematoma: Images Show Healing Over Time

JUNE 11
Here are serial images of a big toenail subungual hematoma showing how the old blood and bruise heal over an eight month period.
In the June 11 image above, a subungual hematoma (mass of blood under the nail) of the big toe is very evident. (more…)
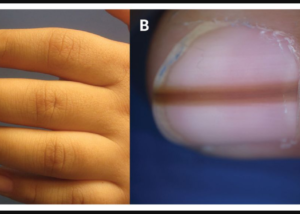
What Cancer Other than Melanoma Causes Hutchinson’s Sign?
If you see what appears to be Hutchinson’s sign in a fingernail or toenail, your first thought might be melanoma skin cancer. (more…)
If All Bodies Are Beautiful what About All Faces? Face Positivity
We keep getting “body positivity” shoved down our throat. What about women with homely faces? When’s their ship going to come in?
Why don’t we see THEM strutting catwalks and getting on covers of magazines?
In fact, the very phrase, “All faces are beautiful,” isn’t even used amid all the body positivity hoopla.
Even women with conventionally attractive bodies don’t stand a chance of getting a modeling gig if they have a plain Jane face, let alone a “dog face.”
Professional Models
Look, I get it: It’s important that a model have a pretty face. I myself use images of only attractive faces for most of my articles.

However, I also don’t actively campaign for “body positivity,” either. I’m off the hook.
I don’t claim to be a pioneer in this area like Sports Illustrated — which contradicts itself by using only gorgeous-faced women.
What about the increasing media attention towards models with skin conditions?
Well, here’s the problem: The barrier-breaker is their skin, not their facial structure!
Yes, they have acne, large moles or a pigment disorder — yet at the same time, still have a “model’s face” — in terms of structure. This is no coincidence.
Winnie Harlow has allegedly “broken barriers” as the first model with vitiligo to strut a Victoria’s Secret show.
BUT … Winnie’s facial structure is traditional model caliber. Check out her beauty below.
Winnie Harlow — a classically beautiful face that just happens to have de-pigmentation.
Amy Deanna landed a contract with CoverGirl, a company that claims body positivity due to this move. Gee what a coincidence that her face is structured like the typical runway model’s!

Amy Deanna. Would CoverGirl had hired her if her lips were thin and eyes closer together?
Let’s see CoverGirl hire a woman with either of the faces below for any contract! That’s the day hell will freeze over.

Sports Illustrated, CoverGirl, you interested?

We should gun for “Lip Positivity.”
We can put a bunch of big splotchy moles on Ashley Graham’s face, and doggone it, she’d still be gorgeous!
We can give Emilia Clarke’s face a noticeable case of vitiligo – and let’s toss in several giant zits while we’re at it — and crikey, she’d still be beautiful!

Emilia Clarke, actress
When I speak of facial beauty or homeliness, I can’t say this enough: I refer to features and proportions, NOT skin color variegation or large moles or patches.
Target’s “Inclusive” Swimwear Campaign
Four models, all with YOUNG faces. Below is one of them. Note the skin difference.

Source: Target’s Shade & Shore line
What else do you notice? Hint: Imagine her without the skin condition.
What do you see? It’s obvious: a face that’s STRUCTURED like that of a conventional model’s!
Paint on some eyebrows, add false eyelashes, eyeliner, eye shadow and lipstick, and she’d be quite attractive despite the rough skin.
Target falls short on inclusion because all the women in their Shade & Shoreline campaign have YOUNG, STRUCTURALLY PRETTY faces.
Recording Artists
For once, I’d like to see a recording artist (plus size or not) hit it big who has an unbecoming face.
I’m not talking about winners of those TV talent shows. I’m talking about those who blow into the public eye out of nowhere and hit it huge.
Now before you start naming successful “fugly” female recording artists, I need to point out that facial beauty is outright required for three genres of music:
• Top 40
• Country
• Hip hop and whatever else you call today’s music
Requirements are looser for rap, grunge rock and alternative, but let’s stick to the big 3.
Name one wildly popular, contemporary recording artist in any of these three genres who is homely.
This excludes those you hate. Some people have posted that Beyoncé, Katy Perry, Taylor Swift, Britney Spears, Rihanna and Ariana Grande are ugly. It’s no coincidence that their posts also spew a lot of hatred towards these performers.
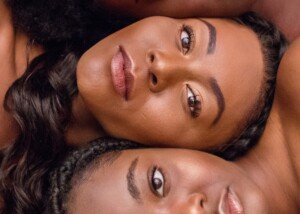
Would Taylor Swift, Alicia Keys, Rihanna or Cardi B gotten their big break if they looked like the two women below?


Joel Mott/Unsplash
Now before you point out that these artists are very talented and that their looks are only coincidental, then how about explaining why – once again – we NEVER see a woman with a homely face who hits it big in pop, soft rock, country or hip hop?
You may be thinking of Barbra Streisand and Celine Dion, but their exceptional pipes cancel out their less-than conventionally attractive faces. Plus, that’s only two out of a boatload.
Keep in mind that “not beautiful” does NOT mean ugly. Think of this as four categories: Ugly/homely, Plain, Pretty and Beautiful.
With makeup ON, name one recording superstar who’s Plain, let alone Ugly/homely.
And don’t let your hatred towards her skewer your perception of her face. Be objective. CAN you name even one?
Even Lady Gaga, with makeup, certainly isn’t a plain Jane, and it’s with makeup that counts, since nobody ever performs or attends functions or photoshoots without makeup.
• Are we to believe that all the good looks in the recording industry are just a coincidence?
• Are we to believe that only women with pretty faces can sing, dance and play a flute?
• Are we to believe that homely women can’t sing?
Recording studio executives know that ugly doesn’t sell; only beauty does – even if it’s on a 230 pound body.
It’s no coincidence that Adele has a very pretty face. You know stinkin’ well that Adele would not have had a snowball’s chance in hell if she’d had a face like Rosie O’Donnell.
It’s amazing that women will cry for body positivity but at the same time would never pay to see a “fugly” woman perform on stage.
Body Positivity Calendars and More
Show me ONE plus size woman on a body positivity calendar whose face isn’t pretty.
The body positivity movement still has a very long way to go.
This includes the photographers who pat themselves on the back and boast inclusivity when photographing women with skin disorders – yet most of their subjects have Golden Ratio proportions!
Source: Target
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Much Should You Worry About Melanoma in Your Child?
Do you worry that your anxiety over your child developing melanoma might be unrealistic, but you just can’t help obsessively inspecting their moles and imagining the worst?
Yes, melanoma occurs in children, even those with olive skin. In fact, no dermatologist will ever say that a child with dark skin is immune to this deadly skin cancer.
But let’s put things into perspective to ease your ongoing anxiety or obsession about melanoma affecting your child or teen.
“According to the American Academy of Dermatology Diagnosis, the number of cases diagnosed in child patients is between 300 and 400 each year,” says Dr. Gretchen Frieling, MD, Triple Board Certified Boston Area Dermatopathologist.
“This makes it rare in children and can look different on them than it does on adults,” continues Dr. Frieling.
“However, the ABCDEs can still help parents identify suspicious lesions. In any patient, child or adult, early diagnosis can alleviate some of the burdens of the condition and/or the treatment.”
One of the biggest differences between many cases of childhood melanoma and that affecting adults is that in the young population, the tumor is often one color.
We are taught that a mole of changing colors over time, or a mole that we’ve never noticed before (e.g., first-time skin self-exam) that has multiple colors, needs to be examined by a dermatologist.
This can create the idea that a mole of one uniform color is benign. But kids can have a melanoma that seems to be a harmless mole of one color.
This is why it’s important to be aware of other changes that can get a dermatologist’s attention, such as fast changes in the spot’s size and shape, and even new elevation, in that previously it was flat.
Another sign that a dermatologist would be interested in is if there’s one mole that looks different from all of your child’s other moles.
• It’s much darker than the rest.
• Or, all her moles are very dark, but one is very light brown.
• All are round, but one has jagged edges or is very large.
At the same time, parents need to know that it’s perfectly normal for benign moles to begin appearing throughout childhood.

Normal moles on a child’s back. Shutterstock/Albina Glisic
While you should be familiar with your child’s moles, there is no reason to let anxiety get the best of you.
Remember, 300 to 400 new diagnoses each year in the U.S. means that this disease isn’t just rare in kids – it’s outright exceedingly rare.
Nevertheless, it’s a smart idea to simply view the moles from time to time – discreetly, so as not to transfer any anxiety or self-consciousness onto your child.
At the same time, do not become obsessive over an illness that strikes only 300-400 kids a year!
Signs of Obsessing Over Your Child’s Moles
• You created a mole map for every mole, either by placing dots on a pre-illustrated child’s body, or drawing sections of your child’s body yourself and placing the dots there.
• You take pictures of your child’s moles and study them.
• You compare the pictures to previous pictures.
• You use an app for mole checking on your child.
• You inspect his moles, from top to bottom, every month without fail, and inspections aren’t quick.
• You frequently ask her questions such as, “Have you noticed that mole before?” “Has that mole always looked like that?” “Does that mole seem darker lately?”
Dermatologists urge parents to be vigilant about their children’s skin health. But at the same time, it’s crucial to keep things in perspective and be realistic rather than a worry wort.
“This can cause them stress and anxiety if they are a parent and hovering over a child’s every mole or spot,” says Dr. Frieling.
“This can distress the child and even transmit some anxiety and fear to the child.”
How to Ease Fear of Melanoma Developing in Your Child:
Facts to Know, Practices to Do
• New moles, again, normally develop throughout childhood and the teen years.
• Because new moles are always developing, it’ll be normal to notice some getting bigger very gradually over time.
• Location of a newly developing mole is not indicative of an increased likelihood of melanoma.
• Moles can be flesh colored, tan, any shade of brown and even almost black.
• Take your child in for an annual skin check by a pediatric dermatologist. This annual exam will go a long way at easing your anxiety.
• Make application of sunblock a non-negotiable routine prior to time spent outdoors.
• It’s perfectly okay to put sunblock on a baby. No baby should ever get a tan, let alone sunburn.
Stop worrying and obsessing. Instead, focus on things that are more likely to harm your child such as not wearing a seatbelt and not being trained in stranger safety!
 Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/TheVisualsYouNeed
Child’s Melanoma vs. Adult’s: Appearance Comparison
The ABCDE rules of melanoma screening for adults don’t apply to children.
There are distinct differences in the way melanoma appears in kids than it does in adults. (more…)
Can a Basal Cell Carcinoma Be Purple?
Basal cell carcinoma is typically described as a nodule or bump that may be pearly in color, but also flesh toned or some range of pink.
Purple is a color that may come to mind for some people concerned over discovering a stubborn nodule or small bump on their skin that just won’t go away.
Though basal cell carcinoma is the least evil of all the different kinds of cancer that can affect the skin… hearing, “You have basal cell cancer,” can still leave a person sleepless the following night.
If neglected (ignored, not treated), this malignancy can cause serious local destruction of nearby tissue.
The Color Purple
“Basal cell carcinoma can present as a flesh-colored or brown spot on the skin,” says Dr. Gretchen Frieling, MD, Triple Board Certified Boston Area Dermatopathologist.
“It can also present itself as a bleeding or scabbing lesion that heals and returns,” continues Dr. Frieling.
“In those instances, the scabbing can make it look a bit purple, but basal cell carcinoma is usually identified by its pearly, light color or a brown spot.

A basal cell carcinoma lesion displaying a scabby, brownish-dull purple appearance.
“Kaposi sarcoma, however, is a more rare form of cancer that occurs in the skin’s blood vessels and can cause purple or red patches of skin.”
If you’re diagnosed with a basal cell carcinoma, do not panic. This type of tumor very rarely metastasizes, even when local destruction has already occurred.
It also cannot turn into melanoma, the most serious form of skin cancer.
But if you suspect that the stubborn pimple-like lesion on your forehead, nose, cheek, near the eye, ear, scalp or any sun-exposed body might be a BCC, do not put off getting it examined just because you just read that a BCC very rarely spreads to other parts of the body.
Promptly get it examined — because melanoma can mimic the appearance of a basal cell carcinoma to the untrained eye.
Any spot, nodule, bump, blemish or patch on the skin that doesn’t go away after two or three weeks should be examined by a dermatologist, regardless of color – be it flesh, pink, purple, brown, tan or whatever.
 Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
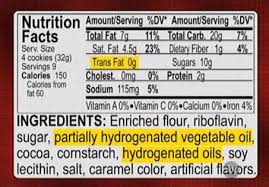
Trans Fats: the Killer Among Us: How to Avoid this Food Ingredient
While gun control dominates the news, thousands of Americans every year die at the hands of trans fats in common foods.
Trans fats should be banned. Where is the outcry?
Trans fats are a poisonous additive that the FDA allows into the American food supply.
It’s not as easy as “Just avoid eating anything with trans fats” when a loved-one with poor heart health doesn’t care.
Or, to put it another way, many people, even those who’ve undergone bypass surgery for clogged coronary arteries, still aren’t convinced that trans fats are poisonous to the heart.
They’re not convinced because putting trans fats in foods is legal.
How many Americans die every year at the hands of trans fats?
“According to the CDC, reducing trans fat consumption could prevent 10,000-20,000 heart attacks and 3,000-7,000 coronary heart disease related deaths each year,” says Alison Massey MS, RD, LDN, registered dietitian and certified diabetes educator with over 10 years of experience in various community and clinical settings.
“These numbers were calculated from FDA data assuming that individuals consumed 1.3 grams from trans fats” daily, adds Massey.
What’s 1.3 grams?
That’s more than many people think. The amount of this toxic substance can easily exceed 1.3 grams a day because it’s in so many food items, including seasonings, and including items with a container that says “Zero trans fats per serving.”
The FDA allows food makers to label a product as “Zero trans fats” or “No trans fats” – “per serving” – as long as the designated “serving size” equates to less than half a gram of this toxin.
However, the “serving size” is usually ridiculously small; the consumer ends up eating multiple servings.
This can occur several times in one day with different food items, easily exceeding 1.3 grams!
Quite frankly, it’s just as insane for a person with heart disease to consume any amount of trans fats as it is for a person with emphysema to smoke.
Why are trans fats harmful to the heart?
“Trans fats elevate the bad LDL cholesterol and lower the good HDL cholesterol levels,” says Massey.
“When LDL levels are elevated, over time they can promote atherosclerosis.” This means plaque buildup in the arteries.
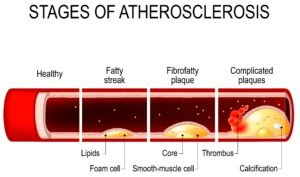
Shutterstock/Designua
Massey continues: “Additionally, some research suggests that trans fat may increase lipoprotein(a), a type of LDL cholesterol, making them small and denser particles that promote buildup of plaque. Trans fat may also increase inflammation, which may play a role in the formation of blockages.”
Insanity
Ever shake your head when you hear about a person who continues smoking after being diagnosed with lung cancer, or who continues drinking after being diagnosed with liver disease?
It’s easier to give up trans fatty foods once a person is diagnosed with heart disease, because there’s no such thing as a chemical or mental addiction to trans fats!
Yet people with severe heart disease, even those who’ve had bypass surgery, continue ingesting this dangerous, unnatural substance.
“I encourage patients to eliminate all trans fat from their diets,” says Massey. “We discuss the fact that even ‘a little’ is not ideal.”
Why are trans fats so prevalent in processed foods?
“There are two types of trans fat: those that are in food naturally, produced in the gut of grazing animals, and those that are formed during food processing, when hydrogen is added to vegetable oil,” explains Massey.
“Trans fat is found in some processed foods because they extend the shelf-life and flavor stability of the product as well as improving texture or ‘mouth-feel’ for certain food items.”
This doesn’t mean that foods without trans fats are inferior in taste, freshness, texture or feel. Many foods that are free of this harmful chemical are absolutely delicious!
How can you tell a food has trans fat?
First of all, never assume something doesn’t have this poison just because the product is promoted as healthy or boasts high fiber or some other nutrient.
There’s only one way to know if a product contains this poison: the ingredients list.
- If you see the words partially hydrogenated in the list, don’t buy the product.
- If you see just hydrogenated, don’t by the product, because hydrogenated alone can mean partially.
- If it says completely or fully hydrogenated, it does not contain trans fats.
- If you see shortening, don’t buy the item, since the shortening may be partially hydrogenated.
- Avoid foods with canola oil; this oil contains trans fats and is not the health-giving oil that it’s been marketed as.
- Finally, avoid foots that contain interestified fats or say interestification in the ingredients list. Though this isn’t a trans fat, it’s just as bad.
To those who balk at reading ingredients lists, since when should this not be a part of smart shopping?
How crushing can your schedule be that you can’t take five minutes to sift through the different brands of stuffing mixes, noodle mixes or snack bars to see which ones contain trans fats?
People will spend more time channel surfing to see which reality show they should watch while eating meals containing trans fats.
Once you know which brands contain this deadly poison, you’ll no longer need to read ingredients lists.
And it’s a given that the bakery section of a conventional food store is Trans Fats Alley.
You don’t have to be faced with the drudgery of figuring out if you’re on track for exceeding 1.3 grams of this poison on a given day; simply avoid trans fats altogether!
Alison Massey has been working in the field of nutrition since 2010 helping individuals make sustainable changes to improve their health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.