Groin Pain Only Overnight: Could this Be a UTI ?
Are you having groin pain, pressure or a gassy feeling there only overnight, particularly after you get back into bed after relieving yourself? (more…)
Why Saying “You Look Tired” Is Among the Rudest Comments

Telling a stranger they look tired is extremely rude and thoughtless, and contrary to myth, is NOT a show of concern.
Men Tell Women to Smile As a Way to Control Them
There is a real obvious reason why men tell women they don’t know to smile: It’s all about control, being the dominant sex, and getting women to smile affirms this need.
Is It Normal Not to Like Being Hugged By Children?

Do you cringe with awkwardness when a parent orders their child to give you a hug? Is it normal not to like getting a hug from another’s child?
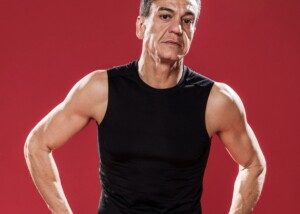
Type of Anxiety & Depression that Responds Best to Exercise

What type of anxiety and depression responds best to exercise for those who don’t want to take medications?
5 Exercises to Make Your Waist Look Thinner with NO Crunches
Here are five exercises to make your waist look thinner without crunches, other ab exercises, sucking in your gut or standing a certain way. (more…)
Strength Tests if You Fear You Have Wrist Drop

Do you keep performing “strength tests” because you think you might have wrist drop and therefore a neurological disease? (more…)
Why You Can’t Climb 5 Flights of Stairs but Can Easily Do One
Why is it that you can easily go up a single flight of stairs, but can barely make it to the fifth flight?
You’re panting hard, legs burning, heart pounding. Why is this?
There are a few reasons why you can easily go up one flight of stairs, but then things start changing quite quickly as you continue climbing.
By the time you’re about to start the fourth flight, you’re noticeably out of breath and slowing down, feeling very out of shape. And your legs are heavy.
Two Reasons One Flight of Stairs Is Cake and Five Flights Practically Drop You
Lack of training. Quite simply, one reason a single flight of stairs is easy yet several are difficult is the same reason you can run hard for 25 yards — but a few seconds beyond that you suddenly have to stop (unless you’re trained in prolonged fast running).
Or, to put it another way, you can kangaroo hop across your bedroom but can’t maintain this for 50 yards.
Walking up a flight of stairs is similar to fast running or bunny hopping in that some of the action is power based – drawing upon fast twitch muscle fibers.
Long duration aerobics such as jogging, fast walking and even a Zumba class are slow-twitch muscle activity. They’re endurance based.
You may be used to jogging, pedaling, mountain biking or doing Zumba for an hour straight, doing these on a recurring basis – recurrent enough to have developed a training effect that allows you to sustain these activities. It’s called specificity of training.
But when’s the last time you trained at stair climbing? You do it only when you have to. This won’t produce a training effect.
Even if you have a staircase in the house, when you use it it’s only for one time, and then you’re walking around on a flat floor or even sitting afterwards.
Too much time lapses in between use of the house stairs to acquire a training effect.
Mechanics. The human body is designed to walk on level ground and even slight grades. Steps were invented by man, not nature.
It’s not a natural movement for us, even though we can train to climb dozens of flights nonstop.
When we walk, do Zumba or run, our feet are not pushing upward off of anything. Our movement is horizontal.
Walking up a staircase involves a degree of verticality. There’s increased hip and knee flexion as we raise a foot to place on the next step up.
And then from that flexed position, we have to push up our body weight.

Freepik.com, jcomp
This also engages more of the buttocks (gluteus maximus), which is a large muscle that’s being put to work in a way that it’s not accustomed to because you use a staircase only when you have to.
Why is climbing multipls flights of stairs still difficult for those who participate regularly in step aerobics classes?
Because in step classes, the stepping upward is being constantly interrupted by a step downward.
When you go up a staircase, there is no interruption in the effort. You’re continously pushing off of steps.
If you do sustained stepping on a 12 inch exercise stool, you’ll still find it challenging to effortlessly go up that fourth and fifth staircase for the same reason:
During stool stepping, every step that’s completed by both your feet is followed by a step down with both feet.
Training Your Body to Breeze up Five Flights of Stairs

Freepik.com
It’s simple: Walk up five flights or a very long outdoor staircase. Then go back down, rest for a few minutes or so, and repeat. Do this twice a week, or, if you do it only once a week, do five sets.
• Make each step count.
• Do not drag yourself up.
• Keep erect and as perky as possible.
• Slow down when you must.
• Don’t start out too quickly.
• Find the pace that allows you to complete five flights without pausing to catch your breath, yet at the same time, provides a challenge.
• If you smoke, quit.
• If you’re overweight, set a weight loss goal.
A lean person can still struggle with stairs for the reasons mentioned above, but carrying 50 pounds of excess fat will make the struggle even worse.
No access to multiple flights of stairs?
You can go up and down your home’s staircase if you have one for 10 minutes straight, going down as quickly as you can to minimize this rest time.
Another option is to hold light hand weights during this workout.
If you don’t have a staircase, you can do stepping drills on a 12 inch stool and sustained walking lunges.
Believe it or not, using a treadmill incline without holding on still won’t do much to make climbing five flights of stairs a breeze.
Though this is a great aerobic exercise, it’s not specific to climbing steps.
A typical hiking trail isn’t the answer, either, because most staircase angles range from 25 to 37 degrees.
Let’s face it: There’s just no substitute for training on multiple flights of stairs if you want to be good at climbing multiple flights of stairs.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.