Can Multiple Sclerosis Cause Toe Pain? What Really Is MS Pain?

If you have multiple sclerosis and toe pain, or if you have unexplained toe pain but have not yet seen a neurologist, there are several important factors that you need to understand. (more…)
Can MS Be Caused by a Car Accident?

Why does multiple sclerosis seem to develop soon after a car accident?
Does the car crash directly cause MS or does it trigger something that’s already there and just make it more noticeable? (more…)
Benign Muscle Twitching vs. MS Twitching: the Differences

There are differences between benign muscle twitching and the twitching muscles of multiple sclerosis.
When a twitching muscle evokes fear in a person, that fear is usually over ALS, a fatal motor neuron disease that can cause what are known as fasciculations.
However, some people’s health anxiety is more tuned in to multiple sclerosis.
MS certainly affects the muscles, but — are fasciculations or any kind of “twitching” muscle action a common part of this autoimmune disease?
Does MS Really Cause Twitching Muscles?
Though MS is well-known to cause muscle spasticity, you should not confuse spasticity (continuously contracted muscles that leads to stiffness) with twitching – that undulating sensation that worms are squirming just under the skin.
Or, to put it another way, think of the type of twitching that occurs in an eyelid happening in a large muscle such as in the leg.
“Muscle fasciculations are not a common symptom of MS,” says Mitzi J. Williams, MD, clinical neurologist with Morehouse School of Medicine, an MS specialist and clinical advisor for the Multiple Sclerosis Foundation.
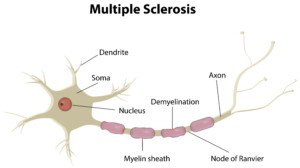
“MS is a disease of the central nervous system which includes the brain, spinal cord and optic nerves,” continues Dr. Williams.
Shutterstock/joshya
“There are other diseases such as ALS which affect the peripheral nervous system (nerves once they exit the brainstem or spinal cord).
“Diseases that affect the central nervous system have signs of ‘upper motor neuron disease, and ones that affect the peripheral nervous system have ‘lower motor neuron’ symptoms.
“Fasciculations are generally a symptom related to lower motor neuron or peripheral nerve disease.”
When Muscle Twitching Is Associated with MS
Dr. Williams explains, “If a person has very advanced MS with severe weakness, fasciculations can sometimes occur, but this is rare.”
If MS ever did cause muscles to twitch (not tremor or go into spasm, but twitch as in the eyelid type happening in the arm or leg), would it feel any different than a fasciculation of a benign origin such as physical exertion, excessive caffeine or anxiety?
Dr. Williams says, “There would not be a difference in the way the fasciculations feel.”
You cannot say, “Gee, the twitching feels like (fill in the blank), so therefore, I must have (or not have) MS.”
As far as concurrent issues that would likely be present with muscle twitching from MS, Dr. Williams explains, “The associated symptom would be advanced stage MS with severe weakness and muscle atrophy or shrinkage.”
There is no difference between benign twitching and that from MS as far as triggering agents such as movement, body position or exposure to an environmental stimulus.
Dr. Williams also points out, “There is not much research on the frequency of fasciculations with MS vs. other conditions because they are so rare with MS.”
This is absolutely true. Also keep in mind that sometimes, the term “twitching” is interchanged with spasm.
However, a spasm is not the same as that wormy, squiggling and undulating sensation just under the skin.
A spasm is something you might see in a person with severe cerebral palsy, in which a limb will involuntarily jerk or jump.
Spasticity is not a spasm, even thought the words sound similar. Spasticity is common in MS, and as mentioned, is when a muscle is in a continuous state of contraction.
Another descriptor that comes up as far as MS is clonus. This is a jerking of the muscles (similar to what happens to healthy people just as they’re falling asleep), but clonus is not another term for fasciculation.
When Muscle Twitching Is Prevalent with Multiple Sclerosis
There may be another problem going on if a person with MS is also experiencing a lot of muscle twitching.
The patient may actually have two conditions: multiple sclerosis and something else causing the creepy crawly fasciculations.
It’s entirely possible for MS and ALS to coexist in the same patient. However, this is very, very unusual.
Not too many cases are described in the medical literature. Dynes et al (ALS, 2000) reports the case of a woman, 62, who developed both MS and bulbar ALS.
Hader et al (Canadian Journal of Neurological Sciences, 1986) describes the case of a man, 56, who suffered from MS, followed by ALS which included body and tongue fasciculations.
In summary, MS as a cause of twitching muscles is a very uncommon occurrence, and when it does happen, it’s in the advanced stages of this disease.

Dr. Williams is author of “MS Made Simple: The Essential Guide to Understanding Your Multiple Sclerosis Diagnosis.” She is a member of the American Academy of Neurology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Orawan Pattarawimonchai
Sources: tandfonline.com/doi/abs/10.1080/146608200750139837
cambridge.org/core/journals/canadian-journal-of-neurological-sciences/article/concurrence-of-multiple-sclerosis-and-amyotrophic-lateral-sclerosis/960A54B59F5357036C3E1877886772C8
What Is a Plethoric IVC?

A medical report might say that the patient has a “plethoric IVC.”
Here is a full description in plain English of what a plethoric IVC is and what causes it.
“The heart is a pump,” begins George Ruiz, MD, former chief of cardiology at MedStar Union Memorial and MedStar Good Samaritan Hospitals, with expertise in the care of adults with advanced heart failure, pulmonary hypertension, congenital heart disease and heart disease during pregnancy.
Dr. Ruiz continues, “As a pump it does two things – (1) fills and (2) pumps blood forward. Any problem with either of these vital functions may lead to heart failure.
“As a result of difficulties filling and pumping, the pressure in the heart increases, leading to a ‘backup’ of pressure throughout the system that drains into the heart.
“The IVC, also known as the inferior vena cava, is the drainage system for all blood returning to the heart below the diaphragm.
“If the heart fails, the pressure/blood backs up, leading to enlarged/engorged veins – the IVC is one of them.”
What exactly is heart failure?
Heart failure is NOT a heart attack and it’s not when the heart stops beating.
It’s when the heart either fails to fill with an adequate amount of blood to be pumped out (diastolic heart failure), or, the heart actually fills with an adequate amount – but the pumping action is poor (systolic HF).
The enlarged or engorged veins (too much fluid in these vessels) may be visible through the abdominal skin.
The engorgement may also affect veins near the anus, twisting and swelling them, leading to hemorrhoidal bleeding with bowel movements.
Another name for plethoric IVC is congested IVC. There may or may not be fluid buildup in the legs with this situation.
“Basically, it means that the patient has evidence that they are holding onto extra fluid,” says Dr. Ruiz.
“This is found on an echocardiogram study – an ultrasound study of the heart and vessels.”
A physician is able to look at the ultrasound image and identify the abnormality as a plethoric inferior vena cava.
This is a life-threatening condition, particularly in people over age 80, a sign of very poor cardiac function.
In the very elderly with longstanding systolic heart failure, a plethoric IVC signals a very dismal prognosis.
 Dr. Ruiz has also treated patients with congenital heart disease and heart disease during pregnancy. From 2006 to 2007 he served as a White House Fellow and was a special assistant to the Secretary of Veteran Affairs.
Dr. Ruiz has also treated patients with congenital heart disease and heart disease during pregnancy. From 2006 to 2007 he served as a White House Fellow and was a special assistant to the Secretary of Veteran Affairs.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dragana Gordic
Can a Baby Get SIDS from Sleeping with Blanket Over Face?

If you’re worried that your infant might get SIDS, here’s why you need to keep the blankets and pillows away from your baby’s face during sleep.
“A baby can suffocate and die if sleeping with a blanket over the face,” says Dr. Lisa Lewis, MD, a board certified pediatrician in Fort Worth, Texas, and author of “Feed the Baby Hummus, Pediatrician-Backed Secrets from Cultures Around the World.”
My Baby Doesn’t Mind Loud Noise: Is this Hearing Loss?

Some babies don’t flinch or seem uncomfortable in loud environments, and parents may think this means their baby’s ears won’t be harmed by the noise, or that perhaps there’s already hearing loss. (more…)
13 Year Old’s Chest Hurts when Inhaling: Possible Causes

Here’s what to do if your 13 year old’s chest hurts upon inhaling, and what the possible causes are including a heart problem. (more…)
All the Smells a Baby’s Poop Has and What They Mean

Baby poop smells different than that of adults, and there are different kinds of odor that a baby’s bowel movements can have. (more…)
Baby Poop Dangerous Color Guide by a Pediatrician

The color of your baby’s poop says a lot about their health.
Certain colors and even textures mean potentially serious conditions that need prompt medical attention. (more…)







































