Why Parents Should Try to Get Their Kids to “Like” Them

There are reasons a parent SHOULD worry whether or not their kids like them.
Trying to be “popular” with your kids is shunned by many parents. But this may be a matter of semantics – the choice of the word “popular” or “like.” (more…)
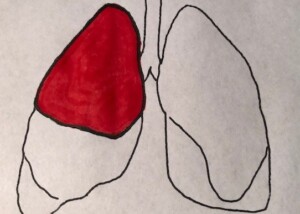
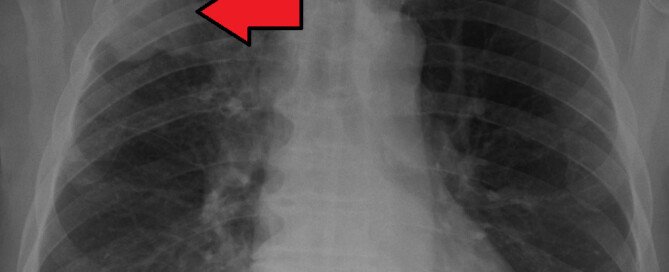
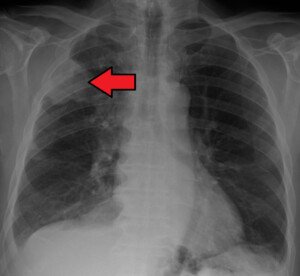
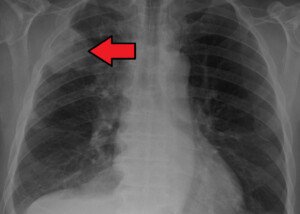
Shortness of Breath from Heart Disease vs. Lung Cancer
Shortness of breath can be caused by heart disease as well as lung cancer, but is there a difference in how feeling short of breath feels between these two very different conditions? (more…)
My Daughter Wants Her Face Moles Removed: What Should I Do?
Has your young daughter come to you asking to have all the dark little moles on her face removed so she could have the “perfect” skin of models? (more…)
How Many Never-Smokers Who Exercise Get Lung Cancer?
Most fitness enthusiasts don’t smoke, and most smokers aren’t into serious exercise. (more…)
Sudden Stabbing Pain in the First Few Toes: Nerve Disease
Nerve related disease is likely what’s causing your sudden stabbing pain in the first few toes.
The pain could be enough to make you stop what you’re doing and grab the toes. (more…)
Numbness Between Big and Second Toe from Flip Flops
If you think your flip flops are actually causing numbness between your big and second toe, you are not imagining this.
Can Diabetes Cause Wet Sweaty Feet?
Do you suffer from wet and sweaty feet and also have diabetes?
There is a real possible connection between sweaty grubby-feeling feet and diabetes.
“In certain diabetic patients, because of the development of peripheral neuropathy, the sweat glands of the patient’s feet may begin to not work properly,” says Dr. Velimir Petkov, DPM, surgeon and sports medicine specialist of the foot with Premier Podiatry in Clifton, NJ.
“Therefore, those patients tend to suffer from either extra dry skin and cracking on one end, or extra wet sweaty feet (a.k.a. hyperhidrosis) on the other.”
Excessively sweaty feet from diabetes is not caused by poor foot hygiene, though poor foot hygiene can worsen the problem.
Letting the sweat accumulate and moisten socks, and then not changing the socks when you should or wearing dirty socks, will not only make your feet feel uncomfortably grimy and grubby, but can cause foot odor that’s noticed by other people in the room.
“Unfortunately, at this point in time, the only way to manage these patients is to treat the symptoms, as medicine has not quite discovered how to treat the underlying cause apart from just controlling one’s blood glucose levels,” says Dr. Petkov.
Managing Sweaty Feet
“In diabetic patients with dry skin (the majority of patients), the treatment is the application of a special moisturizing cream which tends to hydrate the skin.
“In those patients that tend to have more wet and sweaty feet, frequent air circulation is often the key.
“Changing the socks frequently as well as the application of anti-fungal cream as well as anti-fungal shoe spray can often manage the symptoms of hyperhidrosis.”
Whatever type of shoe you often wear, you should have two or even three pairs, so that they can be rotated.
This will prevent moisture and odor from building up in any one shoe over time. This is particularly important if you wear the same footwear every time you exercise (and sweat).
Rinsing your feet every day with soap and water (in addition to your bathing routine) will also help, in that if your feet start sweating really badly later on, at least you’ll know they’re clean.
Since diabetic neuropathy can numb feet, it’s important to check them daily for any cuts or wounds that you might not be able to feel, to prevent infection.
 Dr. Petkov diagnoses and treats numerous ailments related to the lower extremities, and has special interests in sports medicine, wound care and the most advanced minimally invasive procedures for plantar fasciitis and Achilles tendonitis.
Dr. Petkov diagnoses and treats numerous ailments related to the lower extremities, and has special interests in sports medicine, wound care and the most advanced minimally invasive procedures for plantar fasciitis and Achilles tendonitis.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Elvira Koneva
Can a Normal Mole Be All Yellow?
An ALL YELLOW mole? Is this possible, and if so, could it mean melanoma?
Awareness campaigns for the deadly melanoma need to keep rolling out, because this deadly disease can be discovered in its early stages by the patients themselves via home skin exams.
As a person becomes habituated to checking their moles and other areas of skin on a monthly basis, they may sooner or later discover what appears to be a yellow mole.
Not a bright yellow like a lemon, but more like a dull, dingy yellow.
Can a Normal Mole Be All Yellow?
“Most moles are tan-brown, skin colored, or pink in color, although they may less commonly appear with a yellow hue,” says Emily de Golian, MD, a board certified dermatologist with Forefront Dermatology in Atlanta, GA.

But what you think is a yellowish mole is probably not a mole at all, and it also probably isn’t melanoma, since this cancer usually presents in the following colors: black, brown, purple, blue, maroon, red, pink, grey, flesh colored and even milky white.
“Bumps on the skin with a yellow hue are more likely to represent a different type of growth, including sebaceous hyperplasias, which are benign enlarged oil glands that commonly develop on the face [shown in top image]; nevus lipomatosus, which is a benign growth containing fatty tissue; epidermal cysts; milia, and xanthelasma,” explains Dr. de Golian.
Generally speaking, yellow is not a scary color for a skin lesion
 Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can a Skin Cyst Ever Turn into a Melanoma?

Nodular Melanoma
If you’re wondering if a skin cyst can ever turn into a melanoma, this is a very fair question.
Are Moles that Stick Up More Likely to Become Melanoma?

Intradermal nevus. Credit: Dr P. Marazzi/Science Source
Do you have a mole that sticks up more than the others, or maybe it’s the ONLY one that’s raised, and melanoma has barged into your mind?
There are a few things to consider if you’ve come to notice that a mole sticks up more (elevation) than the others.
“Moles that stick out are not more likely to become melanoma; they are simply a type of mole known as an intradermal nevus,” says Emily de Golian, MD, a board certified dermatologist with Forefront Dermatology in Atlanta, GA.
“The raised appearance of these moles is simply due to the architecture of the mole cells in the skin, and this architecture is unrelated to the potential of those cells to become atypical.
“In fact, scientific research indicates that nearly three-fourths of melanomas arise in previously normal skin, not from pre-existing moles.
“Of course, all moles should still be examined regularly for changes.
“However, new brown, black, asymmetrical or growing spots on the skin should be evaluated as well.”

This is a nodular melanoma. Note how similar it looks to the benign mole at the top of this article. This is why any new or “What is that?” growth needs to be examined by a dermatologist.
The Mole Sticks Up – When It Used to Be Flat
This is the second consideration.
A mole that has always been raised, as Dr. de Golian pointed out, is normal and not more likely than any common flat mole to undergo a malignant transformation.
Plus, if you’ve only begun inspecting your skin for just the past few years, and thus, your discovery of that raised mole is only a few years old – what’s very reassuring is if over that time period, the mole’s appearance has stayed the same in all respects (color, size, border).
However…what if you know with absolute certainty that a mole that’s now sticking out — was previously flat?
What can make a previously flat mole become raised?
Trauma to the mole that caused bleeding can make it appear elevated from the collection of old blood on top of it. Do not pick at it.
Another explanation is that the newly raised spot was never a mole; it could be, for example, a harmless skin tag that has mimicked the appearance of a light colored mole due to its difficult-to-view location, and now it’s gotten bigger.
Moles that Are Raised … but not the Intradermal Type
“If a previously flat mole is now raised, this may be normal depending on age,” says Dr. de Golian.
“Most moles are flat in children, and as the moles mature, they sometimes (but not always) raise up into small bumps as we age, typically through the teens, 20s and perhaps early 30s.
“For patients in their early 30s or older with newly raised moles or moles with other changes, this may be suspicious for atypical cells and should be examined by a dermatologist.”
 Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
Dr. de Golian focuses on the surgical treatment of skin cancer via Mohs surgery, cutaneous oncology (melanoma and basal cell carcinoma), surgical defect reconstruction and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.