Negative Mammogram, Dense Breasts: Still Scared You Have Cancer?
So you continuously worry that your negative mammogram missed cancer because you have dense breasts? (more…)
Can a CT Scan Miss Prostate Cancer?

A “negative” CT scan for prostate cancer isn’t anything to get too hopeful about because a CT scan can actually miss prostate cancer. (more…)
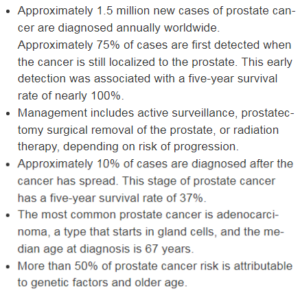
Why Even Early Prostate Cancer Is Potentially Deadly
Don’t be fooled that an early, slow growing prostate cancer is nothing to worry about and can’t be deadly.
Don’t let the relative lack of publicity regarding prostate cancer trick you into believing that this disease isn’t as deadly as breast cancer.
You’ve probably heard the term “slow growing” when the topic of prostate cancer comes up.
You might even know a man who’s been diagnosed with prostate cancer — but his surgery is scheduled for several months out. Don’t be deceived. This is a deadly illness for many patients.
Prostate Cancer May Grow Slowly, But…
“Most prostate cancers grow relatively slowly and develop over years,” begins Jonathan W. Simons, MD, President and Chief Executive Officer of the Prostate Cancer Foundation, David H. Koch Chair.
“However, at some point these tumors often become exponentially more aggressive and gain the ability to spread and metastasize,” continues Dr. Simons.
The spread can reach the bones and other organs, even the brain.
Yes, this cancer can get into the bones and brain tissue if not treated in time.
“Some men develop tumors from the start that are rapidly growing that are prone to metastasize,” adds Dr. Simons.
“Therefore, early detection is critical to intervene while the disease is still localized to the prostate and potentially curable.”
Symptoms of Prostate Cancer
• Frequent urination or the feeling to urinate but nothing comes out.
• Trouble with initiating urination.
• Weak urine stream.
• Pain or burning when urinating.
• Impotence or painful ejaculation
• Blood in the semen or urine
• Rectal pain or pressure

Shutterstock/Chinnapong
• If the cancer has spread to the bones, the patient may feel pain in the back, pelvis or legs. The key to survival is to catch this disease when it’s early.
Yearly PSA values and a complete exam are crucial, no matter how fit and healthy a man believes he is.
Conclusion
When caught early, the cure rate for prostate cancer is excellent — far better than when it’s caught at a later stage.
Early detection significantly improves treatment outcomes.
With prompt intervention, many patients achieve successful management of the disease and maintain a high quality of life.
Men should not feel embarrassed about seeing their doctor for concerning symptoms that could indicate prostate cancer.
Symptoms such as difficulty urinating, frequent urination or blood in the urine should prompt a medical consultation.
Healthcare professionals are experienced in addressing sensitive issues and provide a supportive environment for discussing symptoms.
Prostate cancer screening, including PSA tests and digital rectal exams, can detect the disease at an early stage when treatment options are most effective.
 Dr. Simons is an internationally recognized physician-scientist, oncologist and acclaimed investigator in translational prostate cancer research. Prostate Cancer Foundation.
Dr. Simons is an internationally recognized physician-scientist, oncologist and acclaimed investigator in translational prostate cancer research. Prostate Cancer Foundation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Period After 14 Months of No Period: What Can This Mean?

You’ve gone 14 months without menstruating, when suddenly, you begin feeling crampy, bloated, and here comes the blood — just like any period you’ve ever had.
- How can this be?
- Cancer is something that will resonate in the minds of many women who seem to be having a period when they thought they had completed menopause just a few months before.
Menopausal Timeline
“By definition, menopause is no period for 12 months, so any bleeding after this period [even 14 months] should be immediately evaluated to rule out cancer or precancerous conditions,” explains Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
Causes of Bleeding only a Few Months After Menopause Ends
Most cases of bleeding 14 months (or any number of months) after the completion of menopause are benign. The estimate for this is around 60 percent.
“Other causes are atrophy or thinning of the lining [of the vagina], making it bleed easily,” continues Dr. Riobe.
Intercourse and even an internal pelvic exam can trigger this bleeding, though it may also occur spontaneously.
Vaginal atrophy may present with only dryness, but there can be occasional faint blood appearing on one’s panties.
There may also be burning during urination, and sex may be painful.
The spontaneous “bleeding” from vaginal atrophy is very faint and subtle unless there’s been some kind of physical trauma to the thinning and vulnerable vaginal lining – such as what happens during intercourse.
The blood from vaginal atrophy won’t necessarily show up immediately after menopause ends, because as time goes on during the postmenopausal period of time, the vagina becomes drier.
Abstinence will exacerbate the problem because this promotes increased tightness.
“Infection of the lining of the uterus can also cause bleeding — this is called endometritis,” says Dr. Riobe. “Hormone imbalances can also cause bleeding.”
Cancer
Vaginal bleeding after one goes 12 months without a period and has a confirmed completion of menopause can be caused by uterine, cervical, vaginal or vulvalar cancer.
Cervical, vaginal and vulvalar cancer are strongly tied to the HPV virus.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dreamstime Tadija Savic
Nipple Discharge in One Breast in 15-Year-Old Girl: Cancer?

No doctor will ever say that 15-year-old girls never get breast cancer.
It’s actually possible for breast cancer to strike a 15-year-old girl.
However, the likelihood of this occurring is so incredibly low that the National Cancer Institute Surveillance, Epidemiology and End Results Program determined that the number of new breast cancer cases in females under age 19 for the years 2010-2014 was zero percent.
But zero percent on a graph does not mean never possible or that it’s never happened. It has happened.
But these are truly exceptionally rare cases — rare enough that they don’t register on the NCI’s graph.
Benign Lumps in Teens
“Benign breast tumors can occur in young girls,” says Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
Do not let the term “tumor” scare you. A tumor is simply a mass — which can either be benign or malignant.
If something has been identified as a benign tumor, this does not mean that it’s likely to one day become malignant.
“Fibroadenoma is a more common benign breast tumor in younger women,” notes Dr. Riobe. Cancer is much less likely at this age.”
Fibroadenomas most commonly occur between the ages of 15 and 35.
The way this lump feels to the fingers may be rubbery or as hard as a marble.
Usually such a lump easily moves under the skin with the fingers (a reassuring sign that it’s probably not cancer) and is painless.
“Nipple discharge can be a sign of a pituitary tumor [prolactinoma] in the brain causing prolactin to be secreted. These tumors are usually benign,” continues Dr. Riobe.
“Birth control pills can cause nipple discharge as can other medications.”
Birth control pills can occasionally lead to nipple discharge as a side effect, primarily due to the hormonal fluctuations they induce.
These pills commonly contain a combination of estrogen and progesterone, which can significantly alter hormone levels and subsequently impact breast tissue.
The hormonal changes brought about by these medications can stimulate the milk ducts in the breasts, leading to discharge.
This phenomenon occurs because the synthetic hormones in birth control pills can mimic the natural hormonal fluctuations of the menstrual cycle, affecting the breast tissue similarly to how it would be affected during pregnancy or lactation.
As a result, some women may experience a discharge from the nipples.
It’s important to note that this side effect is generally benign and not usually a cause for concern.
The discharge often becomes more noticeable when there are fluctuations in hormone levels or as the body adjusts to the medication.
If the discharge is persistent, accompanied by other symptoms, or causing significant discomfort, it’s advisable to consult with a healthcare provider to ensure that it’s not indicative of a more serious condition.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Cookie Studio
Source: seer.cancer.gov/statfacts/html/breast.html
Cause of Really Bad Underarm Odor Right Before Period

Do your armpits get really stinky right before your period and you dread going to work and social situations?
Even if you’ve managed to find a strong deodorant that actually masks this problem, having really stinky underarms right before menstruation is a troublesome, though benign, problem.
The smell could be so bad that if the sufferer is standing in the wind, the breeze could actually blow the odor into her face.
Or, she may enter a room and suddenly smell it — because she had just been in there exercising.
And all along, she’s been showering. washing her armpits and wearing clean clothes — but the odor comes on as long as menstruation is about to begin.
Cause of Stinky Underarms Right Before Your Period
“This is a sign of accumulating toxins and poor liver detoxification,” notes Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
Dr. Riobe continues, “This can also be a sign of hormone imbalances such as estrogen dominance from low progesterone.
“Poor diet can also cause bad underarm odor.”
Natural Solutions
• Quit smoking. Smoking causes enough of a bad stink without mixing in with armpit odor.
If you want a de-stressor, you’re better off having a donut than a cigarette.
But ideally, you’ll want to take a brief but very brisk walk to dissolve stress, or listen to your favorite music.
• Have a glass of homemade lemonade sweetened with Stevia every day. Lemons help detoxify.
• Limit your intake of processed foods.
• Take up intense strength training. Intense weightlifting shifts the estrogen-progesterone ratios towards a more progesterone dominant state.

Shutterstock/Improvisor
To help conceal bad underarm odor, first wash them thoroughly with a paraben-free soap.
Don’t scrub with harsh bristles. Instead, you can use a soaped-up sponge and just smear the lather onto your armpits.
Rinse thoroughly, then make sure they are completley dry, and then apply a deodorant.
One more thing you can do to help curb smelly underarms that occur right before menstruation is to work a quarter teaspoon a day of nutmeg into your diet. This spice is good for the liver.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
.
Top image credit: Shutterstock/Aaron Amat
Can Menopause Cause the Urge to Pee to Wake You from Sleep?
Are you wakened at least twice during sleep by the urge to urinate and are wondering if menopause is the cause?
Can an Icy Cold Feeling in a Breast Be Cancer or What?

If you find that your breasts suddenly have an icy cold feeling, the thought of cancer may come to mind.
Breast cancer can present with symptoms other than the classic lump. (more…)
How to Brace for a Sleep Apnea Diagnosis & Treatment