
Diabetes can lead to dangerous conditions that cause pain in the calves and overall legs when walking.
Those with type 2 diabetes are particularly vulnerable to an arterial condition, though the risk is still increased by type 1 diabetes.
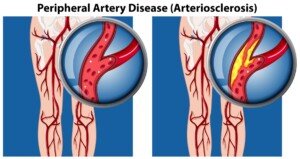
This condition is PAD: peripheral artery disease—also known as peripheral vascular disease. PAD is when there’s plaque buildup in the arteries of the legs.
This is the same plaque or “sludge” that builds up in coronary heart disease, causing the so-called blocked coronary arteries.
Source: vecteezy.com
There are three other conditions—related to diabetes—that can cause pain, aching or cramping in the calves—but first here is information on peripheral artery disease, which can get bad enough to cripple a person.
Diabetes and PAD
Diabetes is not required to develop PAD, but the presence of diabetes (especially type 2) raises the risk.
The reason diabetes increases the risk of peripheral artery disease, which causes pain when walking, is because diabetes causes a higher level of blood fats and raises blood pressure.
These situations can lead to arterial clogging with fatty deposits. The result is blocked, hardened and narrowed arteries in the legs.
“At rest there is no pain, but with activity, there isn’t enough blood flow to the muscles, so there is pain,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
PAD Causes Pain
The pain can be in the feet and toes, not just the calves and upper leg, and will be worse when walking and especially using a staircase.
However, PAD pain isn’t always constant. Sometimes it’s intermittent and is called intermittent claudication.
The discomfort can be in the form of a cramping type of sensation, or that of heaviness or fatigue.
PAD is no picnic. Peripheral artery disease can disable a person and lead to very slow-healing wounds (cuts, scrapes, etc.). The feet may become cold, too.
Ironically, PAD in some diabetics may not produce pain, mainly because the patient also has diabetic neuropathy, which reduces sensation in the legs and feet.
Peripheral artery disease in the diabetic or non-diabetic can also exist under the radar due to a gradual onset.
This gradual onset, or a subtle onset, can masquerade as “normal aging” to some individuals.
Their compensatory behaviors are to shorten the distances they walk (parking closer to store entrances, always using elevators and escalators, taking more sitting breaks when at the amusement park, etc.).
If the patient is older (e.g., 48 rather than 28), they’re likely to shrug this off as a case of “I’m not as young as I used to be.”
Another compensatory behavior is to walk more slowly. They are unaware they have PAD.
Even if they know they have diabetes, it may not occur to them that what’s happening is due to clogged arteries in the legs and calves.
Diabetic Neuropathy
As mentioned, this can reduce sensation and thus, blunt the pain of PAD. But diabetic neuropathy in and of itself can also cause pain.
You can have pain in your legs (although it usually causes pain in the feet),” says Dr. Besser.
If you have diabetic neuropathy this actually raises the risk of PAD. So it’s not just the diabetes that puts you at higher risk of clogged leg arteries, but the neuropathy, which is caused by chronic excess sugar in the body.
Deep Vein Thrombosis
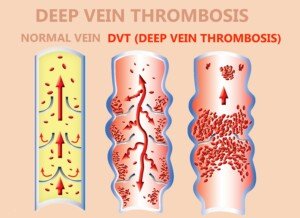
A blood clot in a vein (DVT) can occur to anyone, but many risk factors abound, including diabetes.
A DVT classically presents with pain in a calf, including at rest. There may be associated swelling, redness and warmth to the area.
Shutterstock/Solarisys
A pulled calf muscle, however, typically feels fine at rest and is elicited only upon movement such as walking.
Electrolyte Imbalance
“If your diabetes isn’t controlled, your electrolytes (sodium and potassium) will probably not be normal; abnormal electrolytes can cause cramping,” explains Dr. Besser.
“Muscle strain is due to injury to the muscles (sprain/strain). This pain may also occur at rest if the strain is severe enough.
“There may also be tenderness in the affected muscle and it may be swollen.
“Rest, time and ibuprofen (or similar medications) will treat this but won’t help pain from diabetes related issues.”
Those with type 2 diabetes are particularly vulnerable to an arterial condition, though the risk is still increased by type 1 diabetes.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.

























