Two Big Warning Signs You May Have Nail Melanoma
Yes, melanoma can affect a fingernail or toenail, and there are two major warning signs that what you see is a potentially deadly tumor — also known as subungual melanoma.
What Are All These Tiny Bright Red Dots on My Breast ?
Very tiny, bright red dots popping up over time on the breast can make a woman think this is a sign of breast cancer.
Breast cancer awareness is very important and has ongoing and strong publicity.
More and more women – including younger – are becoming increasingly conscious of this disease and its signs, plus any new changes in their breasts.
So when a woman notices a tiny bright red dot on her breast – and especially if she notices more bright red little spots appearing over the course of time – this can get her heart racing.
“It is important to have a routine skin cancer screening in addition to mammograms annually to verify the cause of these lesions,” says Erum Ilyas, MD, a board certified dermatologist who performs adult and pediatric medical dermatology, cosmetic dermatology and skin cancer treatment with Schweiger Dermatology Group.
Dr. Ilyas continues, “However, the most common reason I see patients for ‘bright red dots’ actually turn out to be angiomas, also referred to as cherry angiomas. These benign lesions are not related to skin or breast cancer.”

Angiomas. Shutterstock/Ocskay Bence
Angiomas, which do not need to be removed other than for cosmetic reasons, tend to come after age 30 and especially after 40. They may be flat or slightly elevated. They are also known as strawberry angiomas.
If one of your parents has a bunch of these tiny red spots, chances are, you will begin noticing them on your own body by the time you reach 40.
They can appear pretty much anywhere where there is skin, including the skin of your breasts.
But here’s what you need to know: An angioma (also known as a hemangioma) is a dermatological situation, not a gynecological one.
What exactly is an angioma?
They are very superficial – and benign – dense masses of very tiny blood vessels, which is why most are “bright” red. They may also appear orange-red and reddish-magenta.
Since this is an issue of the skin, there is no reason why angiomas wouldn’t also appear on the skin that covers a woman’s breasts any less than they would appear on one’s trunk, back, shoulder, neck or arms.
Angiomas, regardless of their location, have no connection to cancer of the breast, skin or any other organ.
As for actual signs of possible breast cancer other than a lump that you can feel, these include puckering of the skin on a breast, an inverted nipple when it’s never been inverted before, a relentlessly itchy nipple, and unusual discharge from a nipple.
If you experience any of these signs, you should make an appointment immediately with your gynecologist.
 Dr. Ilyas has practiced dermatology in the Philadelphia area and Boston for 15+ years and has served as Assistant Professor of Dermatology at Drexel University College of Medicine.
Dr. Ilyas has practiced dermatology in the Philadelphia area and Boston for 15+ years and has served as Assistant Professor of Dermatology at Drexel University College of Medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
.
Top image credit: Shutterstock, Max4e Photo
Mole Removal from the Butt Crack: Pain and Recovery
Here’s what you need to know about removing a mole from your butt crack: if it’s painful and how the recovery goes.
The idea of any procedure that involves the butt crack can cause anxiety in some individuals.
“Removing a mole from the butt crack is no different than removing a mole from another location in most instances,” says Erum Ilyas, MD, a board certified dermatologist who performs adult and pediatric medical dermatology, cosmetic dermatology and skin cancer treatment with Schweiger Dermatology Group.
What’s Involved in Removing a Mole from the Butt Crack
“These are often locally numbed by the superficial injection of a numbing agent that only affects the skin locally,” explains Dr. Ilyas.
“The spot is often scraped or cut out. If small, the base is often cauterized, or if larger, closed with a stitch.”
All removed moles – regardless of reason or location – should automatically be biopsied, even if they appear normal. So make sure that you request that the tissue be biopsied.
“Mole” in a Child’s Butt Crack
Dr. Ilyas explains, “I said ‘most instances’ because it is important to note that in children there can be markers for underlying ‘spinal dysraphism’ which is a group of congenital anomalies that result in incomplete fusion of the spine or its elements such as the bone or neural elements.
“These can present as a midline tag, lipoma (fatty tumor), patch of hair or dimple.
“If a child presents for a lesion in this area we often need to obtaining imaging to verify that there is no underlying concern.”
Recovery from Mole Removal in the Butt Crack
Dr. Ilyas says, “In terms of healing, these do not necessarily have more discomfort associated [than more common areas of mole removal], but can be at a higher risk for infection.
“It is important to maintain proper wound care for preventing these from getting infected.”
 Dr. Ilyas has practiced dermatology in the Philadelphia area and Boston for 15+ years and has served as Assistant Professor of Dermatology at Drexel University College of Medicine.
Dr. Ilyas has practiced dermatology in the Philadelphia area and Boston for 15+ years and has served as Assistant Professor of Dermatology at Drexel University College of Medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/puhhha
Can an Irritated Skin Tag Turn into Cancer?
Skin tags are common and depending on their location are prone to irritation including bleeding.
Can an irritated skin tag, however, actually transform into cancer such as melanoma? (more…)
How Safe or Unsafe Is It to Fly with a DVT?
It is extremely dangerous to fly if you’ve been diagnosed with a DVT in any part of your leg or pelvic area.
How Long Can the AIDS Virus Live in a Tattoo Needle?
Before you head to the tattoo parlor, you should know how long the AIDS virus can live in a tattoo needle.
Remember, tattoo parlors are not medical clinics, so don’t just automatically assume that the one you might be going to is sterile with strict anti-contamination practices.
“HIV can still be active in dried blood for up to six days, but the pH of the environment must be adequate to last that long,” says J. Mark Anderson, MD, DABFM, of Executive Medicine of Texas and who is board certified in family medicine.
“Tattoo parlors can be a place of transmission for AIDS and hepatitis,” continues Dr. Anderson.
“Since a tattoo punctures the skin and causes bleeding, both the tattoo needle and ink can become infected.
“Shared needles and shared ink can be a mode of transmission.
“If you are considering a tattoo, be sure to ask questions about how the parlor sterilizes needles or uses disposables.
“It’s equally important to inquire about the use and reuse of ink.”
Don’t be shy or feel that you will offend the tattooist. At the same time, anyone who wants your business isn’t going to tell you, “We don’t sterilize our needles.”
The best course of action is to gather the names of several parlors and call them with your questions if the idea of asking in person seems awkward.
Trust your gut and make your decision based on how the person over the phone responds to your questions about needle sterilization, disposables and just overall what they do to guard against the transmission of the AIDS virus.
Certainly, if you’re met with a less-than-professional response, you shouldn’t bring your business to that particular parlor.
If upon entering the parlor you don’t like the way it looks or it doesn’t seem clean or sterile — again – trust your gut and find another place to get a tattoo.
The AIDS virus is not to be taken lightly.

Dr. Anderson is coauthor of the award-winning book, “Stay Young: 10 Proven Steps to Ultimate Health,” and host of the nationally syndicated Staying Young Show which goes to podcast as Staying Young Show 2.0.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
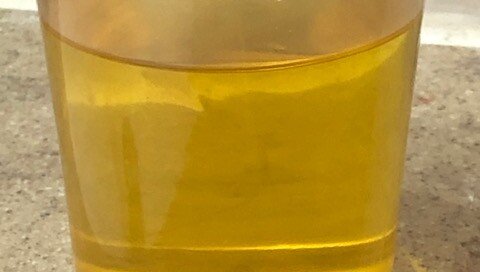
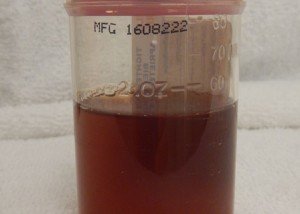
Is Hot Urine a Sign of Disease or Can this Be Normal?
If you’ve ever held a cup of urine after providing a sample in it for your doctor, you will have noticed that the cup was warm.
Or, if your urine has ever streamed down a leg, you’ll recall that it had a warm feel.
• Your skin should feel pleasantly warm.
• If you’ve ever sat in a seat that someone had been sitting in for a while, it’ll be warm.
• In short, the human body is warm, with its normal temperature around 98.6 degrees.
So why wouldn’t something that comes out from inside the body be warm – such as urine? After all, we are warm blooded.
But what about urine that seems more hot than warm?
“Warm or hot urine is normal, especially if a person is cold,” says J. Mark Anderson, MD, DABFM, of Executive Medicine of Texas and who is board certified in family medicine.
Dr. Anderson explains, “Often, when patients have a fever, they may notice their urine is also warmer than usual. That’s because the urine will reflect the core temperature of the body.
“However, if a person experiences burning, it may be a sign of infection and should never be ignored.”
When Urinating Has a Burning Sensation
If it “burns” when you urinate, this isn’t because the urine is extra hot.
It’s because the bacteria from a urinary tract infection have irritated the delicate lining of your urinary tract.
The reason this symptom should never be ignored is because a UTI that goes untreated can lead to kidney damage.
This is because the bacteria can travel up to the kidneys, possibly resulting in permanent impairment.
Another cause of burning, which has nothing to do with any changes in the urine itself, is the presence of anal fissures.
When normal urine makes contact with these irritations in the skin, the chemical makeup of the urine causes a burning or stinging sensation.
“If urine feels hot and there is blood present, seek medical attention immediately,” says Dr. Anderson. This most likely means a UTI that has progressed.

Dr. Anderson is coauthor of the award-winning book, “Stay Young: 10 Proven Steps to Ultimate Health,” and host of the nationally syndicated Staying Young Show which goes to podcast as Staying Young Show 2.0.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Do You Have a Low Resting Heart Rate With No Exercise?
Do you exercise a lot and have a fast resting heart rate, while family members or friends who never work out have a low heart rate?
Though a normal resting pulse is 60 to 100 beats per minute, there have been studies (Copenhale Male Study and Ronald O. Perelman Heart Institute at New York-Presbyterian Hospital/Weill Cornell Medical Center) showing a correlation between the upper levels of normal with an increased risk of all-cause mortality.
• Beta blocker drugs slow resting heart rate
• Caffeine can elevate it.
• But what if that individual who never exercises but has the resting slow pulse doesn’t take any drugs, and the gym rat mountain hiker with the much faster pulse hardly consumes caffeine?
“While most people associate a heart rate with how in shape or out of shape a person may be, heart rate variability can also be influenced by genetics,” says Walter Gaman, MD, FABFM, board certified in family medicine and the author of several award-winning books including “Age to Perfection: How to Thrive to 100, Happy, Healthy, and Wise.”
“Research shows that there are 60 different genetic variants that can impact heart rate. This is why some people who exercise regularly and have a decent BMI can still have a relatively high heart rate,” continues Dr. Gaman.
“An autonomic nervous system dysfunction can also be a cause of high or low heart rate. This can be tested at a physician’s office who does autonomic nervous system testing (ANS).
“Most healthcare providers will also perform a thyroid blood test, especially if the heart rate is abnormally high, to check for hyperthyroidism.”
It may be easier to explain why the fitness enthusiast has a higher heart rate at rest than why the couch potato has the enviably lower resting heart rate.
And that reason is anxiety. The workout buff who has no problem running up a flight of stairs holding a vacuum cleaner in one hand may also be suffering from a chronic state of anxiety that runs in the background – kind of like malware that runs in the background of a computer.
The anxiety changes the hormonal environment of the body, resulting in a sitting pulse in the high 80s or low 90s.
But every so often, the anxiety is out of the system, and the RHR may be in the low 70s and even high 60s.
Another explanation is that maybe the exercise enthusiast isn’t as fit as they think they are.
For example, perhaps they can kill it with a heavy barbell, but this doesn’t mean they have a high level of cardiovascular stamina.
If your resting heart rate is usually at the upper end of normal, despite “all the working out” you do, you’ll want to re-evaluate the degree to which you do aerobic exercise. Perhaps you’re inconsistent?
And if you NEVER exercise but have a low resting heart rate, don’t get smug and assume that this is protective against cardiovascular disease.
Every body needs a good workout at least several times a week.

Dr. Gaman is with Executive Medicine of Texas and is with the Staying Young Radio Show 2.0 podcast.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How High Blood Pressure Causes Headaches and Aneurysms
![]()
High blood pressure, not just brain tumors and sinus infections, can cause headaches.
Hypertension can also cause an aneurysm in the brain – a bulging blood vessel that can burst and cause life-threatening bleeding.
First off, high blood pressure (hypertension) is often referred to as the “silent killer.”
Typically it does not cause symptoms. Typically. That’s the key word.
This is why everyone should regularly get their BP measured with a home device in addition to at a medical clinic.
There is no such thing as, “I can’t have high blood pressure because I feel fine.”
High Blood Pressure and Headaches
Now, in occasional cases, high BP can cause symptoms.
“When blood pressure is elevated, it can often cause a flushed face as well as a headache,” says Walter Gaman, MD, FABFM, board certified in family medicine and the author of several award-winning books including “Age to Perfection: How to Thrive to 100, Happy, Healthy, and Wise.”
“While the American Heart Association takes the stance that high blood pressure does not cause headaches, some scientists and physicians around the world disagree.
“When the heart is working too hard it causes the pressure within the blood vessels to increase.
“The top number, the systolic, represents the heart at work, while the bottom number, the diastolic, represents the heart at rest.
“When someone develops high blood pressure it can increase the pressure of the vessels around the skull.
“Those vessels then begin a processes called autoregulation. In some studies, autoregulation can reduce headaches, specifically if the blood pressure was mostly a systolic elevation.
“However, for people with high blood pressure who develop significant headaches, their body may not be regulating the vessels around the brain, thus causing pressure.
“For those people, headaches may be the first sign of high blood pressure.”

Shutterstock/wavebreakmedia
If you’ve been experiencing bad headaches lately, they are most likely of benign origin such as muscle tension, stress or a sinus issue. Even a tight ponytail can cause a headache.
Brain tumors are uncommon causes of headache. Hypertension, too, is not a common cause, but it’s more likely the culprit than is a brain tumor.
Nevertheless, high BP is a heavyweight in the department of potentially life-threatening conditions.
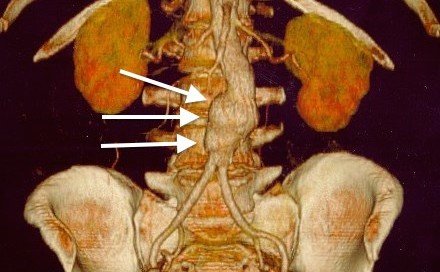
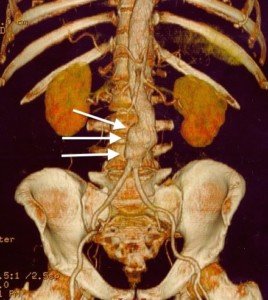
High Blood Pressure and Brain Aneurysm
“Someone with untreated hypertension can be at risk for a cerebral aneurysm,” says Dr. Gaman.
“This is especially true if they also have a history of smoking cigarettes. The uncontrolled hypertension puts pressure on the blood vessel, causing it to become weak.
“Much like a balloon that has been stretched with inflation, deflated and inflated again. Over time, this causes the balloon to lose elasticity.
“The arteries are the same way, becoming weak when over-stretched. If an artery then bursts, it can create a hemorrhage, where blood leaks out into the brain.
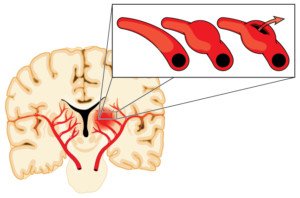
Shutterstock/Blamb
“This is a life-threatening condition. This is one of the reasons that controlling high blood pressure is so important.”
This condition is also called a hemorrhagic stroke. For many who survive this event, they suffer permanent brain damage (depending on which area of the brain got soaked with blood).
Usually, an unruptured cerebral aneurysm does not cause symptoms. However, there are cases in which for a few weeks prior to the rupture, the patient began experiencing headaches.
Beware of this Symptom Triad
A classic symptom trio is highly suspicious for a brain aneurysm:
• Headache
• One eyelid drooping
• Pupils of noticeably unequal size
There may also be double vision. If you’re having any of these symptoms along with a headache, you should be driven to the emergency room.
Though headaches as solitary symptoms normally don’t mean anything sinister, the game changes when the other symptoms are present. Get to the ER!
Avoiding Hypertension
To keep your blood pressure from getting high, here is what you must do.
Quit smoking, increase your consumption of fresh produce, lower your consumption of processed and high sodium foods, maintain a healthy body weight, and do cardio and strength training workouts.

Dr. Gaman is with Executive Medicine of Texas and is with the Staying Young Radio Show 2.0 podcast.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.