New Mole but You’re 60-Plus: May Be Melanoma

If you’ve discovered a new mole and you’re 60-plus, don’t wait to get this checked out by a dermatologist.
If you’re over age 60 you may be noticing new spots arising on your skin on a frequent basis (age spots), but suppose you notice something that appears to be a new mole — as in birthmark or like other moles you’ve had on your body since the day you could remember.
It’s not normal for a person over age 60 to develop a new mole.
A mole is not the same as a sun spot or age spot.
What appears to be a new mole may not be an actual mole (known as a nevus to dermatologists—pronounced “nee-vus”).
That new lesion may be a benign skin barnacle, known as a seborrheic keratosis. Or, it could be melanoma.

Seborrheic keratosis. Shutterstock/
Only a biopsy can rule out melanoma. A “new mole” in someone over age 60 should be biopsied for melanoma.
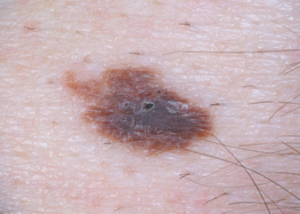
Such a melanoma can progress quickly, as in the case below.

Courtesy of Dr. Gary Goldenberg
“The lesion appeared three months ago and grew rather rapidly,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
Dr. Goldberg explains, “It was slightly painful and itchy. A biopsy was performed and showed a nodular melanoma.
“The patient underwent a surgical excision. Patient is a 68 year old white male who came in with a ‘new mole.’”

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/wavebreakmedia
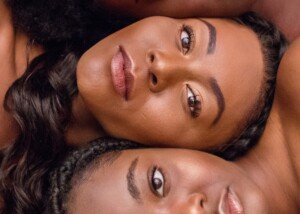
Melanoma in Fingernails: Blacks Not Immune to Skin Cancer

People of color are at higher risk for melanoma (skin cancer) in their fingernails.
Melanoma can arise in the fingernail, or nail bed, and is called acral lentiginous melanoma. Below is a photo of what this may look like.
“The patient is a 42 year old black male with pigmentation of the thumb nail,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“The patient thought that the lesion was caused by trauma and ignored it for over one year.
“The patient presented due to increased pigmentation and pain when using the thumb to perform simple tasks.
“A biopsy was performed and showed a deep acral lentiginous melanoma.
“The patient, unfortunately, required thumb amputation and subsequent chemotherapy.”
Acral lentiginous melanoma is so rare (even in blacks) that most dermatologists won’t encounter it in their professional career.
Melanoma in a nail (which includes toes) may be misdiagnosed as a bruise, fungus or birthmark, and black patients may think it’s benign simply because of their skin tone.
However, a birthmark would have been there since childhood. A fungus will respond to medication, and a bruise will eventually go away when the offender (such as a tight shoe or high heels that compress the toes) is removed.
Beware: Acral lentiginous melanoma can resemble a harmless bruise.
With a bruise that’s underneath the nail, the rest of the finger (or toe) will be normal.
Often, with nail melanoma, it spreads to the cuticle or skin around the nail or behind, and the initial discoloration also spreads.
Acral lentiginous melanoma may also take a straight line shape from nail bed to tip of nail.
It’s normal to develop dark brown or black “streaks” or “slivers” in the nail. In the case of ALM, it’s thick (does not look like a “sliver”) and looks more like a band.
Blacks not Immune
Do NOT avoid getting a biopsy just because you think you’ve convinced yourself that the new symptom is just a bruise or benign streaks or slivers.
Blacks (plus other dark skinned individuals and Asians) are more likely to develop melanoma in the nails than are whites.
Don’t wait; have a dermatologist take a biopsy to rule out anything serious. Chances are it’s benign, but why take chances?
Top image: Courtesy of Dr. Gary Goldenberg

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Do ABCDEs Always Apply to Melanoma; Can Cancer Look Normal?
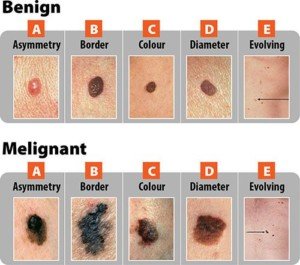
What if a melanoma doesn’t conform to the ABCDE guidelines?
Melanoma can pass as a normal mole simply because there’s always a beginning to this disease process.
In very early melanoma, the ABCDE guidelines don’t always apply.
“Melanoma can have many different looks — the lesions may be black, brown, bluish, red or even flesh color,” Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
A normal mole can be raised. Dr. Goldenberg says that melanoma “can be flat or stick out from the skin surface.
Early melanomas are usually flat, and patients are sometimes surprised that a flat lesion can be dangerous. Early melanomas often look benign (normal) to an untrained eye.”
However, a trained eye can miss a melanoma if the disease is early enough, especially if that trained eye does not know what the mole looked like a month or a few months prior.
The ABCDEs for Melanoma
A = asymmetry. The spot is not equal on either side of a dividing line. However, a normal mole can be asymmetrical, especially if it’s large.

An asymmetrical mole, though this is considered an atypical mole. Source: Biophoto Associates/Science Source
B = border. The border is jagged or erratic. Again, a normal mole can have this feature.
C = color. A normal mole can be any shade of brown, even black, and may even appear purple or blue due to minute vascularity underneath.

Blue mole. Dannii Brighton, CC
D = diameter. A normal mole can be larger than a pencil eraser, and a melanoma that arises in the absence of a pre-existing mole has to start out somewhere: a tiny pinpoint.
E = evolving. This is the key. Has that black mole always been black? Has that “funny” mole always been asymmetrical or had ragged edges? Has that spot on your back always been the diameter of a dime?
“As melanomas progress, they may become more of a bump – that’s called nodular growth phase,” says Dr. Goldenberg.
“These are the most dangerous lesions, since they grow into the skin and can spread to other organs.”
A melanoma is as deep as it is high.
If it’s 2 mm above the skin, it’s 2 mm beneath the skin.
“There is a misconception that a mole with hair growing through it is more likely to become melanoma; it’s simply not true.
“This is why I tell my patients to have their moles checked once per year and to see me if there is a new or changing lesion.”

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Is Blonde Hair a Melanoma Risk in a Biracial Person?

Blonde hair (which usually goes with fair skin) is a melanoma risk factor, but what about for biracial people with olive or caramel skin?
How often have you read that “blonde hair and blue eyes” are a risk factor for melanoma, along with “fair,” “pale” or “light” skin?
Certainly you’ve read that dark skinned people have a lower risk for melanoma when compared to light skinned people.
So here’s an interesting question that I posed to Dr. Rebecca Baxt, a board certified dermatologist with Baxt CosMedical:
Is blonde hair relevant as an added risk factor for melanoma in biracial individual?
After all, some biracial people have varying shades of blonde hair as well as skin tones.

“These are questions that we really don’t know exact answers to,” says Dr. Baxter, “as there are no good prospective studies looking at eye color and hair color and parentage and how much skin cancer these populations develop.
“From clinical experience, darker skinned people have lower risks of all skin cancers, but not zero risk.”
An even more interesting question is if blonde hair means an increased risk of melanoma in a very dark skinned individual.
Below are natives of the Solomon Islands who have a gene called TYRP1, which causes blonde hair.
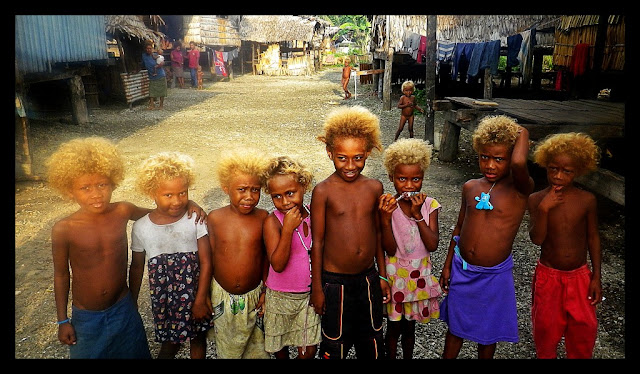
As Dr. Baxt has stated, there is no data on this. Nevertheless, no human is immune to melanoma.
In fact, melanoma can appear in areas that get very little sun exposure, which means that in those cases, the amount of natural melanin (skin pigment) would not play a role.
Plus, biracial people and those with a deeper olive complexion, have been known to get the sun-related skin cancers of basal cell carcinoma and squamous cell carcinoma.
And don’t forget that sun exposure and light skin are not the only risk factors for melanoma, especially the type of tumor that develops inside the mouth, nose or eye.
Genetics do play a role, even in those with dark skin. Researchers also believe there are risk factors not yet discovered.
Dr. Baxt is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, peoplecreations
How Common Is Melanoma Black; Can a Normal Mole Be Black?

A dermatologist discusses how often a mole with melanoma is a black color.
I wondered how common is it that a melanoma lesion is black — not dark brown, but true black. And can a perfectly normal mole be black?
“Yes, normal moles can be black, more commonly in darker skinned individuals,” says Dr. Rebecca Baxt, a board certified dermatologist with Baxt CosMedical.
“Most moles are brown, but some can be pink or black,” continues Dr. Baxt. “Generally, darker skinned people get darker moles; fair skinned people get lighter moles.

“The general rule is if it’s new or changing, it needs to be evaluated by a doctor, preferably a dermatologist.
“If the mole has changed and turned black, that mole needs a biopsy to rule out melanoma.”
Melanoma can definitely appear black (top image and below).


Can a normal mole be black?
“There are other reasons a mole could turn black such as trauma, but melanoma should be ruled out,” says Dr. Baxt.
“Moles can definitely change during pregnancy. They can grow and get darker and they need close follow-up by a dermatologist.
“I always tell my patients to follow up with me more often when they are pregnant and not less often. Self-tanner can make moles look darker temporarily.”
Dr. Baxt is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Image 2 and 3:
CDC, Carl Washington, MD, Emory Univ. School of Medicine, Mona Saraiya, MD, MPH
pcds.org.uk/clinical-guidance/melanoma-an-overview1
Are Many Moles on Dark Skin Still a Melanoma Risk?
You may know that having many moles is a melanoma risk factor, but is this still a risk if you have a dark complexion?
Have you ever seen a person with a dark complexion and a large number of moles, and wondered if having so many moles placed that individual at a higher risk for melanoma?
After all, dark skin is less likely than a light complexion to develop this lethal skin cancer.
Each year, approximately 20,000 to 22,000 Americans die from melanoma, according to the American Cancer Society (2023).
Having many moles is a risk factor for melanoma.
“More moles is generally thought to be a risk factor, as is light skin, light hair, light eyes,” says Dr. Rebecca Baxt, a board certified dermatologist with Baxt CosMedical.
“Darker skinned people tend to get worse melanomas probably due to delay in diagnosis.
“It’s important to check hands and feet, especially in darker skinned individuals.”
There is actually no data that strictly applies to melanoma risk in people with many moles and fair skin, as compared to those with many moles and darker skin tones.
No research is out that gives conclusive information on comparative melanoma risk for dark skinned people who have a large number of moles.
Nevertheless, the comparison is certainly fascinating to speculate about.
Why is this malignancy “worse” in those with dark skin?
Dr. Baxt explains, “No one knows, but when African-Americans for example are diagnosed with melanoma, it tends to be at a later stage.
“We can infer that this might be due to lack of recognition since their skin is darker, or that doctors assume they have a low risk and don’t look for melanoma, or that they have less access to medical care; there is no good answer, just suppositions.
“But the fact is that the melanomas are often diagnosed later, so they have a poorer prognosis.”
In black people, melanoma often appears in less typical locations compared to lighter-skinned populations.
One of the most common areas for melanoma in black people is the palms of the hands and the soles of the feet.
This type of melanoma is known as acral lentiginous melanoma, which, while relatively rare overall, is more prevalent among people with darker skin.
Another area where melanoma can appear is under the nails, in a condition known as subungual melanoma.
This is characterized by dark streaks or spots beneath the nails and can be challenging to detect early due to its subtle presentation.
This stealthy cancer can also occur in mucous membranes, such as those in the mouth or genital area.
These sites are less frequently affected in people with light skin.
It’s simply not known, due to lack of research, if a dark skinned person with few moles is at less risk for melanoma than is a dark skinned person with many moles, even moles in very sun-exposed areas.
Why Is the Prognosis for Nail Melanoma Much Worse than Skin?
Dr. Baxt is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can a Lentigo Turn into Melanoma?

A lentigo can pass as a mole or birthmark; can it ever become a melanoma?
Whether or not a lentigo, which often looks just like a small mole or birth mark, could morph into melanoma, here is what Dr. Rebecca Baxt, a board certified dermatologist with Baxt CosMedical, explains:
“Usually no, but there is a variant of melanoma called lentigo maligna which is basically a lentigo gone bad that grows and becomes a melanoma.

A lentigo maligna. Omar Bari, Philip R. Cohen
“The good news is that these are rarely aggressive; they are usually melanoma ‘in-situ’ [confined to the site of its origin] in its earliest stage, and they grow slowly so there is lots of time to catch them before they become a problem.
“They are most common on the face of older people. If left to grow large, they can be very difficult to remove surgically.”
Dr. Baxt is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
is an assistant clinical professor of dermatology at NYU and a member of the Skin Cancer Foundation. She also specializes in laser treatments, skin rejuvenation procedures, acne treatment and rosacea treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
White Sticky Stuff on Inner Walls of Mouth: Causes

There are several possible causes for the white, slimy and sticky substance that forms on the inner walls of your mouth.
Though experiencing a white, gooey substance on the inner walls of your mouth is a very unpleasant issue, be assured that the causes are not life-threatening.
“Dry mouth is the most common cause of this unpleasant sensation,” Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
If you find that your dry mouth seems unrelated to dehydration, place a small piece of lemon rind between your back teeth and inner wall of the mouth, and it will stimulate salivary gland production.
Other Causes of White Sticky Substance Inside Mouth
Dr. Goldenberg says, “Medical causes also exist, however. A yeast infection in the mouth can cause this sensation — this is especially common in patients with diabetes and those with very weak immune systems.
“An allergy to a food or your dental filling can also be the cause.”
In addition, certain toothpastes or brands can cause a white slimy substance to form inside of your mouth.
However, this would be an immediate result of using the toothpaste, and it will dissipate as the hours pass.
The solution is to find a toothpaste that doesn’t cause this problem.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/farland2456
Itchy Arms and Legs in Winter: Causes & Solutions

A dermatologist explains causes of itchy arms and legs during winter and what you can do about this.
“Winter itch is extremely common,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“It is caused by lack of skin moisture in cold, dry environments. It is particularly bad in patients who suffer from eczema and psoriasis.”
Eczema and psoriasis will cause visible changes to the skin, namely reddish or pink patches, bumps and scales.
Frequent aggressive scratching can cause the area to become crusty and leak fluid.
The itching can be so bad as to temp the sufferer to scratch with a hair brush — up and down the leg or arm. And it feels wonderful — as long as the scratching is in progress.
But soon after the scratching is stopped, the itching returns. There seemingly is no end to this winter itching.
Solutions to Wintertime Itchy Arms and Legs
“There are multiple things one can do to improve dry, flaky, itchy skin,” says Dr. Goldenberg.
“Applying moisturizer is extremely important. There are several products I recommend to my patients, including Cetaphil, Restoraderm, CeraVe lotion, and Kiehl’s Creme de Corps.
“Using a gentle cleanser instead of soap in the shower is also important. The shower should be quick and lukewarm, not hot.
“Using a humidifier in the bedroom while you are sleeping can also be very helpful. Interestingly, drinking more water does not seem to hydrate one’s skin.”
Beware also that wool clothing can make the arms itch, and wool socks can make the legs itch.
To keep warm in frigid outdoor winter air, instead of wearing wool you can try thermal “underwear.”
This thin material, made of polypropylene, is highly effective at insulating the body from very cold temperatures.
And yet one more solution to wintertime itching of the arms and legs is to loosely wrap the most affected areas with Ace bandaging — as this harmless barrier will discourage scratching.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/namtipStudio
Is a Scab that Won’t Heal Always Cancer?

Can a non-healing scab be benign or is it always cancer?
You’ve probably heard for years that one of the classic signs of cancer is “a scab that won’t heal.”
But is a non-healing scab always a sign of cancer?
“A non-healing lesion can be completely benign or could be malignant (cancerous),” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“It really depends on the lesion in question.
“Sometimes something does not heal simply because more time is needed.
“This is especially true in the elderly and on the legs.”
But what if a lot of time has passed and the scab still has not healed?
Yes, cancer can be a cause, but there are a few more benign explanations for why a scab has not healed after a period of time.
One of them is a low grade infection at the site that can be caused by bacteria or fungus.
Another benign cause is repeated trauma to the site that you may not even be aware of, such as a clothing strap or button chafing against the area.
If the non-healing scab is on your face, it’s possible that you’ve been unknowingly traumatizing the area over and over by habitually scratching there or rubbing the area as a stress habit.
If the non-healing lesion is on a leg, have you been unknowingly running a razor blade over the spot when shaving?
Cancer and a Scab that Won’t Heal
Dr. Goldenberg explains, “A more concerning scenario is when a non-healing lesion is a sign of underlying cancer.

A skin cancer that strongly resembles a common scab. Shutterstock/terry meador
“These lesions often ‘try’ to heal, only to scab and bleed again. A bleeding lesion is particularly concerning.
“The way to diagnose the lesion is to have a dermatologist perform a biopsy; this is a procedure in which the doctor will take a piece of skin and send it in for a pathology diagnosis.
“I always advise my patients to see me if they have a non-healing, bleeding lesion, to make sure it’s not cancerous.”


Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.