Cause of a Thick Waist May Be a Popular Ab Exercise …

There’s a good chance you’re doing an ab exercise that actually makes your waist thicker–and is THAT what you want, a thicker waistline?
This exercise builds the sides of your waist if you do it as described in this post. (more…)
How to Do Leg Extensions Correctly for the Best Results
Yes, it’s possible to do leg extensions with poor form vs. perfect form, and great technique makes all the difference in the world. (more…)
Should Elderly People Take Creatine for Muscle Health?
If an elderly person wants to gain muscle, should he — or she — take supplemental creatine?
A study from McMaster University set out to find some answers. The typical elderly person — certainly not those who passionately strength train — has a significantly reduced amount of muscle mass.
Beginning at around age 30, a person will lose five pounds of muscle per decade if he or she does not do any strength training.
The McMaster study was led by Dr. Mark Tarnopolsky, and he found that in elderly people who strength trained, taking creatine in combination with conjugated linoleic acid produced a better result than just the strength training by itself.
The 49 study subjects were at least 65 and did resistance exercise for six months.
- Some of the elderly participants received creatine daily plus the CLA.
- Others were given a placebo.
- The groups did not know whether they were given the creatine or the placebo.
All of the subjects experienced improvements in strength.
However, greater muscle-endurance gains, greater increase in muscle growth and more of a decrease in body fat percentage were realized in the creatine/CLA group. The full report is in PLoS One, 2007.
Natural Production of Creatine in Our Body
The human body produces creatine naturally. It is derived from amino acids, the building blocks of protein.
The muscles use creatine for energy. The food source of creatine, not surprisingly, is meat.
The reason skepticism for supplementation exists is because typically, the athlete consumes two to three times the amount he’d normally get from eating a lot of meat.
It would be intriguing to have a study following people beginning at age 65, for years on afterwards, to see how creatine affects them, in combination with lifting weights.

Shutterstock/Mladen Zivkovic
Are you over 65, have never lifted weights and want to gain healthy muscle?
My opinion, as a former personal trainer, is that you don’t need supplemental creatine to experience increased strength and muscle gain from lifting weights.
What’s more important is:
• Correct form and technique.
• Focusing on compound moves (e.g., dumbbell squat, bench press, barbell row) that target the legs, back and chest, rather than doing a lot of small isolation moves like raising tiny dumbbells straight out in front of yourself, or biceps-curling little dumbbells.
• Adequate nutrition and hydration.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Source: sciencedaily.com/releases/2007/10/071002213425.htm
Why Crunches with a Fitness Ball Will NOT Flatten Stomach

Don’t get your hopes up with that bouncy stability ball and all of those endless crunches; they will not flatten your bulging belly or tighten your abs, and here’s WHY. (more…)
Can You Be Too Old to Get Microscopic Colitis?

As more gets known about microscopic colitis, it’s clear that you can never be too old to get this diarrhea disease–which is often misdiagnosed as irritable bowel syndrome.
Microscopic colitis is considered an autoimmune disease. If someone in the family has it, this is a marker that other family members are at increased risk.
This is why when my 89-year-old mother developed sudden-onset diarrhea (both watery and explosive), I wondered about microscopic colitis—because I was diagnosed with it six years ago.
However, she also has low thyroid! And I’ll get to the significance of that in a moment.
Though the occurrence of sudden-onset diarrhea may seem to contradict the presence of microscopic colitis (since MC is frequently described as chronic diarrhea), keep in mind that in some patients, the onset is sudden, acute.
In my case, one day I just began having loose stools that fell apart in the water when I poked them.
How old is too old for microscopic colitis?
The prevalence of chronic diarrhea in elderly people is not known. My elderly mother was also experiencing sudden urgency and incontinence (normally she has neither).
MC in older adults can present with rectal urgency and incontinence. Medscape.com states that MC “is a common cause of watery diarrhoea, particularly in older female patients.”
The site continues: “MC is a disease that predominantly affects older patients,” and incidence rates range from five to 10 times higher in people over age 65.
Here’s one such references study: Olesen M, Eriksson S, Bohr J, Jarnerot G, Tysk C. Microscopic colitis: a common diarrhoeal disease. An epidemiological study in Orebro, Sweden, 1993–1998. In: Gut (2004) 53:346–50.
Medscape.com says that a Canadian study found that people over 65 were five times more likely to have developed microscopic colitis.
The site lists a slew of study references, but just how old is too old for microscopic colitis has not been determined.
There may be many people out there in their 90s who have microscopic colitis—that has gone undiagnosed, or, for years has been misdiagnosed as IBS-D or stress related (and the latter especially if the flare-ups are intermittent rather than chronic).
Now, about hypothyroidism. Low thyroid is a risk factor, or at least, is an associative factor, in that MC is more prevalent in those with low thyroid than in those without any other autoimmune disorder.
This is a well-established fact, with many studies (referenced on medscape.com) showing this.
As I type this, my mother’s diarrhea seems to be on the way out; she had a normal bowel movement today (after taking Imodium yesterday).
I had taken her to the ER where (not surprisingly), the doctor named only two possibilities for the cause: a bacterial infection or a viral infection.
Her bloodwork came back negative for C. Diff, and apparently, no bacteria were found in her stool sample.
At the ER the doctor never mentioned MC! When an elderly person goes to the ER with complaints of sudden-onset, blood-free diarrhea—and there’s been no travel, no change in eating habits, no new medications—this COULD be microscopic colitis!
Though MC can present with several symptoms, it’s possible for the diarrhea to be the only symptom.
Keep in mind that enteropathic arthralgia from MC can masquerade as age-related joint aches in an old patient—though in my experience with enteropathic arthralgia, it feels identical to the joint aches of premenstrual syndrome!
My mother says she hasn’t had joint aches. MC can come with nausea. My mother had nausea the first day of the diarrhea, then upchucked. Patients with MC have reported vomiting.
They’ve also reported weakness and fatigue. My mother has become markedly weak since the diarrhea began five days ago, but we need to look at other factors.
My mother has lost about six pounds (MC can cause weight loss). Her weight loss is clearly from loss of appetite since the diarrhea began.
Loss of appetite = caloric restriction = weakness and feeling sick when the patient is already only 120 pounds and age 89!
An elderly body responds much faster to a drop in calories from an already-scant diet than if the patient were 45, and that response is a lot of weakness.
In summary, it is not known if a person can be too old to get microscopic colitis, but according to the studies listed on medscape.com, there’s a lot of evidence that this benign inflammatory bowel disease is more likely to strike an older person (especially female) than a younger person.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
.
Top image: Shutterstock/Boryana Manzurova
Source: medscape.com/viewarticle/717156
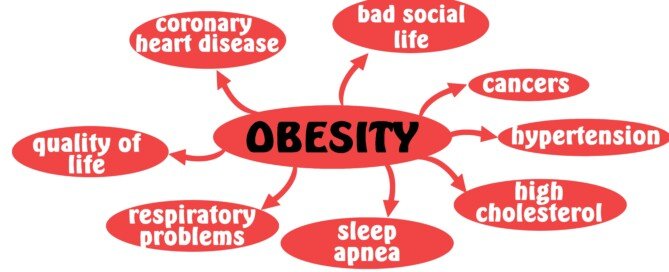
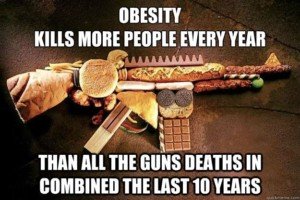
Fat Acceptance vs. Thin Acceptance: Obesity Never Healthy

Would your doctor rather you be fat or thin?
Fat acceptance is wrong on so many levels.
The fat acceptance movement needs to be reversed immediately. Obesity is never healthy.
What is the definition of fat acceptance?
Fat acceptance can mean fat acceptance in the workplace and accommodations made on airplanes, etc.
On the other hand, fat acceptance may mean the encouragement of obese men and women, particularly women, to embrace their bodies, to be “comfortable” with their bodies. And that’s where fat acceptance becomes wrong.
I’m all for fat acceptance in the realm of Hollywood hiring more hefty people, especially women, to fill roles — roles that have nothing to do with being overweight.
I’m also in favor of fat acceptance in high schools, in which overweight kids are not ostracized, and portly mothers can feel they can get involved with their kids’ school activities without worrying that other kids will make fun of the “fat mom.”
But fat acceptance should end where a person’s current or potential health and mobility problems begin.
Frankly, I don’t know how an obese person can be comfortable in a body that gets fatigued easily, that gets exhausted trudging up a staircase, that has difficulty moving swiftly and efficiently.

Fat acceptance is synonymous with smoking acceptance or heavy-drinking acceptance.
Smoking, heavy drinking and obesity are all dangerous to the body.
Rather than give up and resign to accepting your obese body, why not make a permanent commitment to trimming down?
This is not about knocking or criticizing overweight women and men, even though many who read this article will take it that way.
The human body is not supposed to be huge. Being obese was once an anomaly. Now, it’s closing in on being the norm.
In fact, American Sports Data says that 63 percent of America is overweight, and about half those individuals are classified as obese.
Encouraging obese women and men, or even moderately overweight people, to accept being hefty is dangerous.
There are many men and women walking around right now, who are trim and in their best health and fitness ever — who were once obese.
Suppose they had decided to fall for the fat acceptance mindset.
They then would have never lost the weight and got fit and healthy.
But because they refused to accept being overweight, they committed to healthy lifestyle changes.
Just today, at the gym, I was talking to a middle-aged man who was lean and muscular, no pot belly or slumped shoulders.
He said he’d always been into weightlifting, but after becoming a bus driver, gained a wild amount of weight and ballooned up to 308 pounds. He was about 5-8.
Imagine the sorry health he’d be in right now had he, at 308 pounds, fallen for fat acceptance.
I also strongly doubt he would have met his new wife — who was working out with him. I’d say she was pushing 50.
But she had a killer body, ripped arms, tight thighs. They even hit the gym while on their recent honeymoon.
Yes, folks, it CAN be done: A healthier, fitter, trimmer body can be yours by seeing the facts for what they are: Obesity kills.
Saying that obese people can be healthy because skinny people die from heart attacks is like saying it’s safe to swim in shark infested waters because people get killed by alligators.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
.
Top image: Shutterstock/Noiel
How to Choose a Personal Trainer if You’re Obese

Plus size people must know the warning signs when hiring a personal trainer or they’ll waste their money and never lose weight.
Here’s how you can know how to choose a personal trainer.
I’m a former certified personal trainer who’s had many obese and morbidly obese clients.
If you’re very overweight and have decided to hire a personal trainer, here are some warning signs that a particular personal trainer is not right for you.
1. The personal trainer is significantly overweight.
Though on one hand, the very large client may feel that such a personal trainer “knows what I’m struggling with,” ask yourself if this particular instructor knows how to successfully keep excess weight off.
In theory, he or she does. But it will really help the plus size client if the personal trainer shows evidence of firsthand experience with weight control.
This includes a personal trainer who was once “fat” or even moderately overweight, and is now at a healthy weight.
Otherwise, ask yourself why would you want to pay this person to help you lose weight?
At the same time, be aware that a thin instructor may be thin due to youth or an anomalous metabolism, and may have no firsthand experience with adhering to healthy eating or even much exercise.
Choose a trainer who sticks to healthy eating and whose physique indicates commitment to exercise.
Or to put it another way, you can easily picture that person effortlessly shoveling snow and then working out at the gym later that day without a hitch.
Also, a little extra weight on a personal trainer is fine if the bigger picture looks good.
Look at the entire picture; they may be thick in the waist, but how’s the rest of the body?
- Is it strong looking, or out-of-shape looking?
- Muscular (or toned) arms, or shapeless soft arms?
- Perhaps this “solid” trainer can actually do pull-ups or perform jumping routines like a kangaroo.
2. Personal trainers who don’t seem comfortable answering a lot of your questions…
…and seem to have a one-size-fits-all response to why you’re obese. Multiple factors contribute to obesity; though, in my professional opinion, the mainstay in obesity is too much processed food and incorrect workout approaches.
A good personal trainer will ask the prospective overweight client about sleeping habits, any diagnosed medical conditions and what kind of exercise the individual has already been doing that isn’t yielding desired results.
3. A personal trainer whose very plus-size clients do strange, oddball routines.
These routines appear to be more of an attempt to get the attention of other gym members (and possibly more clients).
I once observed a personal trainer have his obese, middle-aged female client standing on a very unstable wobble board, while at the same time she was pulling the handles of a pulley machine towards her.
The resistance was to pull towards her chest. She was so unsteady on the board that she had trouble pulling the handles towards herself, and eventually fell off the board and onto the floor!
The very heavy person should observe how personal trainers work with their clients of all sizes.
Funky-looking drills, moves that require strange balancing acts, one-footed hopping and other unconventional routines, should be red flags.
These have not been proven by science to be more effective than traditional exercise at burning fat or improving fitness and health.
4. Personal trainers who engage clients in conversation while the client is performing the routine.
An obese person needs to focus on good form and good breathing habits.
This won’t happen if the client is enmeshed in socializing while doing the exercise.
If you have a lot of weight to lose, there is a personal trainer who is just right for you.
Shop around and be patient in your search. Don’t feel you must hire the first instructor you see.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/New Africa
THIN BUT BIG BELLY? 4 Exercises to Flatten Your Stomach

You don’t have to keep suffering with spindly arms and legs and a big belly any longer!
Pay attention very carefully, because I’m about to tell you something that’s the opposite of what you probably believe when it comes to flattening the stomach. (more…)
Preparing for a Strenuous Hike: Be Ready, Not Hurting

Fearing you won’t last on that upcoming grueling hike?
This smart routine will prepare your body for handling the hills with grace. (more…)
Locking Elbows Out During Bench Press: Pros & Cons

What are the advantages, if any, to locking out the elbows for the bench press?
Can this even cause an injury to the elbow joint?
For best results, you should not completely lock out the elbows for a bench press. (more…)