How Well Does Cymbalta Work for Spinal Stenosis Back Pain?
Cymbalta may help blunt the pain of spinal stenosis – but not in the way most people would think.
Numb Tingling Finger the Only Symptom of a Herniated Disc?
Is one of your fingers numb and tingling with no explanation?
Are you wondering if a herniated disc (“pinched nerve”) in your neck can be causing this isolated symptom?
“Yes, it’s possible for a numb tingling finger to be the only symptom of a herniated disc,” says John D. Lipani, MD, FACS, neurosurgeon-in-chief for and founding director of Princeton Neurological Surgery in NJ.
“However, this presentation is relatively uncommon,” continues Dr. Lipani.
How is it possible that an irritated nerve in the neck, caused by a disc herniation, can then cause just the isolated symptom of a numb tingling finger?
After all, the nerve in the finger extends up the arm and to the neck.
“A pinched nerve root in the neck may travel down the arm to the tip of the fingers — and depending on which nerve fibers within the nerve root are affected, will determine the patient’s symptoms,” explains Dr. Lipani.
“Usually, pain extends distally [away from the center of the body] from the level where the nerve is pinched (i.e., in the neck).
“But again, sometimes the pain and/or numbness skips the arms and is only experienced in the finger or fingers.”
Likewise, a pinched nerve in the lower back can cause symptoms in a foot, while “skipping” past the length of the leg.
A sudden onset of tingling and numbness in a finger or two has many potential causes.
One common cause is trauma, which you might not even remember, such as lying on a finger while asleep.
Nerve irritation at the level of the elbow or wrist as well can cause a finger to tingle or feel numb.
Give the situation several days to resolve. If it doesn’t, see a doctor, as there are tests that can definitively determine the cause.
If you’ve already been diagnosed with a pinched nerve or herniated disc, this isn’t necessarily the cause of a new-onset, numb and tingling finger – but, it could be.
 Dr. Lipani is a board certified, fellowship-trained neurosurgeon. His specialties include minimally invasive spine surgery and non-invasive brain and spine radiosurgery. He’s the founding director of the JD Lipani Radiosurgery Institute™ for non-invasive neurosurgery.
Dr. Lipani is a board certified, fellowship-trained neurosurgeon. His specialties include minimally invasive spine surgery and non-invasive brain and spine radiosurgery. He’s the founding director of the JD Lipani Radiosurgery Institute™ for non-invasive neurosurgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Bankoo
What Kind of Headaches Can a Pinched Nerve Cause?
Headaches come in many flavors. A pinched nerve in the neck can cause pain in the head — and usually, it’s a certain kind of pain.
“A pinched nerve high in the cervical spine (e.g., C2) can cause sharp, lancinating [piercing, stabbing] pain that travels to the occiput [back of head] that can result in occipital neuralgia,” says John D. Lipani, MD, FACS, neurosurgeon-in-chief for and founding director of Princeton Neurological Surgery in NJ.
Neuralgia means nerve pain. A nerve can become pinched when the spongy, shock-absorbing spinal disc protrudes out from between the vertebral bones, putting pressure on a nerve.
“At first, the pain may start as a dull ache and gradually intensify over days, weeks or even months to full blown occipital neuralgia,” says Dr. Lipani. “Symptoms may vary with position and activity.”
The pain may also be sudden, seemingly from nowhere. At that moment, pressure is put on the nerve, instantly causing head pain. And it can bite hard, often making a person stop in their tracks whatever they’re doing.
People may wonder if they have a brain tumor, simply due to the severity of the pain.
Usually, headaches from a brain tumor are not characterized by sudden stabs of pain. There’s also usually other concerning symptoms by the time a brain tumor causes headaches, such as nausea, vision problems, unsteady gait, unexplained weight loss or fatigue, etc.
Dr. Lipani continues, “A degenerative disc in the neck can also cause occipital headaches, also referred to as cervical headaches.”
Another name for these is cervicogenic headaches.
“This is a consequence of arthritis that causes chronic inflammation within the intervertebral discs, vertebral bodies and/or facet joints.”
An MRI will show if there is any pathology involving the cervical spine or brain.
 Dr. Lipani is a board certified, fellowship-trained neurosurgeon. His specialties include minimally invasive spine surgery and non-invasive brain and spine radiosurgery. He’s the founding director of the JD Lipani Radiosurgery Institute™ for non-invasive neurosurgery.
Dr. Lipani is a board certified, fellowship-trained neurosurgeon. His specialties include minimally invasive spine surgery and non-invasive brain and spine radiosurgery. He’s the founding director of the JD Lipani Radiosurgery Institute™ for non-invasive neurosurgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Menstruation Affect a Herniated Disc?
There may be a connection between your period and the pain of a herniated or “bulging” disc.
But it’s probably not the connection you’re thinking of. (more…)
Can Self Removal of a Skin Tag Cause Cancer?
There’s a cancer related reason why you should never self-remove a skin tag.
A skin tag is formed in areas where there’s friction such as that from clothing or folds in the skin. (more…)
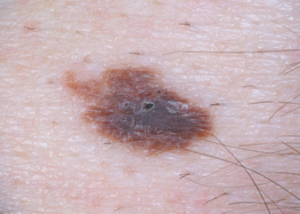
Can Melanoma Grow Back in the Area It Was Removed?
You’re not neurotic if you’re afraid a melanoma will grow back where one was removed and you keep checking the area – because it CAN.
What Does a Grey and Yellow Mole Mean ? Should You Worry ?
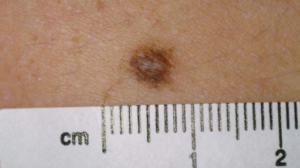
MOLE
Has your mole always been grey and yellow?
Or has it always been kind of grey, and now it has a dull yellow area?
What’s alarming about this is if you know that parts of a melanoma can be yellowish. (more…)
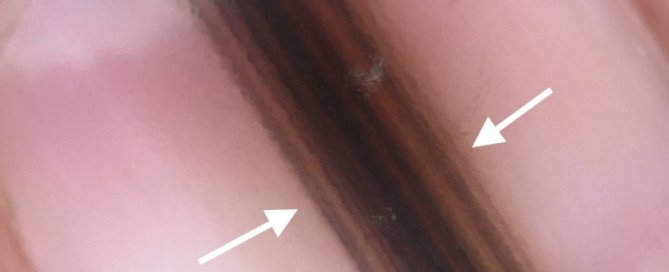
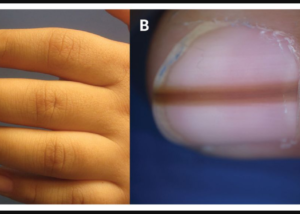
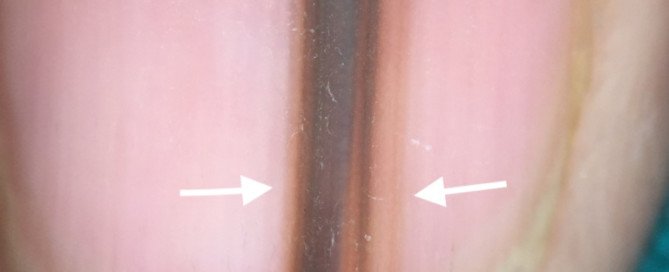
Longitudinal Melanonychia vs. Subungual Melanoma
Subungual melanoma is a type of longitudinal melanonychia, but what are the tipoffs that longitudinal melanonychia is malignant vs. benign?
A brown or black band, stripe, streak or line in a nail is a very common occurrence in men and women of all ages and races. (more…)
What Is a Micro-Hutchinson’s Sign?
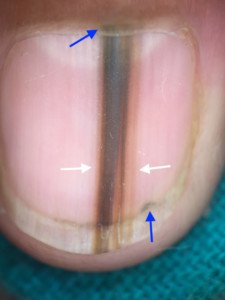
Blue arrows point to Hutchinson’s sign from melanoma shown under magnification. Copyright ©2018 Bhat et al