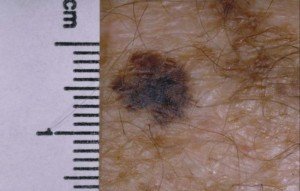
What Does the Local Recurrence of Melanoma Look Like?
A small number of patients will get a local recurrence of melanoma very near to the excision site.
Do you know what a local recurrence looks like? (more…)
Can a Melanoma Survivor Live 30 Years?
If you’ve been diagnosed with stage IV or even stage III melanoma, you’ll likely be wondering if you’ll be alive 30 years from now if you’re middle age or younger.
“In general, survival rate statistics for melanoma are generally calculated at five years and 10 years after initial diagnosis,” says Kara Shah, MD, an adult and pediatric dermatologist and founder of Kenwood Dermatology in Cincinnati, OH.
The five-year survival rate for metastatic melanoma is only four percent, according to the National Cancer Institute Surveillance, Epidemiology and End Results Program.
“Stage IV melanoma involves distant metastasis to other body organs or to distant areas of skin,” says Dr. Shah.
For local disease (both stage 0 and I) the five-year survival is 84 percent.
“While melanoma is unlikely to recur after more than 10 years since diagnosis, it does recur in a small minority of patients (one study documented late recurrence in 6% of patients),” says Dr. Shah.
Two Big Questions
How many people out there walking around were diagnosed with melanoma at least 30 years ago?
How many were diagnosed with stage IV melanoma 30 years ago?
“Melanoma survival is correlated with the stage at diagnosis,” says Dr. Shah.
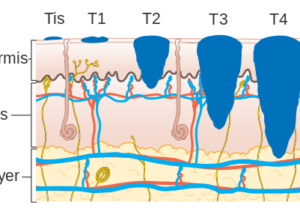
Melanoma
“Stage 0 melanoma, or melanoma in situ, has the best survival prognosis — as it is defined as very early melanoma confined to the superficial component of the skin.” That would be the epidermis.
The five year survival for in situ is over 98 percent. We can deduce that most 30-year survivors of melanoma were diagnosed in the early stage.
Dr. Shah continues, ‘While stage IV melanoma, in which there is distant metastasis of the melanoma to other body organs such as the brain, lungs or liver, has the poorest prognosis.
“Data related to 30-year survival rates is rarely published.
“It is important to note that the treatment paradigm for cutaneous melanoma continues to evolve, and with the recent advent of targeted therapies for melanoma, survival rates have been increasing.
“Most data on survival rates such as that compiled by the National Cancer Institute Surveillance, Epidemiology and End Results (SEER) program use a five-year survival endpoint.”
30-Year Survival Rate for Children vs. Adults
Dr. Shah explains, “With regards to prognosis and age at diagnosis, data suggests that in general, survival statistics for pediatric melanoma mirror those for adults when matched for stage.
“In addition, children are more likely than adults to develop a type of mole called a Spitz nevus that can be misdiagnosed as a melanoma.”

Spitz nevus
This can skewer data for survival rates, even though the number of Spitz nevi that have been mistaken (and hence “treated”) for melanoma is not known.
So can a melanoma survivor live for 30 years?
Yes. It’s just that the statistics for “30-year survival rate” are not known, because the endpoints are either five years or 10 years.
It’s impossible to know how many people in the U.S. are 30+ year survivors of melanoma, let alone a particular stage.
The biggest predictor of whether or not a melanoma survivor will be alive 30 years after diagnosis is likely the stage of the initial disease.
There is no registry for 30+ year survivors of any stage of melanoma.
In this day and age, we can assume that somewhere in cyberspace is a cancer forum in which a 30-year melanoma survivor has posted. Or perhaps they have a blog.
Another way to know they’re out there (but without knowing their numbers) is by personally knowing one.
If you’re a melanoma survivor who’s scared you won’t be around 30 years from now, you should – as all survivors – commit to aggressive surveillance of your skin and never let your guard down.
It will also help to do everything possible to prevent heart disease, high blood pressure and stroke.
There’s no way to know how many melanoma survivors died of cardiovascular disease instead – people who could have lived to at least that 30-year mark had they not developed unrelated illnesses that shortened their life. Or gotten into a fatal car accident for that matter.
Here are more survival statistics from the SEER Program. The overall five-year survival rate of 92.2 percent includes ALL stages of disease.
Why isn’t there any data for 30 years out?
The median age of diagnosis, being 65, is very important to consider when wondering why there’s no data on 30 year survivals.
The vast majority of all 65-year-olds will not be alive 30 years later.
In order for research to be accurate about 30-year survival rates for this skin cancer, the tracked patient base would have to be young enough such that living another 30 years would fall well within normal life expectancies.
Cause of death of patients who died within that timeframe would also have to be tracked, since over a 30-year period, there are so many different potential causes of mortality including the No. 1 cause in the U.S.: heart disease.
Final Point to Consider
Current survival statistics are based on previous populations going back at least five years, and do not apples-to-apples reflect the next five, let alone 10, years of newly diagnosed cases of melanoma.
Dr. Shah is triple board certified: general dermatology, pediatric dermatology and general pediatrics. Her special interests include melanocytic nevi (moles), melanoma, psoriasis, acne, atopic dermatitis/eczema, hair and nail disorders, birthmarks and genetic skin diseases.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Andrey_Popov
Can a Man Help a Woman Run Faster by Holding Her Hand?
How many times have you seen on TV or in the movies a man and woman running away from danger, and he’s holding her hand every step of the way? (more…)
Do Daily Weigh-Ins Mean Poor Body Image & Toxic Diet Culture?
Body image influencers want you to believe that daily weigh-ins mean poor body confidence, no self-love and toxic diet culture. They are wrong. (more…)
Yes, You CAN Tell a Person’s Health Only By Their Size

If we can’t tell a person’s health by their size, does this mean a 600 pound person can be healthy?
Does it mean a 75 pound woman can be healthy? (more…)
Plain Water vs. Electrolytes After Gym Workouts: Which Is Better?
Beverages with electrolytes that are targeted towards fitness enthusiasts is a booming business, but does this mean plain water isn’t good enough after your boot camp class or “leg day”?
(more…)
Headache Every Morning? Could Be Lack of Oxygen to Your Brain

If you’ve been waking up every morning with a headache, this is less likely from a brain tumor and more likely from your brain not getting enough oxygen.
Can Wisdom Teeth Cause Headaches?
Headaches have so many causes, from neck strain and sinus infections to brain tumors and aneurysms.
But what about wisdom teeth? (more…)
Can Cavities Be Cured with Diet? Can Diet Reverse Tooth Decay?
You found out you have several cavities and either can’t afford treatment or are scared of a dentist’s drill. (more…)
Is Holding the Front Bar of a Treadmill While Running Okay ?
Do you hold onto the bar in front when you run on a treadmill?
Stop this. It’s giving you a false sense of accomplishment and will never carry over to outdoor or court running. (more…)