Can Exercise-Induced Acid Reflux Cause LPR?

LPR can make it difficult to breathe, but can acid reflux from exercise cause this scary situation?
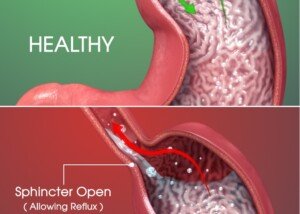
“Acid reflux is when normal stomach acid regurgitates into the esophagus and causes symptoms,” says Jay Desai, MD, who specializes in colon cancer screening, upper endoscopy and consultative gastroenterology with New York Gastroenterology Associates.
“During exercise, this can be exacerbated, especially if you are significantly bearing down on the abdomen (such as in weightlifting, doing crunches, etc.).
“This pressure pushes on the stomach and can cause more acid to be pushed into the esophagus.
“If the acid goes high enough it can irritate the vocal cords. This is called laryngopharyngeal reflux (LPR), and can be diagnosed by an ear, nose, and throat doctor by looking at the vocal cords with a small camera.
“When the vocal cords get irritated by acid, you can develop symptoms of coughing or a hoarse voice.
“Treating the underlying reflux with antacid medication may help these symptoms.”
LPR is often misdiagnosed as exercise-induced asthma when it occurs during or shortly after exercise.
This is especially true if the exercise is of an aerobic nature. The symptoms of laryngopharyngeal reflux disease and asthma are similar enough that this misdiagnosis isn’t all that uncommon.
However, LPR will not respond to the asthma inhaler: “intractable asthma.”
If this describes your situation, it’s advisable that you see an ear, nose and throat doctor (otolaryngologist).
LPR involves the vocal cords and can lead to difficulty breathing, whether it’s caused by acid reflux or an extraneous irritant.
Other symptoms of laryngopharyngeal reflux disease include a hoarse voice, persistent cough, bad taste in the mouth/throat and a sensation of a lump in the throat.

Board certified in internal medicine and gastroenterology, Dr. Desai provides a wide range of GI services including for bacterial overgrowth, constipation, acid reflux and GERD, IBS, incontinence and small bowel disease. Twitter handle: @NYGADocs
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/MikeSaran
Acid Reflux Comes and Goes: Causes
What can make acid reflux come and go if the patient avoids food triggers?
“Acid reflux is when the normal stomach acid regurgitates up into the esophagus,” says Jay Desai, MD, who specializes in colon cancer screening, upper endoscopy and consultative gastroenterology with New York Gastroenterology Associates.
Dr. Desai continues: “In most people it improves and worsens periodically. For example, in periods of severe stress, symptoms of reflux can worsen substantially.
“Acid reflux can also vary in relation to changes in sleep habits, so it is important to try to identify what exacerbates symptoms in each individual patient, and to try to avoid this.
“In some patients, when this is not possible, treating with medical therapy is required.”
If your acid reflux comes and goes with seemingly no rhyme or reason, then it’s time to keep a documentation of it.
• For example, does it seem to come more often when you’re sleeping over your significant other’s house?
• Does it seem to arise only when your in-laws visit?
• How about on the same days you have business meetings?
• Does the fluctuating nature of your acid reflux occurrence seem correlated to when you eat — either the time itself, or perhaps the amount of food, or even the type of food?
• What about exercie? Does it seem to “come” during or right after exercie, and then go away once you’ve been rested for a while?
• Make sure everything even remotely relevant goes into this documentation; do not skip a day. In fact, make note of the days when you’re free of acid reflux symptoms
• Over time, you may begin to see a pattern develop to your acid reflux.

Board certified in internal medicine and gastroenterology, Dr. Desai provides a wide range of GI services including for bacterial overgrowth, constipation, acid reflux and GERD, IBS, incontinence and small bowel disease. Twitter handle: @NYGADocs
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Where to Get the Instruction Manual for Raising Children

But kids DO come with instruction manuals!
Why do we keep hearing “Children don’t come with instruction manuals,” especially in this day and age of online parent communities, tons of websites and blogs about how to raise kids, not to mention all the books published in the past 30 years about childcare?
The irony is that the motto, “Kids don’t come with instructions,” sometimes appears on parenting sites and forums—which give instructions on how to raise kids!
Of all the topics in the world, parenting is probably in the top three when it comes to the availability of instructions, directions, help and advice.
Go to a large newsstand and count how many parenting magazines are on display.
Information on How to Raise Children Is Everywhere

Shutterstock/Just dance
The information will vary from source to source, but the point is that the information is overwhelmingly available.
It’s there at the touch of a mouse, not to mention the following:
- Community in-person support groups
- Free classes at social service agencies, hospitals and recreational centers
Between the Internet, books and magazines, the volume of parenting instructions is simply staggering.
In fact, the wealth of information is so enormous that there are magazines and books on very specific situations, such as publications strictly for newborns, few-months old, under one year, preschooler, gifted, ADHD and many more.
There are parenting magazines that cater to single moms, those who work outside the home, those who have a military spouse, daughters only, party planning, identical twins and much more.
Books on parenting are a sizzling goldmine for “instructions.” There are books on:
- Divorce
- Tough love
- Logical love
- Lenient love
- Bullying
- Raising kids without corporal punishment
- Death/loss
- Only children
- Adopted kids
- Biracial kids
- Life skills
- Sibling relationships
- Talking about sex
- Getting kids to listen
- How to raise “explosive” children
- How to raise boys
- How not to scream at your children
- How to raise caring kids without religion
- How to raise kids with sensory processing disorder
- Autism
There’s even an entire book on how to calm a crying baby (“The Happiest Baby on the Block” by Harvey Karp) and an entire book devoted to how to keep a child occupied while waiting in long lines or during lengthy car rides (“Fun on the run!” by Cynthia L. Copeland).
The only place where there are no instructions on how to raise kids is the moon!
You Need a License to Fish and Cut Hair, but Not Raise Kids
“There is no mandated training to become a parent, no license that you have to obtain,” says Dr. Tia Kern-Butler, a licensed psychologist for over 20 years who treats a broad range of issues including relationship problems and behavioral issues of children and adolescents.
“So I think when this [the instructions mantra] is said, it’s to validate for parents that parenting is the hardest job there is — and one that we are the least prepared to actually take on.
“It’s a phrase that I think was meant to make it safe for parents to admit that it’s okay not to have all the answers.
“While I do agree that there is an abundance of resources for parents to access, the key is for parents to feel comfortable enough to seek these resources without the parent guilt and shame.”
Get the Instructions if You’re a Struggling Parent
What’s really unfortunate is when a flustered parent will state, “Kids don’t come with an instruction manual,” but then refuses to reach out to the massive treasure troves of help, advice and direction – including other parents on the block or at school.
Even a childless person may have some wisdom to share. Sometimes, a solution comes from creative problem solving skills rather than the firsthand experience of raising kids.
Stop kidding yourself that there are no instruction manuals for raising healthy and well-adjusted children. The resources are insanely abundant.
 Currently in private practice Dr. Kern-Butler spent 10 years as the lead child and adolescent psychologist with Winter Haven Hospital and served as the mental health liaison for the Children’s Advocacy Center for 14 years.
Currently in private practice Dr. Kern-Butler spent 10 years as the lead child and adolescent psychologist with Winter Haven Hospital and served as the mental health liaison for the Children’s Advocacy Center for 14 years.
Professionalpsychologyofpinellas.com/about-me
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can a Pacemaker Implant Damage the Vagal Nerve?

If a person has recently had a pacemaker implant, but is also suffering from blackouts or fainting spells, one may wonder if the vagal nerve is somehow getting adversely affected by the pacemaker.
Pacemakers Are Close to the Vagal Nerve
“Pacemakers do not damage vagal nerves,” says David N. Smith, MD, a board certified cardiologist with Premier Cardiovascular Care and Wellness in SC.
He continues: “The question may refer to a phenomenon where the pacemaker implantation process stimulates the vagal nerve to cause hiccups.
“There still would be no damage to the nerve itself. If the pacemaker insertion does stimulate the vagal nerve during implantation, this is more of a reflection of the pacemaker lead being close to the vagal nerve.
“There is no damage to the vagal nerve. The pacemaker lead can be repositioned to correct this.”
What Is a Pacemaker?
This little device has two parts: a generator and electrodes (leads).
It’s placed under the skin (a minor procedure) in the person’s chest where it will then help control, or pace, the heartbeat.
Usually a person needs a pacemaker due to an arrhythmia or abnormal heart rhythm.
If the heart beats too slowly, a pacemaker can set the programmed pace, such as 70 beats per minute.
A pacemaker may be implanted after a person has a heart attack or undergoes coronary bypass surgery.
The pacemaker can detect if the patient’s heartbeat is too slow.
It then sends an electrical signal to the heart to speed up the pulse.
Some people may fear the idea of something being put just under their skin that sends electrical signals to their heart.
But complications from the procedure are uncommon. They include the following:
• Infection at the site of implantation
• Allergic response to the anesthesia or dye that’s used during the implantation
• Bleeding or bruising at the generator site. This is more likely if the patient is on a blood thinner.
• Collapsed lung
• Damage to the blood vessels or nerves (which would include the vagal) near the pacemaker. This is very uncommon.

Dr. Smith is a published author, national lecturer and Yale-trained physician-scientist certified by the American Board of Internal Medicine in Cardiovascular Disease. From his basic science background combined with advanced clinical research training at the Columbia Mailman School of Public Health, he brings an integrated holistic approach to cardiovascular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: J. Heuser/CreativeCommons
Why Isn’t the Corus CAD Test Part of Routine Physical?

Have you been wondering why a routine physical or even routine cardiologist exam doesn’t include the Corus CAD test?
This blood test uses “gene expression” to quickly and safely determine when chest pain is due to obstructive coronary artery disease (clogged arteries).
Some patients are suitable candidates for this test, called the Corus CAD (coronary artery disease).
They have not been diagnosed with a previous heart attack; are not diabetic; have not had a CABG; are not currently on chemotherapeutic drugs, immune-suppressing or steroid prescription drugs.
Chest pain is quite a common symptom of “clogged arteries” (obstructive heart disease).
Another common symptom is undue fatigue or shortness of breath.
The Corus CAD blood test results are ready in 72 hours, and the test can be done in a doctor’s office.
So why isn’t this simple test part of either the routine physical or a heart patient’s routine visit to the cardiologist?
I asked this to cardiologist David N. Smith, MD, a board certified cardiologist with Premier Cardiovascular Care and Wellness in SC.
Dr. Smith explains, “I believe at this point the test is relatively new and most have not heard of its benefits yet.
“Moreover, the diagnostic accuracy and clinical utility of the test fits best when the patient has non-acute signs and symptoms suggestive of obstructive coronary artery disease.
“Therefore, the test should not be used to screen every patient for obstructive CAD.
“Although the test has proven to be reliable in ruling out obstructive in stable symptomatic patients, the truth is it takes many years before new technology will be adapted into the guidelines by the American College of Cardiology or the American Heart Association.
“While numerous Corus CAD studies have been published in highly ranked peer-reviewed journals, it takes time, experience, and more randomized, controlled evidence-based trials before being completely accepted into standard of care.”

Dr. Smith is a published author, national lecturer and Yale-trained physician-scientist certified by the American Board of Internal Medicine in Cardiovascular Disease. From his basic science background combined with advanced clinical research training at the Columbia Mailman School of Public Health, he brings an integrated holistic approach to cardiovascular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Why Don’t CABG Patients Get the Corus CAD Test?

Why isn’t the Corus CAD test given to people who’ve had coronary bypass surgery?
This test uses “gene expression” to safely and quickly determine whose chest pain or shortness of breath is the result of obstructive coronary artery disease (clogged arteries).
Certain patients are candidates for this blood test, called the Corus CAD (coronary artery disease).
They are as follows:
- not diabetic
- have not been diagnosed with a previous heart attack
- have not had coronary artery bypass surgery (CABG)
- are not currently taking chemotherapeutic drugs, immune-suppressing drugs or steroid prescription drugs.
The Corus CAD test can help identify people who are unlikely to have obstructive heart artery disease as the cause of their symptoms.
Chest pain is a very common symptom of obstructive coronary artery disease, the so-called clogged arteries.
Other symptoms are typically that of shortness of breath upon exertion, and increasing fatigue over time.
Less common symptoms include nausea, burning sensation in the upper body, dizziness, lightheaded feeling, and pressure in the throat, jaw, shoulder, abdomen, back or arm.
Often, the only symptom is pain in the chest or what may be described as tightness or pressure.
Corus CAD Blood Test
The Corus CAD blood test results are available in just 72 hours and the test can be done in a doctor’s office.
I wondered why a CABG patient would not be a candidate for this test, since coronary bypass surgery doesn’t actually reduce plaque buildup in arteries,
The heart disease itself continues progressing despite the surgery. What CABG does is re-route the “plumbing” of the heart. This treats the symptom.
“Patients who have CABG have been diagnosed with severe and/or obstructive CAD, and thus were excluded from the clinical trials,” says David N. Smith, MD, a board certified cardiologist with Premier Cardiovascular Care and Wellness in SC.
“Therefore, the test has not been studied with or validated for patients who have had CABG.”

Dr. Smith is a published author, national lecturer and Yale-trained physician-scientist certified by the American Board of Internal Medicine in Cardiovascular Disease. From his basic science background combined with advanced clinical research training at the Columbia Mailman School of Public Health, he brings an integrated holistic approach to cardiovascular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
,
Top image: Freepik.com, peoplecreations
Is IBS a Real Disease & Diagnosis or just Symptom Collection?

“IBS by definition is not a true disease,” says Dr. Saad Habba, MD, a board certified gastroenterologist at Overlook Medical Center in Summit, NJ.
One of Dr. Habba’s areas of interest is irritable bowel syndrome.
He continues, “The condition is a collection of symptoms that are collectively referred to as IBS.
“In fact, many physicians diagnose IBS after some preliminary workup is negative, and it is frequently used as a wastebasket diagnosis.”
If you are ever diagnosed with irritable bowel syndrome but your workup did not include a colonoscopy, this is a reg flag for a wastebasket diagnosis.
Conditions that only a colonoscopy could reveal can cause symptoms that are very similar to those of IBS, namely, microscopic colitis.
“Before diagnosing IBS, a thorough and detailed workup must be done to rule out other medical conditions.”
Dr. Habba performed a large study that demonstrated this very clearly.
It showed that 98 percent of patients with irritable bowel syndrome were prematurely tagged with this diagnosis.
However, when additional detailed workup was performed, other medical conditions were exposed.
It’s vital to get the right diagnosis, even if the symptoms are identical.
For example, people with microscopic colitis are often misdiagnosed with IBS, especially if they’re young adults, because a doctor is less likely to recommend a colonoscopy for a 25-year-old complaining of diarrhea and abdominal cramps (symptoms of both irritable bowel syndrome and microscopic colitis), vs. a 50-year-old reporting the same symptoms.
However, microscopic colitis can only be diagnosed by viewing tissue samples, taken during a colonoscopy, under a microscope.
Dr. Habba says that IBS should not be used as a “catch-all” term as is frequently done.
The symptoms are real alright (who can fake diarrhea, bloating and constipation?), but technically, it’s not a disease.
 Dr. Habba pioneered the concept of IBS being a wastebasket diagnosis and collection of different entities rather than a true single medical condition. He’s been presented and published in 26 national and international medical journals and symposia.
Dr. Habba pioneered the concept of IBS being a wastebasket diagnosis and collection of different entities rather than a true single medical condition. He’s been presented and published in 26 national and international medical journals and symposia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Bannasak Krodkeaw
When Your Child’s Hamster Dies: Guide for Parents
If your child’s hamster is very sick or seems to be dying, here are clear instructions on what you, the parent, should do and NOT do.
In your mind, the hamster might be nothing more than a mindless rodent.
In your child’s mind, the hamster was a cute, cuddly, furry little thing with a personality.
If your child’s beloved hamster has recently died, this can be just as tormenting as if you lost some prized, inanimate memento or piece of jewelry with sentimental meaning.
So be careful how you react to your child whose hamster just died.
When I was 11 years old, my hamster, “Fang,” died. My mother didn’t respond the way a parent should when a child’s pet dies.
I loved that hamster, and he died before his time, having caught some kind of viral or bacterial infection after being handled by several neighborhood children.
How a parent should respond when a child’s hamster dies begins with when the hamster is in the process of dying.
My hamster didn’t die just like that without warning. Fang was sick for a few days preceding his death – very sick. My mother knew this, but didn’t call any veterinarians.
Because I was a naïve 11-year-old, I didn’t think to open the phone book and look under the listings for veterinarians and start making phone calls.
At age 11, I wasn’t supposed to do things like that. I’m not even sure the idea had even occurred to me, actually.
To complicate things, my hamster got sick on a Saturday, when vet clinics are closed.
However, on Sunday, my older sister made a call or two; I cannot recall to whom, but she definitely was making a few phone calls.
But nothing came of them. I think they were to some vet clinics and they were closed.
She gave up pretty quickly, and I was still with a hamster that was getting sicker — I mean really sick, like remaining huddled inside his sleeping bottle.
He wouldn’t come out; wouldn’t eat; and when he moved, it looked painful.
My mother may have asked every so often how Fang was doing, but that was it. Nothing more.
There was no, “On Tuesday we’ll take him to the veterinarian.” Monday was Memorial Day.
Because I was only 11, I didn’t think there was anything that could be done about my sick and dying hamster.
I was completely dependent upon my parents. My parents didn’t really regard Fang as a true pet.
Maybe that’s because hamsters’ brains aren’t developed enough to “know” their handler, like a dog’s and cat’s brain is.
Hamsters don’t look you in the eye and communicate with facial expressions, as do dogs and cats.
We had never had any pets in the house, either; my parents weren’t pet people.
The only reason I had Fang was because my oldest brother, who was daring, one day brought home Fang; in college he had a hamster from the same litter that Fang had come from.

On Memorial Day, Fang was dead; stiff, lifeless, inside his bottle. I cannot recall how I alerted my mother to this.
My father was even less involved, because this was (in my mind) one of those mother things.
But I do remember my mother nonchalantly taking the bottle, with the dead stiff hamster inside, and tossing it in the rubbish outside. And that was that.
There was no consolation; it were as though the dead hamster was an old pair of socks.
Maybe my mother thought that if she didn’t console me or offer words of comfort, that I’d bounce back quickly or not feel any sorrow.
Maybe my mother didn’t know I was distraught that my hamster had died.
But I was determined to retrieve the bottle, with Fang inside, from the garbage can outside.
I did this behind my mother’s back, because I knew she’d never permit this.
It was raining and I fetched the hamster from the garbage can, still in the bottle.
I dug a hole at the side of the house and buried the bottle with Fang inside.
I was just mortified that the whole situation had been treated so casually and matter-of-factly.
If your child’s hamster is sick or dying, phone a veterinarian. Don’t even THINK about how much it might cost you.

When you have kids, you should realize that raising kids isn’t cheap, and unexpected things come up.
- You can put the vet bill on a credit card.
- You can work overtime if you have an outside job.
- You can borrow money from friends and family.
Just GET the dying hamster to a veterinarian — and your child will look up to you for years.
If the hamster is dying on a weekend, call vet clinics until you get one that’s open.
If one is not open, stand by your child and talk about the dying hamster; maybe the hamster isn’t dying and will recover; maybe the hamster will get better if you do certain things with it.
This is something that you, as a parent, should be prepared for; you can get this information from a veterinarian at the time your child first gets the pet.
Do not assume veterinarians are only for dogs, cats and birds. There’s a such thing as a “small animal clinic.”
This means rodents! Hamsters are extremely common as pets, and parents often get a hamster for a child begging for a pet because hamsters are relatively low maintenance pets.
They don’t bark, don’t need to be housebroken, don’t require a lot of food or space, don’t scratch up furniture, etc.
If your child’s hamster dies, you had better be there as emotional support if you want to win permanent brownie points with your child.
And YES, parents SHOULD care if their child “likes” them!
If your child doesn’t have faith and confidence in you, then don’t expect him or her to come running to you for life advice in the future, and don’t be surprised if your child seeks advice about life from his peers instead of from you.
This is Parenting 101, and the School of Common Sense offers this free class year-round.
A hamster is a real pet to a child, even to adults who have them.
I bet you yourself are attached to some nonliving object that has special meaning to you.

Freepik.diller
What if it were stolen or lost? Think about that before you brush the death of your child’s hamster off as trite and trivial.
If your child’s hamster is dying, you have plenty of time to prepare a memorial.
Encourage your child to be a big part in the planning, and do not dismiss the idea as petty and ridiculous.
Instead, be glad that your child has compassion for a creature as small and as helpless as a hamster.
If your child’s hamster has already died, you can still create a memorial of sorts.
Sit down with your kid and ask him or her for ideas. Allow a mourning period for the dead hamster, and do not make your child think you feel it’s silly or nonsensical.
Take it from me, a former child who had a hamster that died prematurely; this makes me an expert in the area of how a parent should react when a child’s hamster is dying or has died.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can GERD Cause Constant Chest and Back Pain?
Are you wondering (hoping) that your constant chest and back pain is being caused by GERD rather than a heart problem?
GERD stands for gastroesophageal reflux disease and is notorious for causing chest pain.
“Acid reflux is when the normal stomach acid regurgitates up into the esophagus,” explains Jay Desai, MD, who specializes in colon cancer screening, upper endoscopy and consultative gastroenterology with New York Gastroenterology Associates.
“The muscles at the bottom of the esophagus are meant to act as a valve to hold down acid, but in many people this valve does not function properly. These symptoms can manifest differently in patients.
“In some patients, especially those with severe reflux, they can have constant chest pain.”
Sometimes, this sensation is more like an ache, including a duller type of ache.
Dr. Desai adds about the constant chest pain, “In general this is due to ulcerations in the esophagus from acid exposure.”
What about back pain?
“Back pain is less commonly associated with reflux. The treatment for this is antacid medication, which helps heal the damage of the esophagus from the acid.”
Keep a record of when your back pain or aching occurs.
-
- Is it only when the chest pain occurs?
- Have you seen a cardiologist to rule out a problem with your heart?
- Have you been diagnosed with GERD?
If you haven’t seen both a gastroenterologist and cardiologist, it’s time to.
Chest plus back pain should never be ignored. One of the conditions that can cause this duo-symptom is a dissecting aortic aneurysm.

Board certified in internal medicine and gastroenterology, Dr. Desai provides a wide range of GI services including for bacterial overgrowth, constipation, acid reflux and GERD, IBS, incontinence and small bowel disease. Twitter handle: @NYGADocs
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Acid Reflux Cause a Heavy Pounding Heart?

Can the acid that’s refluxing up from your stomach and into your esophagus actually trigger a pounding heartbeat?
“Acid reflux is when the normal stomach acid regurgitates up into the esophagus,” says Jay Desai, MD, who specializes in colon cancer screening, upper endoscopy and consultative gastroenterology with New York Gastroenterology Associates.
“This happens to everyone to some degree. However, in some people, the symptoms can be more severe.
“This can be due to the presence of a larger amount of reflux compared to the average individual, or to the esophagus being more sensitive than in others.
“The symptoms of acid reflux can vary between individuals, but most people describe a ‘burning’ sensation in the stomach and chest.
“In some people, these symptoms can feel like a pressure sensation.”
Can acid reflux directly affect the way the heart beats?
Dr. Desai continues, “While a pounding heart is not a typical symptom, sometimes patients with acid reflux can become anxious that another issue, such as a heart attack, is occurring, which can lead to a pounding heart sensation.
“It is important for anyone with these symptoms to discuss them with their doctor to differentiate whether this is reflux related or a primary heart issue.”
Just because GERD or acid reflux doesn’t directly stimulate the heart to beat faster or harder doesn’t mean that a person can’t have both a digestive issue and a cardiac problem.
See a cardiologist for a thorough exam of your heart to rule out any issues such as an arrhythmia.

Board certified in internal medicine and gastroenterology, Dr. Desai provides a wide range of GI services including for bacterial overgrowth, constipation, acid reflux and GERD, IBS, incontinence and small bowel disease. Twitter handle: @NYGADocs
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.