Why Can’t Supplemental Oxygen Alone Treat Sleep Apnea?

Are you wondering why supplemental oxygen rather than a CPAP machine isn’t enough to treat sleep apnea? (more…)
Why Are So Many People Getting Diagnosed with Sleep Apnea?
Is it just your imagination or are there rashes of sleep apnea diagnoses cropping up all over the place?
Is sleep apnea the new “in” disease or do tens of millions of Americans really have it?
You probably know at least five people who’ve been diagnosed with obstructive sleep apnea.
Perhaps you’ve also noticed a new “sleep center” facility in your neighborhood and are wondering, “What’s UP with all this?”
Why It Seems Everyone Is Getting Diagnosed with Obstructive Sleep Apnea
Increased awareness. If you have not been diagnosed with obstructive sleep apnea, but know someone who has, this is enough to increase your awareness.
It’s akin to the phenomenon of noticing that everyone is driving a particular model of car – only after you’ve purchased that car!
Increased awareness by the medical community. Medicine is not finite. Doctors and researchers are always learning something new.
A new discovery does not mean a “fad” or “in” disease just to make money.
Illusion of Sleep Apnea Being a New Disease
“Sleep apnea has been around for a very long time, but wasn’t given its official name until the late 20th century,” says J. Mark Anderson, MD, DABFM, of Executive Medicine of Texas and who is board certified in family medicine.
What OSA used to be regarded as:
• “Prior to sleep apnea being widely recognized, people who died of sleep apnea were often just assumed that they died in their sleep of natural causes, or if elderly, of old age,” says Dr. Anderson.
• “His snoring rattled the windows.” Dr. Anderson says, “Most people who snore, a symptom of sleep apnea, are often undiagnosed sufferers of sleep apnea.”
• “Her snoring was mixed with snorts and gasps.”
• “She’s always been such a sleepyhead.”
• “It’s stress; it’ll fatigue you and give you headaches.”
• “He’s just overworked; too much overtime, not enough vacation time.”
• “Of course she needs 12 hours of sleep a day; she has a three-year-old, a two-year-old and a six-month-old.”
Dr. Anderson explains, “While sleep apnea is underdiagnosed, the number of reported cases are on the rise.
“Perhaps this is due to a number of famous people dying of the condition,” such as Supreme Court Justice Antonin Scalia.
The symptoms of obstructive sleep apnea have always been around. Other symptoms include irritability and trouble concentrating, not to mention falling asleep easily when immobile or inactive.
Just because the cause of these symptoms for some patients has been discovered doesn’t mean that OSA was created for profit.
Some naysayers will point out that sleep centers are cropping up everywhere and are run by doctors for profit.
- Well gee, who should run a sleep center, an auto mechanic?
- A florist?
- Don’t you think that a specialized medical center should be run by a doctor?
As for the profit, medical centers are businesses, just like dental and veterinary centers are businesses.
Just like the guy you go to for a car repair wants your money. Profit does not mean fad or fraud.
Though a lab sleep study can run up to $3,000, this does not invalidate the existence of obstructive sleep apnea.
A sleep study will not miss events of stopped or disordered breathing.
Otherwise, that’s like saying cancer is a fad disease because treatment is so expensive. Or that root canals aren’t necessary because they’re so pricey.
Medicine Continues to Evolve
Obstructive sleep apnea was identified around 1980. That makes its identification, not existence, relatively new. Newly identified and classified should not invalidate prior existence.
“Considerable progress has been made over the last several decades in our understanding of the pathophysiology of both central and obstructive sleep apnea.” – American Journal of Respiratory and Critical Care Medicine (Dec. 2005)
You can bet that years from now there will be an identification of a new medical condition that’s been around for ages.
It’s just that today, doctors and researchers have not made that particular discovery.
Increase in Sleep Apnea Diagnoses: Reasons
• Increased awareness, pamphlets, campaigns, etc.
• More sleep labs and home sleep study equipment available
• Dr. Anderson points out, “The cases of sleep apnea are on the rise mostly due to the change in body composition across the country.
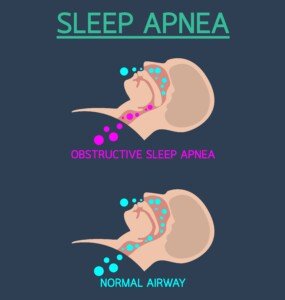
“Obesity is at an all time high, causing a rise also in the cases of sleep apnea. The two are connected because fat deposition around the upper airway can cause the obstruction that leads to sleep apnea.”
Have you heard of the “sitting disease”? This, too, has been brandished as a fad disease for profit. Gee, perhaps doctors are in cohoots with the treadmill desk companies?
Really, do you actually believe that all the diseases that can possibly affect people should have been identified 100 years ago?
Look at smoking. There was a time when smoking was deemed safe. We now know the truth.
But the truth was just as much truth a hundred years ago when some doctors were recommending that harried patients smoke to calm their nerves.
Obesity was once deemed a status symbol rather than a health hazard.
But as time marches on, doctors and researchers gain new knowledge. This is what’s happening with sleep apnea.
“Although OSA is a relatively common medical condition, it is believed that more than 85% of patients with clinically significant OSA have never been diagnosed,” says a report in The Ochsner Journal (fall 2009).
So if you think everybody and his brother has sleep apnea, they probably do.
Obstructive sleep apnea remains as one of the most misdiagnosed and underdiagnosed medical conditions.

Dr. Anderson is coauthor of the award-winning book, “Stay Young: 10 Proven Steps to Ultimate Health,” and host of the nationally syndicated Staying Young Show which goes to podcast as Staying Young Show 2.0.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: ncbi.nlm.nih.gov/pmc/articles/PMC3096276/
Should a Weak Elderly Person Lift Weights or Just Walk?

Let’s suppose you know an elderly man or woman who’s weak and frail, but does not use a cane for walking.
Should this person start a strength training program or a walking program — or both at the same time?
The typical elderly person who’s considered weak does very little walking — only what they absolutely need to do, such as around the house and while shopping.
Walking for the Weak Elderly Individual
“The answer is truly it depends on how weak,” says D’Wan Carpenter, DO, a board certified physical medicine and rehabilitation physician with SIMEDHealth in FLA.
“As a general rule, I would start a more sedentary elder with walking a set distance or time until that became slightly easier.
“Then I recommend increasing the distance and/or time. Once the increased distance or time has become routine, the next best thing is to add ankle or wrist weights to the walk.”
Example Walking Program for a Weak Senior Age Person
- Walk from one end of a long stretch of room in the house to the other — at a faster-than-normal pace for that person.
- Do the return walk slowly to recover.
- Alternate this way for five minutes if possible. This assumes that the person does not have bone-on-bone osteoarthritis.
- Over time, increase one of several metrics: 1) duration of overall walking, 2) duration of just the brisk portion, 3) add soup cans or one-pound dumbbells to the person’s hands.
Walking or light aerobics is not a substitute for strength training: pushing or pulling against resistance, which can be in the form of tension bands, a weighted ball, soup cans or small dumbbells.
Strength Training for the Weak Elderly Person

“I do agree that an elderly person with decreased strength can indeed do walking and strength training,” says Dr. Carpenter.
“Some may need to start with walking first and then add the weight training.
“One good option to add weights is to use the ones that can be strapped to the wrists and ankles during a walk.
“There are several studies which note several benefits to strength training which include building muscle, preserving bone density, decreasing osteoporosis risks, improving mood and better sleep, just to name a few.
“Some helpful exercises include biceps arm curl, triceps extension, shoulder press and squats.”
Squats can be done with one’s body weight only, as depicted below, but if it’s necessary to hold onto something for balance, one should do that.
However, to improve balance and coordination, the elderly individual should not grip the support too tightly or rely on it any more than what’s absolutely necessary.
 Dr. Carpenter is one of the nation’s top board-certified physical medicine and rehabilitation physicians, a national speaker, medical legal expert and independent medical examiner. She is founder and Chief Medical Officer of DJC Physical Medicine Consultants. Follow Dr. D’Wan on Twitter.
Dr. Carpenter is one of the nation’s top board-certified physical medicine and rehabilitation physicians, a national speaker, medical legal expert and independent medical examiner. She is founder and Chief Medical Officer of DJC Physical Medicine Consultants. Follow Dr. D’Wan on Twitter.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
One Mole On Top of Another: Benign or Melanoma?
What appears to be a mole growing on top of another can be melanoma.
“It would be rare but not impossible for one mole to grow within another mole,” says Estee Williams, MD, a board certified medical, cosmetic and surgical dermatologist and assistant clinical professor in dermatology at Mount Sinai Medical Center.
Dr. Williams adds, “Certainly this would constitute a change in the mole, and should be checked in person by a dermatologist.”
That’s the key word: change. Have you known the mole to be on top of, or apparently within, a bigger mole for as long as you can remember?
If so, has the duo changed in appearance? If not, it’s probably as benign as it was years ago.
The medical term for mole is nevus (plural: nevi).
If you’ve always had one mole on top of another, is one of the moles looking different lately?
If so, you need to have a dermatologist inspect it – with a dermatoscope.

Dermatoscope. Freepik/wavebreakmedia_micro
A mole can change into melanoma, as you certainly already know. And a melanoma can arise on top of a mole, and in its early stage of growth, the cancer can resemble a common mole.
But the fact that a benign mole sits on top of or inside of another normal nevus does not make either nevus more likely to commence a malignant transformation. It’s a location thing, not a DNA mutation thing.
In other words, just because a mole is on top of another doesn’t mean it’s atypical.
An atypical nevus, however, can be located anywhere and is made up of atypical cells.
These nevi have an odd or irregular appearance but are benign. Atypia means that the benign mole is simply more likely than a nearby typical mole to ever transform into melanoma. The issue is “more likely to,” not “destined to.”
Dr. Williams’ clinic offers serial digital dermoscopy – computer based mole mapping – to track one’s nevi for changes over time.
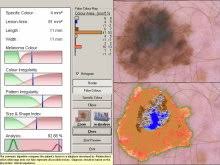
Serial digital dermoscopy
The images are compared to the patient’s previous images for telltale signs of evolution.
The images are also rated by the computer’s algorithm for an index of melanoma suspicion. If the index is high, a biopsy will be recommended.
When a normal or common appearing mole sits on top of another typical looking nevus, this “stacking,” in and of itself, is not a reason to pay extra close attention when you do your monthly skin exams – beyond what is necessary simply to get a good look at the duo.
But remember, if this duo is a new phenomenon, have it checked out!

Dr. Williams strives to be at the forefront of her field, being active in local, national and international medical and cosmetic dermatology conferences.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/pixinoo
How Likely Is a Scab in the Nose that Won’t Heal Skin Cancer?

There are three kinds of skin cancer that can grow inside the nose and present as a scab that won’t heal.
“Any scab that does not heal normally after one month should be evaluated because normal wounds should heal by that time,” explains Estee Williams, MD, a board certified medical, cosmetic and surgical dermatologist and assistant clinical professor in dermatology at Mount Sinai Medical Center.
“This is especially true if you’ve allowed it to heal without picking or traumatizing it! If you have, then there is a good reason why it has failed to heal.
“It is hard to say how likely it is for such a thing to be skin cancer.
“There are other conditions that can causes a non-healing scab in the nose, such as a fissure.”
Skin Cancer Inside Nose that Looks Like a Scab
First off, any growth that you keep picking at will probably bleed, and the bleeding will scab.
If what you’re picking at is a cancer, it will be a scab that won’t heal.
Of course, if you don’t pick at a cancer, it still won’t heal anyways.
But at least if you’re not picking at it, you can honestly tell a dermatologist that you have allowed it plenty of time to heal and are wondering why it hasn’t healed.
Basal cell carcinoma can grow inside the nose. Don’t panic if you get this diagnosis.
The chance of this common skin cancer metastasizing is so super tiny that it’s not even worth mentioning beyond this sentence.
Warning: Graphic Image Below
For all practical purposes, basal cell carcinoma is a local cancer that, if left untreated, will destroy your nose before it ever starts spreading beyond your face.

Neglected basal cell carcinoma
Squamous cell carcinoma, too, can arise inside the nose. However, SCC can spread to organs and if caught late, can be fatal. But it’s a relatively slow growing tumor.
Melanoma, unfortunately, can arise inside the nose and definitely look like a small scab.
A late-caught melanoma is usually fatal.
And yes, skin cancer can grow in places that seemingly get no sun, especially melanoma and squamous cell carcinoma.
 A scabby growth inside the nose can also be a common benign scab — resulting from aggressive picking of the nose.
A scabby growth inside the nose can also be a common benign scab — resulting from aggressive picking of the nose.

Dr. Williams strives to be at the forefront of her field, being active in local, national and international medical and cosmetic dermatology conferences.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Hair ON Nose: Cause & Solutions to Surface Nose Hair

Hair that grows ON the nose is actually quite normal, but there are a few great ways to get rid of this unattractive hair growth.
Do not be alarmed if you’ve recently noticed that a lot of hair has been growing ON your nose.
Why shouldn’t it? After all, skin has hair follicles. Your nose is covered in skin.
For some people, the growth of hair on their nose is more obvious than that in other individuals.
In fact, it’s been said that the human face has as many hair follicles as the face of a lower primate.
It’s just that the hairs of our foreheads, cheeks and nose are very light, fine and short.
And some people end up having darker hair on their nose, making it more visible.
Very fine, “peach fuzz” hair on the nose (and face) is called vellus hair.
Get Rid of Hair on the Nose
There are options far better than that of using a plastic shaver that’s designed for the legs or a man’s facial contours.
And you certainly do not want to pluck at the hairs with a tweezer.
This will hurt and it’ll take forever to get enough hairs to make a difference. Plus, you’ll have to keep redoing this task every several days.
Furthermore, some hairs, though visible, will always be too short to pluck out.
Better Ways…
“Waxing and Biore Clay pore strips are excellent options for removing unwanted nasal hairs, blackheads and whiteheads,” says Estee Williams, MD, a board certified medical, cosmetic and surgical dermatologist and assistant clinical professor in dermatology at Mount Sinai Medical Center.
Waxing the nose can be done at home, but you’ll get better results having a professional aesthetician do the job.
Give the Biore pore strips a try. First wet your nose. Then peel a strip off the plastic and apply to your nose.
Leave on for 10 to 15 minutes. Then peel off the strip starting at its edges.
If the hairs aren’t removed, your nose will still benefit from the deep cleansing action to the pores, which should last three weeks.
Dermaplaning to Rid Hair on the Nose
A trained professional uses a sterile, surgical-grade blade to gently scrape the surface of the skin.
This process removes the top layer of dead skin cells and fine, thin hairs.
While professional dermaplaning is often recommended for the best results and to ensure safety, there are also at-home dermaplaning tools available — which will cost a lot less than what a professional would charge.
If you choose to do it yourself, be cautious to avoid cutting or irritating the skin.

Dr. Williams strives to be at the forefront of her field, being active in local, national and international medical and cosmetic dermatology conferences.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Point Fr
Why Isn’t a Light Sleeper Wakened by Most Sleep Apnea Events?

If a light sleeper could be wakened by a pin dropping 300 feet away, you’d think that most or at least many apnea events would jolt the sleeper to full wakefulness.
CPAP Humidifier Tank Has Mold: Causes and Solution

The humidifier tank of your CPAP machine should not attract mold. If it does, it’s not being cleaned thoroughly.
The issue, then, is just how should the humidifier tank be cleaned to prevent mold buildup? (more…)
10 Signs You’re in Denial of Having Sleep Apnea

Here’s a checklist of 10 signs that are very suspicious for sleep apnea. How many apply to you?
You may think you know all the signs of sleep apnea, but this list will enlighten you and make you really wonder if you just mght have this very often-misdiagnosed condition.
“Sleep apnea increases your risk of high blood pressure,” says Daniel Rifkin, MD, a sleep medicine expert at the Sleep Medicine Centers of Western New York.
“In fact, sleep apnea is one of the common causes of high blood pressure –also known as hypertension.
“We all know the dangers of hypertension including kidney disease, heart disease and so on.”
“Sleep apnea makes you more likely to have atrial fibrillation, an abnormal heart rhythm.
“This can increase your risk of stroke. Furthermore, like noted above with hypertension, sleep apnea, independent of atrial fibrillation, can increase your risk of stroke.
“Almost every patient with stroke should be tested for sleep apnea, as it is seen in 69% of patients with stroke.”
10 Signs You Might Have Sleep Apnea
#1 You snore.
#2 You snort and gasp in your sleep.
#3 People tell you your breathing stops during sleep, then after up to 30 seconds or more, resumes, sometimes followed by a gasp.
#4 You just have to have your daily naps. You’ve repeatedly told yourself that napping is a healthy habit and can’t possibly mean you have a health problem.
You’ve also told yourself that it’s normal to nap for two hours nearly every day despite getting at least eight hours of sleep overnight.
#5 You tell people that your naps are necessary because you “put in long hours at work” or have three young children who keep you on your toes all day long. In short, you keep coming up with excuses.
#6 You keep blaming the frequent morning headaches on either overnight dehydration or lying funny on your pillow.
#7 You blame the most comfortable chair in the house for making you fall asleep nearly every time you watch TV or read.
#8 You’ve convinced yourself that your fatigue is due to not being as young as you used to be or maybe it’s caused by recently gaining 10 pounds.
#9 Your irritability and difficulty with concentration is due to stress — or so you keep telling yourself.
#10 Getting up several times overnight to void is perfectly normal in people over 40 — and you keep reminding yourself of this every time a lot of urine comes out of you in the middle of the night.
Sleep Apnea Checklist
Having just one of the above signs doesn’t automaticaly mean you have OSA.
In fact, none of the above symptoms is caused ONLY by sleep apnea.
However, all of the signs in the checklist deserve an evaluation by a physician.
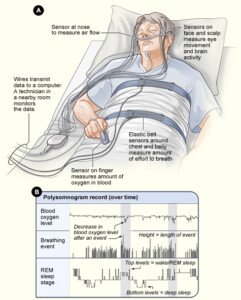
You might then be referred for a sleep study (polysomnography) — a test overnight to see if you have sleep apnea.
 Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
![]()
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Maria Sbytova
Feeling More Tired after Using CPAP: Causes & Solutions

CPAP therapy for sleep apnea should not be making you feel even more tired and drained.
“If you’re actually sleeping the majority of the night and feeling MORE tired than you did without the CPAP, chances are that you have developed complex sleep apnea,” explains Joseph Krainin, MD, board certified in sleep medicine and neurology and founder of the online sleep apnea clinic Singular Sleep.
“Complex sleep apnea refers to a few different conditions, but one of them is when patients with obstructive sleep apnea ‘flip’ to central sleep apnea after initiation of positive airway pressure,” continues Dr. Krainin.
“A sleep apnea test on PAP is required to diagnose this issue.”
What causes the “flip” to central sleep apnea?
First off, if there’s too many central events throughout your sleep, even if your airway is maintained wide open, this can result in feeling bogged down the following day.
A central apnea is when a disconnect between the brain’s signaling system and the respiratory muscles causes you to cease breathing.
So if your airway is nice and wide due to CPAP, it’s as good as being collapsed if you’re not breathing!
Many central events will cause many associated brain arousals — depriving you of restorative sleep.
When the flip occurs, this may be referred to as treatment-emergent central apnea.
According to studies, it occurs in about 10 percent of CPAP users.
Shutterstock/iLoveCoffeeDesign
But there’s good news for the vast majority of this 10 percent:
These treatment-emergent centrals will resolve within several months on their own while continuing CPAP therapy.
Don’t let any of this make you think that CPAP machines cause central sleep apnea.
In fact, it’s not clear just what causes that flipped switch when everything else seems to be working smoothly as far as the CPAP therapy.
But there is a theory.
When CPAP corrects the issue of a collapsed airway, this removes a burden from the respiratory system.
This leads to lower than normal levels of carbon dioxide in the blood, which may trigger a cessation of breathing.
So it’s no wonder that, for a small percentage of patients, they end up feeling as tired with CPAP as they did before the treatment, or in some cases even sleepier despite compliant CPAP use.
Another Reason for Still Feeling Sleepy Despite CPAP Use
If the mask doesn’t fit right and just feels uncomfortable, or if it’s irritating the skin, this will disturb one’s sleep. Mask leaks, too, will disrupt sleep.
Sleep fragmentation results, and this ups the occurrence of what are known as transitional central apneas.
If your mask is giving you trouble, you will be repeatedly awakened to consciousness.
You’ll then transition back into sleep. Here is where you may experience the central events as you enter back into slumber – enough to rob you of the restorative deep sleep that you need.
You may also have arousals below the conscious level as you fitfully cope with the troublesome mask. Subconscious arousals prevent fully restorative sleep.
So even though your airway remains open due to the CPAP, you’re just not refreshed upon waking up and feel tired throughout the day.
Solutions
• As mentioned, treatment-emergent central apnea resolves on its own for most patients.
• About two percent of these patients do not have resolution. To date there is no firmly established protocol for correcting non-resolving TECAs.
• Work with your provider until you find a mask that’s comfortable enough to tolerate well.
• Work to resolve leakage issues.










 In 2013
In 2013 
































