Burning Pain in Arch of Foot: 3 Possible Causes

There are three very likely causes of burning pain in the arch of one’s foot.
“If the burning pain in the arch is toward the heel area on the plantar surface (underside) of the foot, a likely cause is a heel spur or plantar fasciitis,” says Bob Thompson, certified pedorthist, executive director, Institute for Preventive Foot Health.
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
“Plantar fasciitis is inflammation of the plantar fascia, the dense band of fibrous tissue that functions as the main support for the arch of the foot,” continues Thompson.
Causes of plantar fasciitis, says Thompson, are:
• Sudden increase in exercise intensity
• Overuse/overtraining involving the feet
• Faulty biomechanics (e.g., walking on one’s heels, gait abnormality from flat feet or high arch)
• Poorly designed footwear
• Standing for too long
• Being overweight, especially morbidly obese
Second possible cause of burning pain in the arch:
This would be posterior tibial tendonitis. “Tendonitis is inflammation of a tendon,” says Thompson.
“The posterior tibial tendon runs through the area on the medial (inside) area of the ankle and into the arch area.
“This type of tendonitis can occur due to injuries related to falls and athletic activities that put stress on the posterior tibial tendon (as basketball, soccer and tennis).
“Other causes include overuse, degeneration from conditions such as rheumatoid arthritis, diabetes or hypertension and obesity.”
Third possible cause of burning pain in the arch of the foot:
That’s a strained muscle. “The flexor digitorum longus muscle runs along the medial side of the foot in the arch area; and a strain in this muscle can produce burning pain in the arch area,” says Thompson.
“As in other conditions, strains can occur due to overuse and vigorous activities that include running, jumping and throwing, especially if the participant is not well-conditioned for those activities.
“Other causes include fatigue and insufficient or improper warmup before vigorous physical activities.”
Treatments that Will Help Relieve a Burning Pain in the Arch of Your Foot
Initial treatment for plantar fasciitis — perhaps the most common cause for burning in the arch of the foot — typically involves avoidance of the offending activity, ice application and over-the-counter anti-inflammatory medications (NSAIDs).
Stretching exercises for the Achilles tendon and plantar fascia, along with strengthening exercises for the foot and lower leg, can help heal this often burning condition.
Before exiting your bed every morning, spend one minute pulling your toes towards yourself, each foot, to stretch the plantar fascia, which will have tightened up overnight. See the image below.

Plantar fascia stretch. Freepik.com/yanalya
Arch supports are recommended during exercise or sport.
If conservative treatments don’t work, then physical therapy, corticosteroid injections or shockwave therapy may be considered.
Rarely, if other treatments fail and symptoms persist, surgical options may be explored.
Treatment for posterior tibial tendonitis includes rest, ice and NSAIDS.
Physical therapy is important for stretching and strengthening to improve flexibility and support for the tendon.
Custom insoles or arch supports can provide additional stability and relieve pressure on the tendon.

In more severe cases, a brace or walking boot may be used to immobilize the foot and allow healing.
If conservative treatments do not provide relief, corticosteroid injections are an option.
In rare cases, surgical intervention might be necessary.
For a flexor digitorum longus muscle strain, avoid the offending activity and apply warm compresses. Gradually resume activity as the burning in your arch begins subsiding.
To further reduce burning pain in the arch of your foot, or to help prevent any burning from developing or recurring — work on losing weight if you’re overweight.
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Denis Val
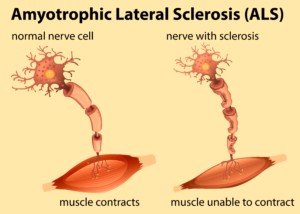
Can Burning Feet Be Caused by a Serious Disease?

Don’t blow off that burning in your feet. This can mean a life-threatening condition.
Don’t assume that feet don’t show symptoms of serious disease.
“Burning feeling in the feet can be an indication of neuropathy (nerve damage),” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (IPHG.org).
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
“Since this is a serious condition, anyone who experiences a burning or tingling sensation in the feet should see a physician immediately,” continues Thompson.
“Neuropathy is most commonly associated with longstanding cases of type 1 or type 2 diabetes.”
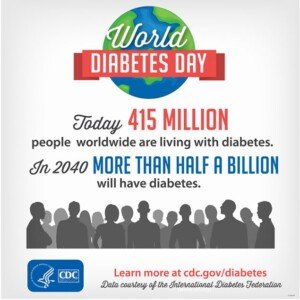
Perhaps you’ve heard the term diabetes neuropathy, and maybe you’ve even seen print magazine ads for medications to alleviate the symptoms, which are often depicted as a burning pins and needles sensation.
Neuropathy, which as mentioned can cause a burning in the feet, has other causes besides diabetes.
These are, says Thompson, “nerve injuries (especially in the lower back), pressure on the spinal nerves from a herniated disc, lack of blood flow to the feet, often because of artery problems, multiple sclerosis, seizures, strokes or transient ischemic attacks, and a number of other systemic issues.”
If you’ve been experiencing burning in the feet that clearly doesn’t seem related to recent excessive activity such as trail running, an all-day hike, an extra strenuous step aerobics class, plyometric (jumping) drills or first-time inline skating, make an appointment to see a doctor.
“If the burning sensation is located between the toes or is accompanied by itching, it is likely due to athlete’s foot,” says Thompson.
“Feet may also burn as a result of alcoholism, Charcot Marie Tooth (a nerve disorder), or certain vitamin and mineral deficiencies.
Simply being in ill-fitting footwear including sneakers all day long — even without a lot of walking — can cause a sensation of mild burning, though this would dissipate by end of day once the shoes are off.
“Burning in the feet is also often associated with certain chemotherapy drugs,” says Thompson.
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss and keeping it off, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss and keeping it off, muscle building, fitness and improved health.
.
Top image: Shutterstock/Africa Studio Foot Pain
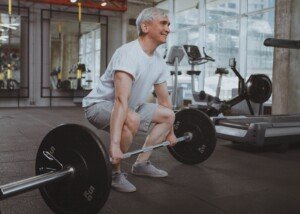
Twitching Muscles: Strength Tests for Quadriceps
Here are reliable strength tests for the quadriceps if twitching muscles have you scared.
As a former personal trainer, I’ve come up with excellent ways to test the strength of your quadriceps muscles.
Strength test # 1
Get up from a sturdy, non-rocking, non-deep chair — or weightlifting bench — with just one leg.
This will not be possible for many healthy people, but if you can do it without using your hands, this should be really reassuring.
Don’t despair if you can’t do this; again, it’s inherently difficult, and should not be attempted from a low chair.
This quadriceps strength test is basically for athletes or well-conditioned gym enthusiasts, but feel free to give it a try.
If you can’t do this, you can still use it as a strength test in terms of progress over the next few weeks.
Progress is reassuring, because it means that the muscle is healthy and getting stronger with repeated attempts.
Strength test # 2
Hop up a flight of stairs with both feet at the same time.
At the top, expect to be winded if you’re able to bound up nonstop. This is a strength test for your quadriceps, not a test of cardiovascular stamina.

Shutterstock/Vadim Martynenko
Begin slowly at first, as agility is required, and non-athletic people risk stumbling. Go one slow step at a time. With both feet, jump to the next step and collect your balance.
Proceed at a comfortable pace. If both quadriceps are normal, you will feel an equality in your legs, rather than one noticeably deficient relative to the other.
If you’re sloppy doing this, the thing to look for is equality or bilateral ability.
Non-athletes will struggle with this, but if their muscles are healthy, the struggling will be equal in both legs, or bilateral.
Practice this daily; a person with healthy muscles will experience progress.
Strength test # 3
Dash up and down a staircase or outdoor steps.
Did one quad’s “weakness” cause you to stumble and fall?

Athletes or exercise enthusiasts can try all sorts of things for quadriceps strength tests, such as jumping up and down exercise stools; performing barbell and dumbbell squats; deadlifts; leg presses and leg extensions.
If you can perform these with the same amount of weight you’ve always used, and especially if you’re making gains as far as mount of weight lifted, this should be extremely reassuring.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com
Cause of Sudden Arm, Leg Weakness on One Side of Body

The cause of sudden weakness of an arm and leg on one side of the body isn’t necessarily a stroke.
If unexplained arm and leg weakness are happening to you, ask yourself if, in the past few months, you bumped your head or fell and hit your head — or in some way, got banged in the head — even if at the time there were no symptoms.
Dr. Irene Gatti de Leon began experiencing weakness in her right arm and leg, seemingly out of the blue.
Two months prior, she had slipped on some ice and hit her head, but at the time was able to shake it off and didn’t give it a second thought.
Two months later, when she began having weakness in her arm and leg, she didn’t make the connection.
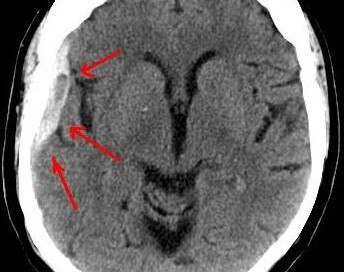
She wasted no time getting an MRI, which revealed a chronic subdural hematoma — a large one compressing her brain.
“Chronic subdural hematoma develops over the course of weeks and sometimes, if the size is small, can cause no symptoms,” says Natasha Fuksina, MD, an internal and integrative medicine specialist who combines traditional and functional medicine to restore health and function.
“However, as the pressure from the bleeding increases it can cause symptoms such as headache, dizziness, personality changes and even progress to the weakness of the arm and leg the opposite side of the body (contralateral side).
“In severe cases, subdural hematoma can cause loss of consciousness and death if the pressure it exerts on the brain is extremely high.”
Sudden Arm and Leg Weakness on One Side: Not Always a Stroke
My mother passed out from a sudden blood pressure drop while standing at the bathroom sink, and on the way down, hit her head against the porcelain bathtub.
She wasn’t even conscious as she fell, so thus couldn’t even help break the fall.
When I heard that awful thud (I was on the lower level), I immediately knew what happened and flew up the stairs.
Unlike the Dr. Gatti de Leon case, my mother had a brain scan that very day — but it showed no subdural hematoma; it was normal.
Six weeks later she had sudden weakness in both legs, particularly the left.
If a chronic subdural hematoma is ignored, with the patient thinking that sudden arm or leg weakness is from stress or working too hard, the patient risks permanent disability — similar to that suffered from a stroke.
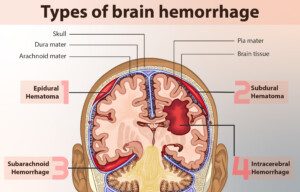
“The brain is covered by three layers of coverings (meninges) – dura, arachnoid and pia,” says Dr. Fuksina.
“A subdural hematoma is a collection of blood outside of the brain — between the outermost layer (dura) and the middle layer (arachnoid).”
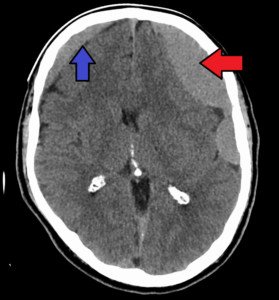
Subdural hematoma. James Heilman, MD
An acute subdural hematoma is immediately life-threatening, since the bleeding is rapid.
A chronic subdural hematoma leaks blood very slowly over time, which is why the patient can go weeks without symptoms, and then literally awaken one day with significant arm and leg weakness.
Neurological symptoms should never be ignored.
If you have sudden or even gradual weakness of an arm and leg, especially on one side of the body, seek immediate medical attention; insist on a brain scan.
 Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/GBALLGIGGSPHOTO
Source: sciencedaily.com/releases/2012/04/120413145220.htm
Ripping Chest Pain: Get to ER ASAP! This Could Kill You

Ripping, Stabbing Chest Pain that Suddenly Occurs: Get to ER, Stat
A stabbing, severe kind of chest pain that suddenly comes on isn’t necessarily caused by a heart attack.
But this doesn’t mean it can’t be life threatening. It very well CAN be.
Think Aortic Dissection
“Stabbing or ripping chest pain always raises the specter of what we call ‘aortic dissection,’ says Dr. John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
Schematic of an aortic dissection. Shutterstock/sciencepics
“Aortic dissection means internal tearing of the aorta, separating the inner from the outer layers of the aorta,” continues Dr. Elefteriades.
“This is exactly a ripping apart of the layers of the aorta, just as the term implies. This is a very serious condition that usually requires an immediate operation.”
Aortic Dissection Cannot Resolve on Its Own
This situation never self-corrects. It only gets worse; the course of it will lead to death 100 percent of the time … unless it is promptly treated—and treatment is always surgery (which may be open heart or endovascular).
Taking ground-up aspirin or a nitroglycerin pill would be useless in the event of an aortic dissection.
So would chest compressions, because the blood that should be pumped to the body’s organs is spilling out of the aorta and filling up the chest cavity.
An aortic dissection results in massive internal bleeding. Some patients will die within minutes.
However, there are others who have had a delayed visit to the ER visit, not realizing how serious their situation was, and because the dissection was of a slower nature, they survived despite delaying the ER visit by up to a few days.
But don’t assume that can be you, even if the pain kind of feels like it has subsided a bit. Don’t take any chances. Just get to the emergency room.
A “slower” dissection will ultimately lead to death if it is not surgically repaired.
So if you or someone you know has been complaining of agonizing or ripping chest pain, don’t wait another second in getting to the ER.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com
Can Severe Persistent Chest Pain Be Caused by Cancer?
Persistent and especially severe chest pain usually gets people worrying about their heart, but this symptom can also be caused by cancer.
“Chest pain is abnormal and important and must be reported to a doctor,” says Dr. John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
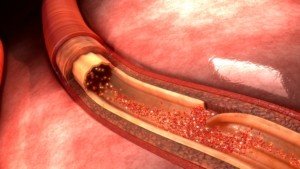
“As everyone knows, chest pain felt under the breastbone can be a sign of angina or heart attack,” continues Dr. Elefteriades.
“Angina indicates that the heart is receiving inadequate blood flow due to arteries blocked by arteriosclerosis.”
Arteriosclerosis is hardening of the arteries from plaque buildup.
“Angina usually comes on with exertion or emotion. Women and men feel chest pain differently, as shown in the accompanying diagram (to come).
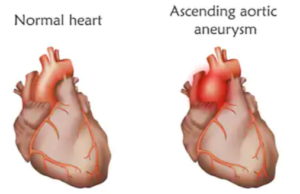
“Chest pain can also indicate an aneurysm of the aorta, the main artery of the body. This pain is usually non-exertional.
“If felt in the front, it indicates involvement of the ascending aorta in the front of the chest.
“If felt in the back (between the shoulder blades), it indicates involvement of the descending aorta in the back of the chest.”
An aneurysm is an abnormal enlargement of a blood vessel; the enlarged area is weak and prone to rupture or dissection — a life-threatening situation that requires immediate surgery.
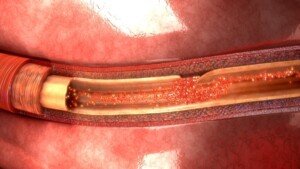
A tear in the inner lining of the aorta. Shutterstock
“Chest pain can also indicate that there is a lung cancer impinging on or invading the chest wall.”
As the tumor grows, it may spread to nearby structures, including the chest wall, causing discomfort or pain in the chest area.
This type of pain is often persistent and may worsen with movement or breathing.
Additionally, the pain can be accompanied by other symptoms such as persistent cough, weight loss, shortness of breath or blood in the sputum.
Can persistent chest pain have a non-serious cause?
Dr. Elefteriades continues, “Chest pain can also be benign, from inflammation of the costal cartilages, the soft bone that connects the ribs to the breastbone in the front of the chest.”
This is called costochondritis, and athletes who have this have been known to report that the pain is quite severe.
The pain associated with costochondritis, even though it has nothing to do with the heart, is typically sharp or aching and may vary in intensity.
It is often exacerbated by certain movements or pressure on the chest, such as coughing, deep breathing or physical activity.
The discomfort can also be tender to touch in the affected area, which is often found along the upper ribs.
“However, if you are having chest pain, you must report this and have it checked out,” urges Dr. Elefteriades. Especially if it’s persistent.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Chest Pain with Hoarse Voice: May Be Cancer or Aortic Aneurysm
Have you been experiencing a hoarse voice and chest pain?
If your chest pain and hoarse voice seem to be connected to each other, and even if they don’t seem related, this can indicate a potentially life-threatening situation.
“A hoarse voice by itself just indicates voice box (larynx) or vocal cord problems, like inflammation, infection, or polyps–as we see with celebrities like Julie Andrews or Adele,” says Dr. John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
“The additional symptom of chest pain puts this in a different category.
“The nerves that operate the vocal cords, called the ‘recurrent laryngeal nerves,’ run (curiously) into the chest and around the arch of the aorta before ascending back to innervate the vocal cords.”
The aorta, the body’s largest blood vessel, branches off the heart and supplies the body with blood.
Dr. Elefteriades continues, “So, a combination of chest pain and hoarseness makes one think of space-occupying lesions in the chest in the vicinity of the recurrent laryngeal nerves.
“Such lesions could include aneurysms and tumors and cancers.”
An aneurysm is an abnormally enlarged blood vessel, sometimes referred to as dilated or ballooned.
The ballooned or enlarged portion is very weak and prone to tearing or rupture; there is a direct correlation between size of aneurysm and likelihood of tearing or rupture.
Shutterstock/Veronika Zakharova
“These lesions cause chest pain by compressing adjacent structures and impinging on intra-thoracic (in-the-thorax) nerves,” continues Dr. Elefteriades.
“These lesions cause hoarseness by stretching the recurrent laryngeal nerves, thus disturbing their function. This disturbance may be transient or permanent.
“Sometimes, with removal of the offending mass, vocal cord function can return to normal.
“The symptoms must be attended to, as not only is the hoarseness troublesome in itself, but an aneurysm or tumor or growth can be very serious and life-threatening.”
If you have chest pain with a hoarse voice, seek immediate attention:
An aortic aneurysm can rupture without warning; half of all patients with a ruptured aortic aneurysm die before they reach the hospital.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Andrey_Popov
Symptoms You Can Expect After Coronary Bypass Surgery
How can the coronary bypass patient know which are normal postoperative symptoms and which ones warrant a trip to the emergency room?
Is the line fuzzy here?
My mother had quintuple bypass surgery, and there were ongoing issues the first three weeks after surgery, including severe abdominal pain.
When I phoned the on-call doctor, he said to get her into the emergency room.
So I drove the 40 minutes down there, at around midnight.
After she got out of the car, she began collapsing. At the time, I thought it was a heart attack and had no idea what it really was (it turned out to be a sudden severe drop in blood pressure).
In the ER she was immediately tended to, and this included an ultrasound of her abdominal aorta (presumably to see if the severe abdominal pain was being caused by a rupturing aortic aneurysm).
The cause of the pain was never determined and my mother eventually made a full recovery.
Some select articles on coronary bypass surgery
Everyone who’s had CABG, plans on having CABG, or has a family member who’s had or is planning on having CABG, should read these articles:
- Vomiting after surgery
- Abdominal pain after surgery
- Chest pain after surgery
- Trouble breathing after surgery
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/virgo1957
Severe Chest Pain from GERD Can Mimic Heart Attack Feeling

The chest pain from GERD can feel just like the chest pain that occurs during a heart attack or one that’s about to occur.
GERD is a very common condition. Unfortunately, the chest pain that gastroesophageal reflux disease causes can be severe enough to mimic a heart attack, says Dr. Maxwell Chait, MD, gastroenterologist at ColumbiaDoctors Medical Group in Westchester County, NY.
Can an abdominal spasm be the only symptom of GERD?
Dr. Chait responds that the problem could be an esophageal spasm or “nutcracker esophagus.”
He adds, “These are true spasms of the muscle of the esophagus and can cause chest or upper abdominal pain that can be severe and mimic a heart attack.”
If you’re in the ER and report this symptom, you will have blood drawn to see if an enzyme called troponin has leaked into your blood.
The test for this is extremely sensitive and hence, extremely accurate in determining if you’ve had a recent heart attack or if you’re in the process of having one.
When cardiac muscle is damaged, troponin leaks from the tissue into the bloodstream.
But back to the abdominal spasm or a hiccup-like sensation…
Dr. Chait says that this can also “be associated with a sensation called water brash, which is the welling up of fluid in the mouth that one feels just before they vomit.”
He adds, “Both may be warning signs of GERD when it is associated with more severe problems such as esophagitis, gastritis, ulcer disease, etc.
“The spasm feeling also may not be related to the esophagus and actually be related to diseases of the gallbladder, stomach or pancreas.
“Either way, when someone gets these severe symptoms, they need further evaluation by their doctor.”
Severe chest pain or abdominal pain should never be ignored.
Though there are numerous non-serious causes, there are also quite a few serious causes.
Plus, you should never attempt to make a diagnosis; medical imaging can reveal a lot about what’s going on in the body, and that includes GERD.

Dr. Chait’s practice interests include digestive conditions such as colon cancer, gastrointestinal endoscopy and internal medicine. He has authored numerous publications in reputed journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
BRAIN BLEED from Concussion Can Mean Subdural Hematoma
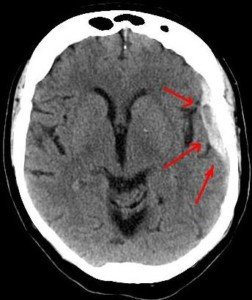
Bleeding in the brain, namely a subdural hematoma, can result from getting hit in the head or hitting your head in a fall.
“Traumatic brain injury (TBI) can produce hemorrhages (including subdural, epidural and subarachnoid) from the focal trauma to a particular area of the brain,” says D’Wan Carpenter, DO, a board certified physical medicine and rehabilitation physician with SIMEDHealth in FLA.
“In the case of subdural hematoma (SDH), the traumatic force causes shearing of the bridging veins which lie between the pia-arachnoid layer and the dura.
“There is an increased risk of subdural occurring from concussion/mild TBI in people with cerebral atrophy (generalized loss of brain parenchyma), a normal finding in the elderly.”
This is because there’s more room or space between the veins and the skull for them to be torn, whereas, in young people, this space is very tight (due to a bigger brain).
Younger people are far more likely to sustain an acute subdural hematoma — typically from vehicular crashes and sport-related impact (skiing, boxing, football).

“The findings of a SDH can occur immediately [acute], between three days and three weeks [sub-acute] or greater than three weeks [chronic],” says Dr. Carpenter.
“This is in part due to the fact that the blood flow through the bridging veins is at a low pressure.
“And this [sometimes] creates a slow leak of blood into the space between the skull and the dura mater.
“The severity of the TBI is typically related to the rate blood accumulates.”
An acute subdural hematoma is an emergency situation and has an 80 percent mortality rate.
Credit: myupchar/wikimedia commons
With a chronic subdural hematoma the patient can go weeks, even a few months, before symptoms begin appearing.
This happened to my mother: Six weeks after fainting and then falling, hitting her head on the ceramic bathtub — she experienced her first symptoms.
One was weakness in a leg and a difference in the way she walked as a result.
She also experienced a major, persistent headache that she described as a “crown of thorns.”
 Dr. Carpenter is one of the nation’s top board-certified physical medicine and rehabilitation physicians, a national speaker, medical legal expert and independent medical examiner. She is founder and Chief Medical Officer of DJC Physical Medicine Consultants. Follow Dr. D’Wan on Twitter.
Dr. Carpenter is one of the nation’s top board-certified physical medicine and rehabilitation physicians, a national speaker, medical legal expert and independent medical examiner. She is founder and Chief Medical Officer of DJC Physical Medicine Consultants. Follow Dr. D’Wan on Twitter.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.