How Effective is Cymbalta for Treating Depression?

Cymbalta snuffed out my mother’s crippling depression.
Yes, the antidepressant Cymbalta literally saved my mother’s life. Cymbalta wiped out my mother’s depression and panic attacks, with no side effects save for a few brief dizzy spells at the beginning.
My mother became disabled from depression, which included a weight loss of 12 pounds (mostly muscle) from refusing to eat, and reverted to weeping over the tiniest issues.
I didn’t need medical training to recognize a textbook case of clinical depression, and I recommended an antidepressant (though not naming Cymbalta specifically).
It all began when I planned on living with my parents for about three days, to help my mother recover from knee arthroscopic surgery.
Little did I know that a power-hungry depression awaited me and would hold me hostage there for over two months.
In hindsight, I realize that subtle signs of depression had been present for several weeks preceding the surgery.
However, the depression began stomping its feet the morning of the knee surgery, and had an unforgiving accomplice: panic attacks.
My mother had had orthopedic surgeries before, but never sobbed or was convinced she was dying like this time.
The problem was merely a meniscus tear in the knee. She also complained that the fingers of both hands were tingly.
Several days after the surgery, I suspected clinical depression and I began urging my father for “psychiatric intervention,” and that “she needs an antidepressant!”
Both my mother and father adamantly opposed antidepressants.
My mother denied having depression, and attributed her apathy, overall weakness, inability to hold herself together while doing simple shopping, comments about wanting to die, excessive crying, loss of appetite and withdrawal from daily activities to:
1) post-surgical knee discomfort, and then 2) a developing pain in both hands and arms, along with continuing tingling in the fingers.
My father admitted something was wrong, but attributed it to “lingering effects of anesthesia” (even five days out from surgery), and then to the hand pain (eventually diagnosed as carpal tunnel syndrome).
Meanwhile my mother often talked about her funeral, gave us “If I die…” talks, and often said her entire body hurt.
“She has depression!” I kept harping to my father, who still opposed antidepressants and accused me of trying to play doctor.
After six weeks of taking care of my mother, including daily battles to get her to eat, I finally convinced my exhausted father to embrace an antidepressant.
I chose Cymbalta because at the time, we thought that her frequent shoulder pain (which would trigger hard sobbing) was residual nerve pain from the double carpal tunnel syndrome surgery.

In addition to nerve pain, Cymbalta is prescribed for panic attacks, and my mother often felt as though death were imminent.
I showed my father information from a Web site about how major depression can cause whole-body pain and amplify pre-existing joint pain by heightening a person’s perception of pain.
I just had a gut feeling that the Cymbalta would take out the depression like a tank.
That evening my mother took one 30 mg Cymbalta capsule. “I don’t know how long it will take before it kicks in,” I told her, “But believe me, this is the RIGHT thing to do.”
Next morning, my mother awakened feeling vibrant, pain-free, and eager for a big breakfast.
Absent was the scene for the past six weeks: a withered, crying, wasted-looking stranger. My mother’s eyes were alive, voice robust. She said, “I feel GREAT!”
I said, “It’s the drug, the Cymbalta, it worked!”
My mother needed no help sitting upright; she popped right up and got ready for the day as though nothing were wrong. “For the first time in weeks, I feel human!” she said.
And for the first time in seven weeks, she washed her hair. My father was floored by the drug’s effect.
The Cymbalta prescription was 30 mg daily for the first week, then 60 mg the second week.
The Cymbalta was working so beautifully that on the eighth evening, I kept the dose at 30 mg (I was in charge of administration).
Next day, my mother had a partial relapse and asked, “Do you think it’s because you didn’t double the dose?” I said, “Yes. Well, tonight you’re getting 60 mg.”
Early next morning while still in bed, my mother boldly said, “I feel SO strong, like I can just swing my legs off the bed and stand right up!”
She then began talking about going out for breakfast and doing some shopping to buy ingredients to make bread and meat pies — while still in bed.
Another three weeks on 60 mg worked wonderfully, and then we had to increase to 90 mg. Cymbalta restored my mother’s appetite, wiped out panic attacks, brought back her laughter, resurrected social connections, and motivated her to stick to an exercise plan.
Since taking Cymbalta, my mother has had NO “my whole body hurts” episodes, and the shoulder pain (eventually diagnosed as rotator cuff tears) has significantly diminished — or perhaps her perception of it has.
And when the shoulder pain does occasionally act up, my mother doesn’t sweat it, whereas pre-Cymbalta, she’d sob away and completely shut down.
About five weeks after starting Cymbalta, my mother’s energy level began plummeting; she felt increasingly drained and excessively sleepy, even though her mood remained normal.
We took her to the ER, and a blood test revealed a medical condition, hypothyroidism, that’s known to cause depression.
She started treatment the next day. In retrospect, my mother had been showing signs of low thyroid for several months, but we didn’t think much of the subtle symptoms.
Also, about five weeks after beginning Cymbalta, my mother signed with a new medical plan that didn’t cover Cymbalta, and thus had to gradually transition to a comparable dose of Effexor. These two unexpected developments extended my stay with my parents.
Effexor, like Cymbalta, is a seratonin/norepinephrine reuptake inhibitor. The transition from Cymbalta to Effexor was smooth, save for a disabling case of persistent dizziness on the last dose-changing day — yet despite that, my mother was upbeat.
In summary, my mother is now gradually tapering off Effexor; apparently, the depression is now under control with the treatment for that medical disorder.
There are NO problems with the Effexor tapering, and absolutely NO relapse of the depression, which is strong evidence that the depression’s underlying cause was the low thyroid.
(Original publication date: January 2010)
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
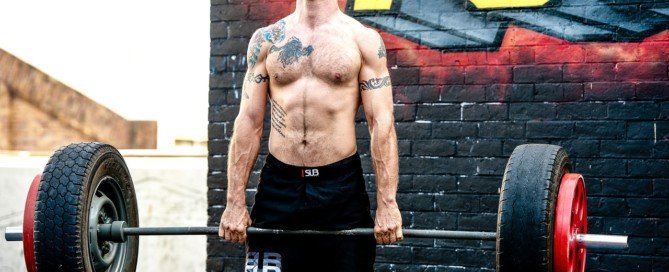
Can Heavy Lifting, Squatting, Deadlifting Cause Aneurysm?
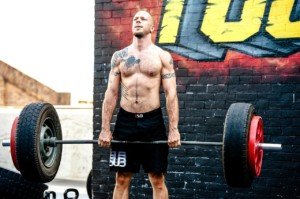
Does that nasty headache from heavy weightlifting mean you might have an aneurysm?
Sometimes heavy weightlifting (squats, deadlift, etc.) can cause a headache and make you think this is an aneurysm.
I’m a former certified personal trainer and know for certain that a headache, while doing heavy lifts, can be brought on by dehydration, even though you may not feel thirsty.
To help rule out dehydration as the cause of a bad headache that occurs during or after deadlifting, squatting or some other heavy weightlifting routine, drink plenty of water prior to working out; a tall glass worth.
- Fifteen minutes into your routine (including any warming up), drink some more water.
- Every 15 minutes drink four ounces (half a cup) water.
Also make sure that you’ve been adequately nourished throughout the day with nutritious food.
If you nevertheless develop a headache during your weightlifting or shortly after, the first possible cause may be due to an increase in the venous pressure of the brain.
A primary thunderclap headache can be caused by heavy weightlifting. And we all know how heavy and wicked a set of deadlifts and back-squatting can be.
The primary thunderclap headache is related to the vasoconstriction of the blood vessels that feed the brain.
If you’ve been worrying about an aneurysm being triggered by your weightlifting, or if you’re troubled by headaches following your workouts, even though you’ve been drinking plenty of water, speak to your physician just to play safe.
What about an aneurysm?
If you experience a sudden-onset bad headache while working out, stop immediately.
“Patients with a history of brain aneurysm or family history of aneurysm may be at increased risk of bleeding during intensive exercises like heavy lifting or weight-squatting,” says Atif Zafar, MD, medical director of St. Michaels Hospital in Toronto, Ontario, and former director of the stroke program at University of New Mexico Hospital.
A ruptured aneurysm is called a hemorrhagic stroke.
“These exercises do not cause aneurysm per se,” adds Dr. Zafar.
An aneurysm is a bulge in a blood vessel. This can remain dormant for many years, though over time, may increase in size.
The bigger it gets, the weaker its walls get, making it more prone to rupture — at any time of the day.
So if you already have an aneurysm, then there’s a small chance that heavy squats and deadlifts – by themselves — may cause it to get bigger.
However, if you have perfectly healthy blood vessels in your brain, lifting weights will NOT cause the actual formation of the bulge. Do not mix up formation with rupture.
The actual cause of formation may be genetic as well as from smoking and uncontrolled high blood pressure. And yes, there are weightlifting enthusiasts who smoke.
Hypertension rarely presents with symptoms. So even if you feel great, don’t smoke and can lift the entire gym building, get your blood pressure checked! You can do this with a home device.
• Heavy powerlifting or other styles of strength training do not cause chronic hypertension.
• A high sodium diet can lead to hypertension.
• It’s believed that in some cases, chronic high blood pressure has a genetic cause.
• Chronic hypertension can also be caused by untreated obstructive sleep apnea.
Though middle age and excess body fat can bring this out, a younger leaner person can still have it simply due to the natural structures of their throat, such as a large tongue base.
Dr. Zafar also explains, “Now if a person is taking cocaine or amphetamines or has underlying hypertension, in that case, every time they would do heavy lifting or deadlifting, naturally their blood pressure will spike even more.”
So what’s the most likely cause of a worsening, pre-existing aneurysm in someone who powerlifts?
“The long-term effect of uncontrolled hypertension or drug use can cause strokes or worsen the underlying aneurysm, rather than the primary effect of these heavy exercises,” says Dr. Zafar.
A ruptured aneurysm typically presents with a most horrible, very sudden headache that incapacitates a person.
If one eyelid is drooping with the headache, this is HIGHLY SUSPICIOUS for a rupturing aneurysm. Other possible symptoms are nausea/vomiting and confusion.
Dr. Zafar is author of the book, “Why Doctors Need to Be Leaders.” His interests include vascular and endovascular neurology, and the neurosciences.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
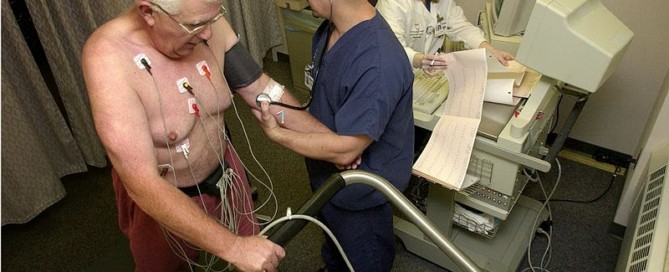
How a Cardiologist Can Miss Severe Heart Disease in Women

A cardiologist provides insight into how a specialist can examine a woman with severe heart disease and then tell her she’s in great shape
Cardiologists do indeed miss severe heart disease in women (men as well, but more prevalently, women).
One reason is because despite all the mounting media attention given to women’s heart disease, many doctors take the symptoms more seriously in men, and also, symptoms of heart disease in women oftentimes differ from those in men.
“Communication between doctor and patient is critical,” says Suzanne Steinbaum, MD, a New York cardiologist for 20+ years and founder of SRS heart — a groundbreaking program for womens’ holistic health prevention.
We have all heard many stories of young women who were dismissed by their doctors as being healthy, only to find out later that they had heart disease.
“It is important, from the patient’s perspective to discuss all the symptoms, and address all concerns,” says Dr. Steinbaum.
“Discussing family history is crucial in giving your doctor a true understanding of your own risk.”
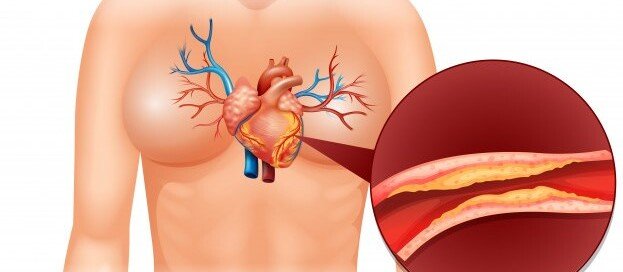
Dr. Steinbaum adds, “Heart disease is invisible until is presents itself, so even if you are thin and fit, you can still be at risk.”
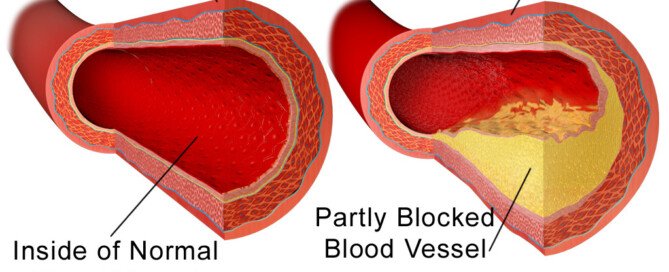
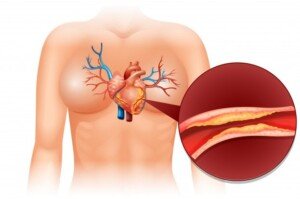
Diet is a big player in coronary artery disease. No matter how hard you train in the gym, you cannot out-train bad nutrition.

Shutterstock/Altagracia Art
You may look great and be able to knock off pushups and run 5Ks, but a processed-food diet and mental stress can cause plaque to build up inside your coronary arteries.
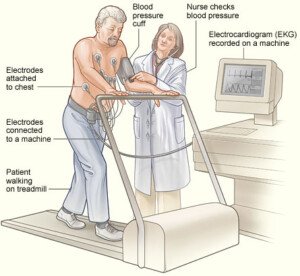
“Baseline EKG’s, echocardiograms and blood tests don’t always predict who is going to have a heart attack, and even simple stress tests without imaging studies may be misleading,” says Dr. Steinbaum.
“Communicating symptoms and changes in activity levels might be the first clues that there are cardiac problems.”
Unfortunately, though some women are aware of recently-new symptoms, they don’t connect them to possible severe heart disease.
My mother experienced shortness of breath for months and attributed this to narcotic painkillers, which CAN cause labored breathing
Then one morning she upchucked, after suffering shortness of breath, and still, did not make a connection.
My father even questioned her on what she ate the day before! Severe coronary plaque buildup was the last thing on their minds at this point.
However, the vomiting tipped me off and I took her to the ER where she was diagnosed with reflux disease and released!
Two days later I took her back for chest pains. She was admitted, and the next day I was told by three doctors that a massive heart attack was imminent due to blockages of at least 97 percent in five coronary arteries.
Ten months prior, my mother’s cardiologist (not one of the three) told her, “You’re the last person I’d ever think would have a heart attack.” Ten months later she had emergent quintuple bypass surgery.
Dr. Steinbaum says, “Sometimes your sixth sense tells you somethingis significantly wrong. As a patient, you must empower yourself.”
One way a woman can do that is to undergo a calcium score test which is pretty accurate for determining the likelihood of coronary artery disease, and near-future heart attack, which kills about 267,000 U.S. women every year – over six times the rate of breast cancer death.

Dr. Steinbaum has been awarded a New York Times Super Doctor, a Castle and Connolly Top Doctor for Cardiovascular Disease, and New York Magazine’s prestigious Best Doctors in the New York edition. She is on the NYC Board of the American Heart Association.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos.com
Source: womensheart.org/content/HeartDisease/heart_disease_facts.asp
High Calcium Score but Normal Stress Test: Should You Worry?
So your calcium scan score is high, but your stress test was negative and showed no diminished blood flow through your coronary arteries.
Are you off the hook?
Do you wonder about the implications of a high coronary calcium score and a normal-result stress test (either chemical or exercise) in the same patient?
After all, a stress test measures blood flow through the coronary arteries.
A stress test does not show plaque buildup, including the “soft” type of plaque, which is the type that has the potential to rupture and cause a heart attack.
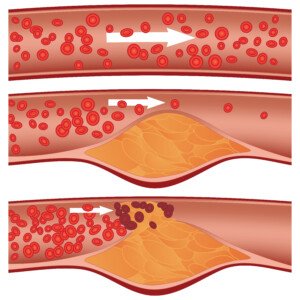
Soft plaque rupture. Shutterstock/Diamond_Images
For such a patient with both findings (high calcium score but normal stress test), Larry Santora, MD, explains:
“Never assume all is well. Look it as a great opportunity to change your life and make things better.”
Dr. Santora is a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
He explains, “You cannot ignore the calcium or plaque, but now that you have identified it and you know what your heart is like, there is no longer any question that you have coronary disease. You can take charge; you can now control it.”
There is a third variable, besides the high calcium score and the normal stress test: absence of symptoms (e.g., chest pain, difficulty breathing).
Suppose a patient has a really high calcium score, but the stress test is normal, and he or she is not experiencing any symptoms and even “feels fine.”
Dr. Santora says that such a patient does “not need an invasive angiogram or stent or bypass surgery.”
In fact, the general consensus is that if the stress test is normal, the patient has no symptoms, but the calcium score is high, it is not warranted to have an elective bypass surgery or even stent procedure.
But does this come to terms with the phenomenon that sometimes, the first symptom of severe heart disease is a heart attack?
Is it smarter to wait to see what might happen?
Should this patient undergo the invasive catheter angiogram which carries the risk of heart attack and stroke?
After all, a high calcium score means something is wrong.
Perhaps a CT angiogram is in order, to get a clearer picture of the arteries and see how much soft plaque (the dangerous plaque) there is.
Only problem is that if the calcium score is high enough, this will contraindicate a CT angiogram; the presence of all that calcium will obscure the imaging.
So what should the patient do?
Dr. Santora says, “You need to make lifestyle changes and be on a combination of cholesterol medications (even if cholesterol is normal) to prevent the plaque from progressing, or worse, suddenly rupturing and causing a heart attack.

Freepik.com/schantalao
“The calcium score (think of it as a plaque score) tells us: how low to get your cholesterol and the types of cholesterol medications, and how frequently to get a stress test; for instance, if you have zero calcium you do not even need a stress test if you have no symptoms.”
Just when you thought the plan sounds simple, keep in mind that taking a cholesterol-lowering drug to prevent plaque progression doesn’t guarantee this result.
For example, a person has a calcium score of 450, which is considered high risk for heart attack, or severe heart disease.
He or she goes on a statin drug to help prevent plaque progression.
Over the next 10 years, the patient doesn’t bother with follow-up calcium scans, but finally has a second calcium scan 10 years later:
The score is nearly 1200. Yet all this time he’d been on the cholesterol-lowering drug.
What happened?
These drugs do not guarantee prevention of further plaque buildup, especially if the patient has a junk food diet.
The coronary calcium score is the “total amount of plaque in all the arteries and gives a very good prediction of heart attack risk over 10 yrs (that is, long-term risk), and chance of short-term risk, that is, what is the chance of having an abnormal stress test due to the artery being significantly narrowed,” says Dr. Santora.
And then there is the coronary calcium percentile, which “reflects how aggressive your atherosclerosis is.”
Dr. Santora explains, “If you have a percentile of 75%, that means you have more plaque than 75% of others of similar sex and the same age. You need aggressive treatment.”
Aggressive treatment starts with setting goals.
Dr. Santora says that the HDL cholesterol should be greater than 50; and the LDL cholesterol should be less than 70.
The LDL in this case should be less than 70 “if you have a high score (>300 or percentile >70%),” adds Dr. Santora.
“However, if the score is zero, then an LDL cholesterol <160, near 130, is fine. A big difference in your cholesterol based on calcium score.”
Diet should consist of a moderate amount of carbohydrate (about half of total calories), and slow-absorbing carbs at that; 25% protein and 25% “healthy fats” like olive oil and safflower oil.
The patient is prescribed a statin.
Dr. Santora adds, “If the percentile is >75%, we order an advanced lipid panel to look for LDL size, HDL subtypes, and Lp(a); these abnormalities respond to niacin which, when added to a statin, provides the best chance in preventing plaque progression.”

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
CT Calcium Scoring & Radiation Cancer Risk: EBCT vs. 64 Slice

Fear of radiation exposure keeps some people from getting a calcium score done for their coronary arteries.
The calcium score is a strong predictor of likelihood of a future heart attack. The equipment used for calcium scoring is the CAT scanner, also known as “CT.”
The amount of radiation delivered during most CT calcium score tests is 2-3 millisieverts up to 8 millisieverts (msvs).
A millisievert is a unit of radiation emission. We are exposed to radiation all around us, and a year’s worth of radiation, in general, amounts to around 3 millisieverts.
You may have heard about a recent study that concludes that the risk of getting cancer from a CT scan is “one in 1,000.”
However, this study leaves several questions, such as how many CT scans would it take to produce this result?
And what about the length of time in between each CT scan? What about age of the patient? What about type of CT scanner (msvs delivered)?
Regarding the one in 1,000 conclusion, “There is no reliable statistic for this and I believe the fear is well-overblown,” says Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
He explains, “That being said, it is wise to adhere to the lowest radiation dose possible. There are various types of CT scanners.
“The premier and fastest scanner for coronary calcium screening is the EBCT ( also called ULTRAFAST CT).”
EBCT stands for electron beam computed tomography.
Dr. Santora continues, “This is the gold standard for coronary calcium screening, the fastest and most accurate, and the lowest radiation dose, about the equivalent of two chest X-rays.
“The standard CT scanners are called a spiral or multi-detector CT scanner, like the ‘64 slice CT,’ which can also be used for calcium screening, but are less accurate and much higher radiation, about 15 to 30 chest X-rays of radiation.”
Dr. Santora’s group at the Orange County Heart Institute has been using only EBCT scanners for coronary calcium scoring for 15+ years.
The Institute, however, uses the 64 slice for CT angiography for the coronary arteries, to measure for possible narrowing and levels of “soft” plaque.
“The cancer risk from an EBCT heart scan is infinitesimally small,” he continues.
How many millisieverts of radiation does an EBCT calcium scoring emit? Six-tenths of a millisievert.
This is less than one dental X-ray, says Dr. Santora, or the equivalent of one abdominal X-ray.
A much lower radiation dose isn’t the only benefit with EBCT.
Dr. Santora explains, “The X-ray beam comes only through the patient from behind throughout the back, whereas regular CT spirals (multi-detector CT like 64 slice) go around.
“The thyroid and breast tissue are the most sensitive organs to radiation, so with EBCT they get very little radiation, while they get a lot with other CT.
“So EBCT is overall less radiation, and the most sensitive organs get a lot less.”

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Brian A Jackson
Can You Be Too Young to Have Calcium Buildup in Heart Arteries?

How young is too young to have measurable plaque buildup in the coronary arteries?
A coronary artery calcium score exam has been proven to be very reliable at predicting the likelihood of a coronary event such as a heart attack, one to three years out from having the exam.
I wondered, however, if a person can be too young to have a buildup of calcium in their coronary arteries; I don’t mean as in toddler young, but more like young adulthood or teenage-hood.
“I think you mean at what age does calcified plaque develop. It is rare to see calcified plaque in men younger than 30 or woman younger than 35,” says Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
Dr. Santora continues, “We start to develop very minor ‘fatty streaks’ as the earliest development of atherosclerosis in our early 20s.”
Atherosclerosis is the term for plaque buildup in arteries.
Dr. Santora continues, “This was determined during autopsies on Korean War Vets. We usually do not do EBCT scans on men younger than 35 or woman younger than 40 since it is unusual to see calcification in the plaque at ages younger than this.”
EBCT is electron beam computed tomography, a type of CAT scan that is used for calcium scoring (and other imaging studies).
EBCT emits lower radiation than does the more common 64-slice CAT scanner.
“The radiation is equivalent to 2-3 chest X- rays using EBCT scanners, vs, 10-15 chest X-rays for conventional CT scans,” says Dr. Santora.
“In addition, the radiation beam comes from behind the back, exposing very little radiation to breast and thyroid, using EBCT, whereas the X-ray beam encircles the body when using conventional CT.”
There are exceptions when it comes to getting coronary calcium buildup at an early age, continues Dr. Santora.
He explains, “…dialysis patients, juvenile diabetics who smoke, anabolic steroid abusers, and those with familial hyperlipidemias who have family history of heart attacks in their 30s.” Hyperlipidemia is excess fat in the circulating blood.
- About 75 percent of women age 45 to 49 are found to have a coronary calcium score of zero, meaning no measurable atherosclerosis.
- Over 95 percent of women age 30-34 have a coronary calcium score of zero.
- For men in this age group, it’s close to 90 percent.
- For men under 30 it’s 99 percent. Dr. Santora says, “Atherosclerosis is a very unusual cause of death in someone under 25 years old.”
This doesn’t mean that young adults and teens have a green light for living on a junk food diet, smoking and avoiding exercise.
A young adult may have a zero coronary calcium score, and thus think he or she can get away with regularly eating heart-harmful foods and not exercising.
But the predictive factor of calcium scoring is short-term (1-3 years), and 10 years down the road, that young adult who feels invincible may end up having a growing problem inside his or her arteries.

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: newportbodyscan.com/GuidetoCoronaryCalciumScoring.htm
Can You Have a Low Calcium Score with Blocked Arteries?
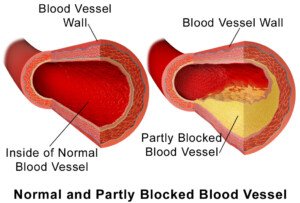
Is it possible to have blocked arteries but at the same time a low coronary calcium score?
The calcium score is a numerical value that’s associated with the likelihood of having soft plaque heart disease.
“A blocked artery means the narrowing in the artery is more than 70 percent narrowed, the point where blood flow is restricted,” says Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
Dr. Santora explains, “This is called ‘obstructive coronary artery disease.’ There is a direct relationship between total calcium score and ‘obstructive disease,’ so if the calcium score is greater than 100, the chance of an abnormal stress test is greater than 3 percent.
“If the score is greater than 400, the chance of an abnormal stress test is 15 percent, and so it goes”
A stress test can be done either with physical exercise or a chemical stress test.
“So you can have obstruction, though it is very unlikely, even with a very low score.
“However, if you are having angina, even with a very low score, then the chance of an abnormal stress test becomes dramatically higher.
“So anyone with symptoms of chest pain should have a stress test first, because you are then trying to determine if the chest pain is due to obstruction of blood flow in the coronary arteries.”
Can a person have a very high coronary calcium score, yet less than a 70 percent blockage in the arteries?
Dr. Santora explains, “The reason the score is high but the artery lumen (channel) is not severely narrowed is because the plaque is forming in the walls of the artery.”
Wouldn’t a CT angiogram (which measures the amount of unstable soft plaque) be preferable over a stress test?
After all, can not a stress exam miss severe coronary blockage? Wouldn’t the CT angiogram, which emits less radiation than a stress test, be more definitive?
“The CTA would be a helpful tool, but not preferable, since the CTA shows the shape of the artery (anatomy), but not the function or ‘flow’ in the artery,” says Dr. Santora.
Flow is also referred to as perfusion, which is why stress exams are usually called perfusion stress tests or myocardial perfusion tests.
Dr. Santora continues, “The stress test is a ‘functional test,’ whereas a CTA is an anatomic test. Sometimes, even with an invasive angiogram (which uses catheters), I find blockages that look borderline in narrowing, like 60 to 70 percent.
“Before putting in a stent, we place a wire through the narrowing and measure flow.
“It is called a functional flow reserve test (FFR). If the flow is not restricted, then I do not put in a stent.”

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus
Calcium Score Too High for CT Angiogram to Show Arteries?
Suppose you’ve been wanting a CT angiogram, and your cardiologist has informed you that the CT angiogram would be pointless —
— because your very high calcium score indicates that all the calcification in your arteries would obscure the images on the CT angiogram.
What should you do at this point?
“A CT angiogram has limitations if there is severe calcification (a calcium score > 800),” says Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
He adds, “There is a good chance the CT scan cannot see through the calcium to see the lumen (channel) of the artery. High scores are a relative contraindication.”
So if your physician says that the CT angiogram is out, due to a very high calcium score, this is the real deal, unfortunately.
It’s likely that one day, technology will advance enough to create a way for a CT angiogram to read through the heavy calcification.
Until then, you are left with the next step, which is a “stress test,” which can be done via exercise to stress the heart, or chemical stress (usually given instead of exercise if the patient cannot carry out sufficient physical exertion, e.g., patient has osteoarthritis).
Dr. Santora says, “If the stress test (nuclear or stress echocardiogram) is normal, you do not need a CT angiogram.”
This will sound surprising to the patient who has a very high calcium score, since the higher the calcium score, the higher the likelihood that he or she will have a heart attack in the next several years. The correlation between the two is well-established.
“The stress test becomes abnormal when there is a narrowing of at least 70% in the coronary artery.
“Such a blockage may benefit from a mechanical fix, like an intracoronary stent or coronary bypass.
“The idea is if the stress test is normal, there is no restriction of blood that requires such a fix.”
But Dr. Santora explains that there are two key indications for the CT angiogram:
No. 1: “A stress test that is equivocal for decreased blood flow — that is, it is a little abnormal, but not enough to make a diagnosis.”
And No. 2: “Unexplained chest pain.”
If the patient with the very high calcium score undergoes a stress test with normal or negative-finding results, and he has not been having unexplained chest pain, then he does not need the CT angiogram. Dr. Santora says that CT angiograms are not screening tests.
So if you’re this type of patient with the exceedingly high calcium score, but a normal stress test result and no chest pain … what is your next step?
Well, it certainly isn’t to go home feeling safe, because there is a reason why your calcium score is so high.
You need to go on an aggressive treatment to prevent further calcification of the arteries, increase stabilization of the plaque, prevent or slow further plaque buildup, and even reverse some of the plaque buildup.
A normal stress test does not rule out the presence of the dangerous kind of plaque – the “soft” and unstable plaque that is prone to rupturing and causing heart attack.
Do not let a normal stress test fool you. A stress test simply detects blood flow through arteries.
It cannot tell how much soft plaque you have! The CT angiogram can do this.
But the CT angiogram, again, is pointless if the images are obscured.
Hence, you absolutely need to commit to aggressive treatment, which comes in the form of a change in diet, addition of supplements, and prescription drugs that are designed to put some brakes on coronary plaque buildup.
Daily, structured exercise is also part of this plan. If you smoke, quit, once and for all.

Dr. Santora’s areas of interest include interventional cardiology – coronary stenting; cardiac CT – CT angiography, and coronary calcium screening with EBCT. He is board certified in cardiovascular disease and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
No Family History of Heart Disease: You Sure About That?
You can be fooled into thinking that you don’t have a family history of heart disease!
Do you really know for sure? Would your relatives tell you they had heart disease?
My mother repeatedly told a steady stream of medical professionals, “I have no family history of heart disease,” and, “There is no heart disease in my family,” after she had a quintuple bypass surgery and mitral valve replacement.
There is no way my mother could know with certainty that she has no family history of heart disease.
She bases this on the fact that her own mother lived to 94 and was never diagnosed with heart disease. Her father died at 73 from an endocrine disorder.
We can’t rule out that her mother had heart disease.
We can only rule out that by the time she was 94, if she had heart disease, it had not yet reached the point of coronary attack.
And had her father lived beyond 73, who’s to say he wouldn’t have eventually developed chest pain, shortness of breath and even a massive coronary? He was not autopsied.
For all we know, at the time of his death, his coronary arteries were 90 percent blocked.
Had he lived another several years, who’s to say he would not have ended up in the ER with chest pain, and then next day, had emergent coronary bypass surgery?
My maternal grandparents were never diagnosed with heart disease, but then again, they also never underwent the following modern-day screening and diagnostic tests:
- echocardiogram
- catheter angiogram
- CT angiogram
- CT calcium score
- treadmill stress test
- adenosine perfusion scan (chemical stress test)
- C reactive protein blood test.
A person, such as my mother, could have very advanced heart disease yet still have a normal-sounding heartbeat under a stethoscope!
A cardiologist gave her a clean bill of health just 10 months prior to the emergent quintuple bypass surgery!
And this clean bill of health was based on a stethoscope exam, pulse-feel, blood pressure reading, an EKG that was impossible to discern due to a “left bundle branch,” height and weight chart, and questions about family history of heart disease!
I’ll assume that my maternal grandparents had routine physical checkups – that were very similar. You can see how heart disease can be missed with such rudimentary testing.
This happens contemporarily as well. People are told they are as fit as a fiddle, after a routine physical, and then shortly after keel over from a cardiac event caused by severe coronary artery blockages.
Both my mother’s parents could have easily had undiagnosed heart disease, even though they didn’t die from it. Many people with undiagnosed heart disease die from unrelated causes.
Pneumonia following hip replacement took my maternal grandmother. There was no autopsy. How do we know she didn’t have 90 percent coronary artery blockage?
I might add that my mother’s sister, about eight months prior to my mother’s coronary bypass surgery, had stents placed in her coronary arteries!
My mother’s sister has heart disease! This is family history! However, my mother didn’t know this (and still doesn’t) because my aunt never told her. I found out through another relative!
If you think you’re safe from coronary heart disease because you believe there’s no family history of it, you may want to revisit your conclusions good and hard.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/brgfx
Why Isn’t All Stable Angina Treated with Stents or Surgery?

Must some people live with angina instead of getting it treated with stents or bypass surgery?
So many people live with stable angina rather than get stents or bypass surgery.
“It is rare that angina can’t be treated with stents or CABG in this day and age, but it does occur.” CABG stands for coronary artery bypass grafting,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Severe diffuse narrowings throughout the entire length of an artery may be untreatable with either method,” continues Dr. Fiocco.
“There are also cases not suitable for stents, but may be anatomically fine for CABG, but other medical conditions make CABG prohibitive (i.e., severe lung disease, terminal illness, etc.).
“There are patients whose angina is well-controlled with medication, and that is an appropriate treatment method as long as the patient is followed closely.”
In 2006, 10.2 million U.S. people were living with angina.
Angina is when there is restricted blood/oxygen flow to the heart due to narrowing and blockage of the coronary arteries.
Every year about 500,000 people in the U.S. are diagnosed with stable angina: Symptoms occur only upon physical exertion and sometimes mental stress.
That’s a lot of people living with a condition that seemingly could be corrected with stenting, angioplasty or bypass surgery, but obviously, that is not the case.
Dr. Fiocco continues, “Many patients control their angina for years with medication. Yes, they may have to curb their lifestyle (no chopping wood, running marathons, etc.), but this is an acceptable treatment regimen.
“If symptoms worsen, become more frequent or difficult to control, then they may need stenting or CABG.
“Some may have no choice but medical treatment due to other health problems or strictly based on coronary anatomy.
“Others prefer to avoid the more invasive procedures, which is acceptable as long as their symptoms remain stable.”
Medications used to treat stable angina are the following: aspirin, nitrates, beta blockers, statins, calcium channel blockers, ACE inhibitors, and ranolazine.
A person with angina should also make lifestyle changes, such as quitting smoking, losing weight, exercising and managing mental stress better.
The reason that coronary bypass surgery is not the treatment of choice for stable angina is because balloon angioplasty with stent placement has been shown to be an effective treatment, and of course, it’s not nearly as invasive as CABG.
Medications will still probably be necessary after the stenting.