Are Heart Attacks with No Chest Pain Less Severe?

Is there a link between how mild or severe chest pain is, and how mild or massive a heart attack is?
Heart attacks often come with chest pain, but some come without or with just a little bit of discomfort.
It should not be surprising that for many people who’ve suffered a significant or massive heart attack, the chest pain was either mild or non-existent.
“Your body is often not good at identifying heart pain because it has not had any practice,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
Hanifin explains, “Think about your thumb. You have spent your whole life touching it, twisting it, burning it, hitting it with a hammer, slamming it in the door, and getting splinters stuck in it.
“When something is wrong with your thumb, your body knows just what is going on.
“Contrast this with your heart. At least during your first episode, your nervous system has no experience identifying heart pain.
“When you start to have a heart attack, your body can have a hard time figuring out what is going on. The pain can radiate to either arm, your neck, your jaw and even your teeth.”
Study Shows No Connection Between Absence of Chest Pain and Severity of Heart Attack
A paper published in a Sept. 2013 JAMA Internal Medicine details a study of over a thousand women 55+ who had heart attacks – but reported no chest pain.
Dr. Louise Pilote, senior study author, urges people to get away from the perception that heart attacks usually mean an “older man clutching his chest.”
There are other symptoms to be acutely on the lookout for, such as shortness of breath, weakness and rapid pulse.
The so-called Hollywood Heart Attack creates the illusion that this event necessarily comes with enough pain to make someone clutch or grab their chest.
In the study, 20% of women suffering a heart attack did not experience chest pain. And, absence of chest pain was not associated with less severe heart attacks.
Don’t ever think, “Well, if I’m having a heart attack, it’s only mild because I don’t have any chest pain with this shortness of breath.”
The absence of chest pain may mean fewer symptoms altogether, but this does not mean that the disease state itself is less severe.
An exact diagnosis cannot be made based on presence or absence of symptoms.
“Another important factor to consider is that some patients who are at increased for heart attack generally have decreased pain sensation,” says Hanifin.
“Diabetes is a big risk factor for coronary artery disease.
“It’s pretty well-known that diabetics need to check their feet regularly and carefully because they can develop sores and injuries and not have the associated pain. The same thing can happen with heart pain.”
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/uzhursky
Source: sciencedaily.com/releases/2013/09/130916204742.htm
How Accurate Is a Stress Test for Women’s Heart Disease Detection?
A treadmill stress test to determine the presence of heart disease in women is not as accurate as you may think.
If you’ve always imagined that all a woman needs to do, to find out if she has clogged coronary arteries (heart disease), is to take a treadmill stress test so that doctors can see if there’s restricted blood flow during exercise — think again.
Maybe one day it will be that easy, but currently, it’s nowhere near it.
“It is a known fact that stress test has 50% sensitivity and specificity for detecting CAD in women younger than 60 years of age due to the phenomenon of false positive test,” says Asim Cheema, MD, who’s board certified in internal medicine, cardiovascular diseases and interventional cardiology by the American Board of Internal Medicine. Dr. Cheema is with Your Doctors Online, an online doctor chat site.
Dr. Cheema also adds, “The exact cause/mechanism of false positive test in women is unknown but likely related to hormones (progesterone).”
Let’s Look at a Study
A study in the Dec. 2012 issue of The American Journal of Cardiology reports a promising conclusion to researchers’ investigation of treadmill stress tests identifying heart disease in women.
However, the percentages aren’t exactly super high, as you’re about to find out.
The report points out that many physicians don’t put a lot of faith in the accuracy of the exercise treadmill test (ETT) in detecting women’s heart disease.
Nevertheless, the researchers, from UC Davis, discovered that the exercise treadmill test can accurately predict heart disease in women over age 65.
Though this sounds great, it’s not too impressive for women under age 65.
The paper notes that the predictive efficacy of the treadmill stress test was enhanced by two particular EKG indications.
The exercise treadmill exam includes an EKG reading. If the exam detects signs of heart disease, then more invasive and definitive procedures are warranted, such as the catheter angiogram.
This is actually the gold standard in identifying blockages, but it’s very invasive and carries with it the risk of stroke and heart attack.
The study involved 111 women who reported chest pain and whose treadmill results were “positive.” These women underwent catheter angiograms.
The Results
Half the women had heart disease (determined by the catheter angiogram).
When the results were broken down by age, the percentage went up to 68 percent for women over age 65, and down to 36 percent for women 35 to 50.
The percentage for the older women may not seem impressive, but to the researchers, it’s a mark of a successful procedure.
What about the EKG?
Two indicators, called the ST-segment depression and the ST-segment recovery, turned out to be important to the ETT’s diagnostic value.
For women over 65, longer ST-segment recovery time yielded an 80 percent prediction rate of heart disease.
Tips for Reducing the Risk of Coronary Artery Disease for Women and Men
• Don’t stress about the small things in life. Practice stress management.
• Realize that just because you “feel” beautiful doesn’t mean you practice heart-healthy habits.
Make sure you’re at a medically acceptable weight.
• Do both strength and cardio exercise.

Shutterstock/Nata Kotliar
• Don’t assume your heart is healthy just because you weigh 120. If you smoke, quit. If you eat a lot of processed foods, cut back, especially on high sodium foods.
• Avoid trans fats, limit saturated fats, and eat more “good fat” foods like olive oil, seeds, nuts and fish.

Your Doctors Online offers a free 7 day trial where you can ask a doctor questions online and get answers in minutes from anywhere 24/7. Learn more here. Dr. Cheema teaches and provides supervision to graduate students at the Institute of Medical Sciences, University of Toronto.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2012/12/121206153646.htm
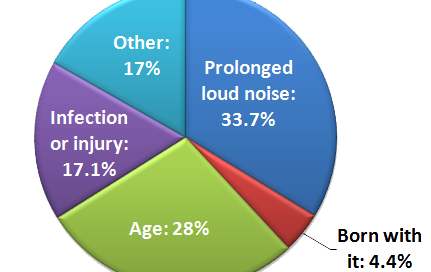
Why You Should Wear Earplugs at Ball Games & Other Sports
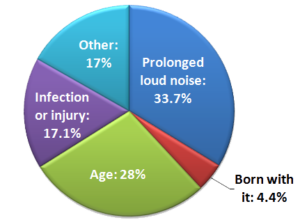
Hearing loss causes; which is No. 1?
The screaming at ball games and other sporting events is literally deafening, yet very few people think to wear earplugs at these events. You’re ruining your hearing.
The loud screaming, hollering and cheering at ball games and other sporting events not only can cause hearing loss, but just one game can damage hearing.
There are sporting events that have been studied for the very purpose of hearing loss from the loudness.
“To provide an example of one such event, a study of noise levels produced at an NCAA arena has shown that one-third of the participants tested over the course of three home games for the Murray State Racers were exposed to noise levels above the OSHA noise exposure limit of 85 dB for an average of eight hours,” begins Rivka Strom, AuD, CCC-A, chief audiologist at Central Hearing LLC in NY.
“OSHA is the Occupational Safety and Health Administration, and they set noise exposure limits for levels based on a timing factor,” continues Strom.
“The effect of noise induced hearing loss (NIHL) are potentially serious — and while spectators may realize these events are loud, they may not realize they are dangerous to the ears. Ear protection is a MUST at these events!”
One Sporting Event Is All It Takes to Damage Hearing
This is the finding from a study by Bill Hodgetts (U of A’s Faculty of Rehabilitation Medicine) and Dr. Richard Liu (Faculty of Medicine and Dentistry).
They measured noise levels at games 3, 4 and 6 of the Stanley Cup finals against the Carolina Hurricanes in 2005.
Don’t let that past date fool you; their findings still stand strong.
Results of Sound Level Meter Testing
It took under six minutes to achieve the maximum allowable daily dose of noise volume.
To put another way, every fan without earplugs got socked with about 8,100 percent of their daily noise dose.

The paper adds that fans aren’t the only ones at risk for hearing loss at sporting events; athletes and employees are as well.
One must wonder how damaged the hearing is of that brawny hockey player who proudly sports his permanently disfigured nose.
The study report points out that usually, fans’ ears will recover after one or two games.
But do you have season tickets or otherwise attend frequently? Whatever hearing loss you eventually develop will be connected to these games.
Who’d ever get caught dead wearing earplugs to a sporting event?
One woman posted in an etiquette forum that she nonchalantly popped in earplugs when the woman behind her began screaming blood curdles every time her team scored.
We all want to have fun and root for our teams. But must you sound like Fay Wray when she sees King Kong for the first time?
The woman with the earplugs never even turned to look at the screamer, yet the screamer became offended at the sight of someone in front of her putting in earplugs and began hurling obscenities.
Though the reaction by this nutcase is the exception, you should not hesitate to pop in earplugs. In fact, put them in as you take your seat rather than after the fact.
Just like you’d wear sunscreen to protect your skin while at the ball game, a cap to shield your eyes from glare, mittens to keep your hands warm, a scarf over your nose, and so on, why should earplugs be excluded from your arsenal of body protection?
Never mind what strangers, or even your own camp, might think.
You may need to loosen one or both plugs to fully understand conversation with your group amid a generally noisy atmosphere, but when conversation is finished you can just push the ear plugs firmly back in to protect your hearing.
The study appears in the 2006 Canadian Medical Association Journal.

Dr. Strom is a member of the American Speech Language and Hearing Association and has received several awards including Brooklyn College’s Excellence In Audiology Award.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources: sciencedaily.com/releases/2006/12/061206095322.htm; etiquettehell.com/smf/index.php?topic=112801.0
Supplement Pills Stuck in Chest Feeling: Solutions

Here’s how to prevent getting that pills stuck in chest feeling after taking several supplements at once.
Have you found that often, if not always, whenever you take your usual “handful” of supplement pills, that soon after, it feels as though they are stuck in your chest?
The stuck pill sensation can be described as being behind the breastbone (sternum) or somewhere in the esophagus — which is actually behind the breastbone.
The way to prevent the sensation that a cluster of supplement pills are stuck somewhere behind your breastbone or in your chest is to keep your head lowered a bit while swallowing the nutritionals.
This seems counterintuitive to the traditional way of swallowing a pill: tossing the head back while swallowing with the water.
Somehow we’ve been led to believe that tilting the head back will assist in getting something down the throat.
I was doing some online research into the issue of that stuck feeling in the esophagus, as this had been occurring to me (I take numerous supplements daily).
Tossing the head back narrows the passageway through which pills and food travel, and lowering the head, on the other hand, opens up the passageway more — thus creating an easier path for incoming pills to slide down.
If this still seems like it would cause you to choke, think of it this way:
When you eat food — meat, cereal, candy, a crunchy salad, munchies, a sandwich, a milkshake, soda — do you toss your head back every time you swallow a mouthful?
Of course not. Typically, when people eat, their head is straight ahead, or even tilted down somewhat, as in when they’re eating and reading a book or magazine at the same time! Yet they don’t choke.
Certainly you’ve eaten while your head was tilted downward, such as while looking at your computer keyboard, at your smartphone, etc., without gagging on the food.
Though a pill is a harder item that doesn’t get pulverized and pureed by our teeth and saliva before it slides down the throat, the principle still applies that keeping the head lowered while swallowing will help that supplement (capsule, gel cap or tablet) go down more efficiently.
So next time you take your supplement pills, keep your head lowered for every swallow.
For best results, drink some water ahead of time to lubricate the passageway, and make sure you drink a big glass of water (or fluid) with your nutritional supplements for optimizing the prevention of that stuck in the chest feeling.
Two More Solutions
“Feeling of pills stuck in the esophagus happens when the supplements are passed into the esophagus but are not moving into the stomach, causing discomfort and chest pain,” says Natasha Fuksina, MD, an internal medicine and obesity specialist who combines traditional, integrative and functional medicine to restore health and function.
“This can be alleviated by swallowing small amounts of warm liquids, sometimes with a small amount of soft food, which can help propel the stuck pills into the stomach.”
Second, you may want to consider spreading the intake of all of your supplement pills throughout the day rather than as a bunch in one sitting.
 Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/sirtravelalot
Noise Sensitivity ADHD: Real Illness or Product of Culture?
One of the symptoms of ADHD, according to WebMD, is the following:
“Easily distracted by irrelevant stimuli and frequently interrupting ongoing tasks to attend to trivial noises or events that are usually ignored by others.”
This describes me perfectly. However, this does not mean I have ADHD or some kind of problem or neurological issue.
People who’ve been diagnosed with “noise sensitivity” or “hypersensitivity to noise” due to ADHD would find that, in certain environments (e.g., out in the country), their alleged problem would be non-existent.
In a culture replete with relentless auditory stimuli, seems like the oddballs are people who CAN ignore it all.
If your coworker keeps repeatedly tapping their pen on the desk, or keeps making clucking and smacking sounds with endless gum chewing, and you find this disruptive to your concentration, WHO really has the problem?
Not you! This is an issue of being considerate vs. inconsiderate, not who might have ADHD (or ADD).
Some years ago I was repeatedly distracted by ongoing giggling of a young woman who was being taken on a tour of my workplace. For all I know, nobody could stand it.
But even if I’d been the only one, this doesn’t make me noise sensitive or ADHD.
Instead of wondering why I’d be the only one distracted by ongoing giggling (nobody was telling funny jokes; it was merely a tour), the better question is why was this woman giggling at everything?
Let’s look at some culture-based noises that people who’ve been diagnosed with ADHD are driven “crazy” by:
- loud high pitched beeps from vehicles backing out
- motorcycle engines and men fooling around with their car motors
- clocks clanging every hour
- ticking clocks
- hums from various machines (computers, lighting fixtures, ventilation, refrigerators, copy machines)
- chairs squeaking
- bus and car brakes shrieking.
What’s ADHD “noise sensitivity” today was non-existent 100 years ago.
The website for the Environmental Protection Agency identifies noise pollution as a real problem:
Noise pollution adversely affects the lives of millions of people. Studies have shown that there are direct links between noise and health.
Problems related to noise include stress related illnesses, high blood pressure, speech interference, hearing loss, sleep disruption, and lost productivity.
Noise Induced Hearing Loss (NIHL) is the most common and often discussed health effect, but research has shown that exposure to constant or high levels of noise can cause countless adverse health effects.
What about noise that’s been around since the beginning of time? That would be loud laughter, shrieking and screaming children, noisy eating, knuckle cracking, whistling and humming.
I once finally told a coworker that his incessant whistling was very annoying. This doesn’t make me ADHD. Brazen, maybe, but not ADHD.
More power to those who can tune out rude people.
But this doesn’t mean that others have ADHD or “noise sensitivity.” Like the EPA says, noise pollution is real.
I don’t consider myself ADHD just because I wear ear plugs at Whole Foods Market where piped in music blares and toddlers scream nearby, or at the gym where attention-seeking men smash metal weight plates into each other.
I don’t want noise induced hearing loss. This doesn’t make me ADHD.
I’m no more ADHD for wearing ear plugs to preserve good hearing than someone is for wearing sun block to protect their skin, or avoiding cigarette smoke to protect their lungs. Being health conscious does not make you ADHD.
The criteria for ADHD has been expanded over the years, and some of this involves how one reacts to noise.
If my reaction to unnecessary and offensive sounds (e.g., neighbor keeps revving up his thundering car engine over a 30 minute period just to play around with it, versus revving up a malfunctioning engine for a few minutes to get it going so he could drive to work) means I probably have ADHD, then that’s fine with me because it also means I’ll have great hearing well into old age since I make efforts to avoid loud or shrieking sounds.
There’s normal and necessary noise (lawn mower, carpet steam cleaner, crying infant or injured young child), and then there’s intrusive and unneeded noise (letting toddlers and preschoolers scream in stores, raucous laughter in the workplace, adults screaming over petty things, incessantly barking dog).
If you want to protect your hearing from harm and be a healthier person, this doesn’t mean you have “noise sensitivity” or ADHD.
UPDATE: In March 2022, the author of this article was diagnosed with Autism Spectrum Disorder — but not ADHD.
Though the autism explains getting distracted by irrelevant sounds that would not be noticed by other people, and finding some non-loud sounds to be very annoying — the desire to protect one’s hearing in loud environments to avoid future hearing loss is not indicative of a neurodivergent mind.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: ©Lorra Garrick
Sources: webmd.com/add-adhd/guide/adhd-symptoms; womenwithadhd.com/forum/topics/sensitivity-to-repetitive; epa.gov/air/noise.html#health
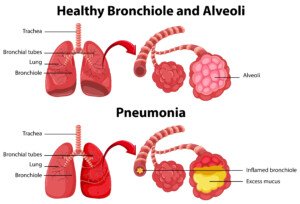
Cough Is Getting Worse: What Does an ER Exam Involve?
If you have a worsening cough, get to the emergency room because it can be serious; here’s what’s involved.
When my mother developed a cough with phlegm that sounded horrible — and after several days was only worse — I took her to the ER, suspecting pneumonia.
My mother was taken to a room in the ER, and soon the doctor appeared. The doctor asked her many questions.
If you go to the ER with a cough, the doctor will ask a lot of questions.
This includes if you have symptoms other than the cough such as fever or chills.
This helps guide the doctor in suspecting viral versus bacterial pneumonia.
“If a cough is rapidly worsening, it is crucial to seek medical attention promptly,” says Alice Benjamin, a clinical nurse specialist, and chief nursing officer and correspondent for nurse.org.
She explains, “Early intervention can lead to earlier diagnosis and initiation of appropriate treatment.
“Delaying medical care can allow the condition to worsen, potentially leading to more severe complications and a more challenging recovery.”
Pneumonia, which can be life-threatening at any age, isn’t the only potentially serious problem of a cough.
Benjamin points out that it may also be caused by congestive heart failure and lung cancer, though bronchitis can also be the culprit.
The doctor ordered a chest X ray for my mother, then had the nurse come in and give her a five minute albuterol treatment, in which she breathed into and out of a hand-held tube device that expelled vapors.
Vitals were taken, but a blood test was not taken (though lab tests are typically taken).
The doctor seemed very sure that the coughing was either from pneumonia or bronchitis.
In fact, after listening with a stethoscope, he said he heard wheezing, which he thought was likely caused by bronchitis.
The chest X ray showed “a little” pneumonia. The doctor then prescribed an antibiotic called Levoquin.
She was given one 500 mg pill right there (about 10 pm), then discharged with an albuterol inhalation pump.
The ER visit wasn’t that long, but of course, length of stay will depend on how busy the emergency room is, and whether a patient gets “bumped” by an incoming patient with a more serious presentation.
The ER facility need not be a hospital; it can be an urgent care facility, which is fully equipped to deal with cases of pneumonia.
I’ve taken my mother to an urgent care facility as well for a worsening cough.
An ER visit for a bad cough is well-worth the time investment.
A bad cough that goes untreated can turn out to be pneumonia, which the Centers for Disease Control says kills about 50,000 Americans a year.
“Visiting the emergency room for a rapidly worsening cough, especially for individuals over the age of 65, is important for several reasons,” says Benjamin.
“A rapidly worsening cough can be a sign of respiratory distress, which may result in decreased oxygen levels in the blood.
“Hypoxia (low oxygen levels) can be particularly dangerous for older adults and can lead to confusion, dizziness and organ damage.
“ER staff can quickly assess oxygen levels and provide appropriate interventions.”
Older adults are also at higher risk of developing serious complications from respiratory infections, but younger adults are not immune to this outcome, either.
“The ER is equipped to evaluate and manage these types of emergencies promptly,” says Benjamin.
 Alice Benjamin, APRN, is Chief Nursing Officer & Correspondent for Nurse.org. In addition to being a clinical nurse specialist and family nurse practitioner, she also has 20+ years of experience in critical care and emergency medicine, and gives podcasts on health.
Alice Benjamin, APRN, is Chief Nursing Officer & Correspondent for Nurse.org. In addition to being a clinical nurse specialist and family nurse practitioner, she also has 20+ years of experience in critical care and emergency medicine, and gives podcasts on health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Stockbakery
Sources:
my.clevelandclinic.org/heart/disorders/aorta_marfan/aneurysm_aorta.aspx
cdc.gov/Features/Pneumonia/
Cause of Blackout in Seemingly Healthy Elderly

Do you know an elderly person who blacked out for no apparent reason, with no history of fainting?
An elderly person apparently blacks out and falls. First of all, you need to determine — if possible — that they actually passed out while upright, versus lost their footing or a knee buckled and then fell.
I’d been staying with my elderly parents to care for them; my mother was experiencing severe pain from a herniated disc, and my father had just had knee revision surgery.
The knee rehabbing was going good; my father got around on a walker. Though there was a lot of post-surgical pain, he was stable with the walker.
Then a THUD! in the Middle of the Night
Eight days after the surgery, I heard a thud at 3:30 in the morning; my mother called out to me.
I dashed into my parents’ room and found my father prone (stomach down) on the floor, shoulders and head in the bathroom.
His surgical knee was over the walker, which was lying on the floor.
I removed it from under the leg, and my first thought was that the knee surgeon goofed up; the hardware suddenly loosened.
I got on my knees and within seconds realized my father was disoriented and belligerent (not his nature), and not responsive to my simple commands to alter his body position so that I could better assist.
He was holding his stomach off the floor; only his forearms, knees, thighs and feet were making contact, and he was stuck in this position.
I immediately knew that this fall had not been broken consciously as he went down, because:
1) He had altered mentation, indicative of a significant whack on the head, and 2) He had a purple and red “goose egg” hematoma on his forehead, indicative of a hard fall.
Based on his body position, he had fallen forward. Because the walker had been under his leg, this meant that, just prior to the fall, he had slumped forward over the walker, body weight crumbling on top of it as he pitched forward, knocking the device over as he fell over it.
Sleuthing 101: He’d had a blackout while standing, while using the walker to get to the bathroom.
He had passed out, then fallen. The knee could not have given way; otherwise, he would have supported himself on the walker and remained upright.
Knee pain would not have made him fall over the walker and end up prone on the floor, walker under leg. Pain would have simply made him safely shuffle back to the bed.
The floor was clear of obstacles; tripping was ruled out. He had blacked out.
Why would a seemingly healthy elderly person black out?
I also considered that my elderly father didn’t actually black out, but instead, became so dizzy or lightheaded that he fell forward, still conscious but not grounded enough to break the fall. I suspected a narcotic painkiller contributed.
I also suspected his high blood pressure drug, Lisinopril, which can cause fainting as a side effect.
It was more than a coincidence that a fainting spell occurred in that tiny sliver of time during which my elderly father got up in the middle of the night to use the bathroom; I suspected a big blood pressure drop caused by medications.
Emergency room personnel suspected a “cardiac event” because a blood test revealed that his troponin was elevated.
He was admitted to the cardiac unit. The follow-up troponin test yielded no upward trend, so heart attack was ruled out.
The doctor suspected one of three things:
1) A combination of dehydration, physical stress from the recent knee surgery, Lisinopril side effect and Flomax side effect.
My father had been taking Flomax for quite a while, and the doctor said it causes dizziness in 30 percent of patients.
2) Heart rhythm disorder, or 3) Heart valve problem.
A heart rhythm and valve disorder were ruled out with tests. Blood sugar was normal, ruling out diabetes. CT scan of head was normal.
The diagnosis of exclusion, then, for why my elderly father blacked out, was “the perfect storm” of recent knee surgery stress, lack of hydration, Lisinopril and Flomax.
The doctor took him off the Lisinopril and Flomax.
A week out from the blackout, he continued to sometimes experience the “room swirling” upon sitting up from a back-down position on his bed.
Takeways from a Medical Doctor
“To prevent from having a fainting episode, it’s important to make sure you maintain a good hydration status,” says Amber Robins, MD, a board certified family medicine physician in NY.
“A good way to tell if you’re hydrated is by looking at your urine. If it is yellow, this means that you may need to drink more fluids.

Shutterstock/gritsalak karalak
“Keep in mind that you can also overdo your hydration which could lead to other medical issues.
“This is where speaking to your primary care doctor about your particular medical conditions may be most appropriate.
“After a knee replacement or any surgery, a patient may also be on pain medications. For some, this can lead to feelings of dizziness which could lead to having a fall.
“Again, I would suggest talking with your doctor to discuss a regimen that may be best for you.”
Remember, if an elderly family member has had surgery, hydration is super important.
However, clear with the surgeon just how much water a day the patient should be getting.
And make sure that the family member is taking any medications in their proper doses.
 Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Photographee.eu
Sources:
drugs.com/lisinopril.html
mayoclinic.com/health/orthostatic-hypotension/DS00997/DSECTION=causes
Bad Cough in Elderly: When to Go to the ER
A bad cough in the elderly can mean pneumonia, a top killer of the elderly, so head to the emergency room promptly.
If an elderly family member (over age 65) has a cough that seems to be getting worse, take them to the emergency room, because this can mean pneumonia.
Pneumonia is the fifth leading cause of death in the elderly (over age 65).
“If there is fever, shortness of breath, and/or mental status changes, one should definitely visit the doctor’s office,” says Richard Honaker, MD, Chief Medical Advisor at Your Doctors Online, an online doctor chate site.
“If none of these are present, it is recommended to see a doctor if the cough lasts more than a week, is rapidly worsening, impacts sleep, is severe or is causing distress,” continues Dr. Honaker, who has 30+ years’ experience as a primary care physician.
My mother, whom I consider “young elderly,” developed a nagging cough that involved phlegm (a “productive” cough).
I didn’t think much of it since she felt fine otherwise, and has had coughs in the past.
“Because illnesses in older adults can be more serious and life threatening, I would suggest that they call their doctor who can then evaluate them and determine the appropriate next steps,” says Amber Robins, MD, a board certified family medicine physician in NY.
My mother called the Kaiser Permanente hotline to receive some advice from a nurse.
The nurse said that sometimes, it takes about three weeks for a cough (non-pneumonia) in the elderly to work its way out of the system.
That’s all the nurse said; just let it run its course. It seemed to run its course and apparently was out of my mother’s system.
A few weeks later I was visiting and noticed my mother was coughing quite a bit—the same type of cough, but very frequently and for lengthy episodes. She was hacking up phlegm.
I wondered if the previous bout had never really gone away, and instead whatever had caused it was still in her system, this time all fired up with a vengeance.
My father informed me that my mother had been coughing like this for the past three or four days.
Mistake
My father should have been more tuned into this problem and gotten my mother to the emergency room.
“Coughing in older adults can be due to several medical reasons that include both heart and lung disease,” says Dr. Robins.
Pneumonia, however, should always be considered even if the older individual does not have a chronic lung disease or a known heart problem. The earlier that pneumonia is treated, the higher the chance for recovery.
Freepik.com, brgfx
Instead, my father had believed that it was a mere resurgence of the cough of several weeks ago that the nurse hadn’t seemed too concerned about.
In fact, the nurse never even mentioned that it might be pneumonia!
Why didn’t the nurse say, “I can’t diagnose over the phone, but when an elderly person has a persistent or worsening cough, they should go to the ER to rule out pneumonia or a bronchial infection” ?
I couldn’t help but think about pneumonia, as the cough had a sinister sound to it. TRUST YOUR GUT.
I also had no reason to believe my elderly mother was immune to this infectious disease.
I said, “We have to get you to the ER. If this is pneumonia, it can be easily treated in the early stages.
“But if we don’t go to the emergency room, and this is pneumonia, it will progress beyond the point of no return.”
Well, that clinched it, and I took her to the ER, where the chest X ray confirmed “a little pneumonia.”
It was “a little” because I had gotten her to the ER early in the disease. Treatment was an antibiotic.
 Dr. Honaker has been recognized by D Magazine as one of the Best Doctors in Dallas several times and a Texas Super Doctor by Texas Weekly. He’s also a recipient of the Physician Recognition Award from the American Medical Association multiple times.
Dr. Honaker has been recognized by D Magazine as one of the Best Doctors in Dallas several times and a Texas Super Doctor by Texas Weekly. He’s also a recipient of the Physician Recognition Award from the American Medical Association multiple times.
 Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Ruslan Huzau
Sources:
seniorhealth.about.com/od/deathanddying/tp/cause_death.htm
mayoclinic.com/health/pneumonia/DS00135/DSECTION=symptoms
Pulmonary Embolism Tied to Excessive Sitting in Women

A pulmonary embolism is a blood clot in the lungs, and can be fatal within a minute, and for women who sit a lot on a daily basis, their risk is two to three times higher than in more active women.
This 2011 conclusion appears on the British Medical Journal website. An inactive lifestyle ups a woman’s risk of pulmonary embolism, plain and simple.
The conclusion was reached following an 18-year study of almost 70,000 female nurses who provided detailed information concerning their lifestyle.
In women who spent over 41 hours a week sitting, excluding at the workplace, the risk of pulmonary embolism turned out to be more than two times greater when compared to women who sat less than 10 hours a week, excluding at work.
Variables such as body mass index, age and smoking were adjusted for.
Not surprisingly, the investigation also revealed that a sedentary lifestyle correlated with high blood pressure and heart disease, and these conditions could quite possibly be driving forces behind pulmonary embolism.
There are a number of ways to reduce sitting time outside the workplace.
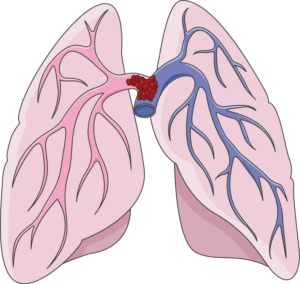
A “saddle” type pulmonary embolism, plugging up the area where the pulmonary artery splits off into each lung. This can cause death in minutes. Laboratoires Servier, CC BY-SA/creativecommons.org/Wikimedia Commons
If you’re concerned about pulmonary embolism, consider the following strategies for cutting back on the amount of time you spend sitting.
– Treadmill desk. A cheap model can serve as a desk for your computer at home, so that you can very slowly walk (sub-1 mph will do) while perusing the Internet.
– Set a timer for 45 minutes every time you sit before the computer. When it goes off, do something on your feet for several minutes.
– Stand while watching TV. This isn’t as dreadful as it sounds. You’ll get used to it. You need not stand still. You can march in place or tap your feet side to side, or pace frontward and backward for several steps.
– Pace while on the phone.
– Stand while going through the mail or eating a snack or even a bowl of cereal.
You should also be aware of how much time you sit at the gym, and I don’t mean during seated strength training exercises.
I mean in between sets.
Keep on your feet your entire workout, unless it’s time to lie down for a bench press or sit for an overhead dumbbell press or cable row.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik/8photo
Source: sciencedaily.com/releases/2011/07/110705071745.htm
Premarin vs. Estradiol and Blood Clot (DVT) Risk

Find out which poses a higher risk of a DVT blood clot: estradiol pills or Premarin pills.
To help manage menopausal symptoms, women can be prescribed estrogen-type pills, but these carry with them the increased risk of a deep vein thrombosis.
This is a type of blood clot that can dislodge and get into the lungs, fatally blocking air supply.
A new report in the JAMA Internal Medicine explains that in a study, women who took estradiol had fewer negative vascular events (such as a blood clot) when compared to those who took Premarin.
Premarin vs. Estradiol: DVT Study
The women in the study who did not develop a blood clot were also compared, in terms of their clotting factors.
The women on the Premarin, in this particular group, had increased clotting factors in their blood, than did women on the estradiol.
Plus, the Premarin users had a small increase in the risk of suffering a heart attack.
However, a difference in the risk of stroke was not observed.
Easing Menopausal Symptoms
So if you’re a woman who’s considering taking a pill to ease menopausal symptoms, you now have some information that should be helpful if you’re concerned about an increased risk of a blood clot, says the study’s first author, Nicholas L. Smith, PhD.
Symptoms of menopause include hot flashes, night sweats, vaginal dryness/burning/irritation, constipation and migraine headaches, says Mayoclinic.com.
The site also says that mood changes, sleep disturbances, thinning hair, dry skin, slowed metabolism and weight gain are also symptoms.
Many women prefer to manage menopausal symptoms with nutrition, supplementation and exercise, rather than take estradiol or Premarin.
But women who do take these hormone pills should know what the symptoms of a DVT are: swelling in one leg; redness and warmth in one leg; sudden cramping or pain that cannot be explained by recent exercise.

The leg on the right is affected by a DVT. Heilman, MD, CreativeCommons
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.