Do Minor TIA Symptoms Mean No Treatment Necessary?
A very brief transient ischemic attack is as much a medical emergency as is a full-blown stroke.
Sometimes, people who have experienced a transient ischemic attack (TIA) are not given clot busting drugs because their doctors don’t consider the condition serious enough to treat, says a study.
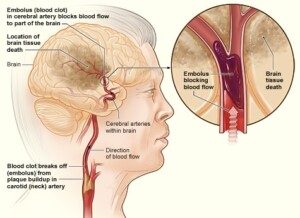
A TIA is a “mini stroke,” meaning, a blood clot forms in a blood vessel in the brain, blocking blood flow from that vessel to wherever in the brain it feeds. That portion of the brain then suffers.
However, a transient ischemic attack, like its name says, is temporary.
The clot dissolves, sometimes in under a minute, leaving the patient with no lasting effects; the patient may feel perfectly normal just a few minutes after a TIA.
A study at Foothills Hospital in Calgary, Alberta, Canada, shows that TIA patients, as well as those who had a minor stroke, are at a substantiail risk for disability and require early assessment and treatment.
No matter how minor the TIA symptoms are, the report says that early imaging of patients is crucial, and that the administration of clot busting drugs is critical if the imaging reveals a blockage in the brain.
TIA of One Very Brief Symptom vs. Full-Blown Stroke
These are equal to each other as far as degree of emergency: Get to the ER — even if what appears to be a TIA lasted only 20 seconds.
For instance, the inability to form words that lasts 20 seconds is just as much an emergency as the inability to use the right side of one’s body plus mental confusion plus double vision lasting three hours!
Whether it lasts 10 seconds or an hour, the same thing happens: a blood clot forms in the brain.
This is not something to take lightly, regardless of duration! The type of symptom is determined by the location of the stopped blood flow.
The study authors state that clot-busting treatment is not typically given because transient ischemic attacks are often deemed too mild to treat.
“Mild” TIA — is there a such thing?
“TIA is an emergency,” says Atif Zafar, MD, medical director of St. Michaels Hospital in Toronto, Ontario, and former director of the stroke program at University of New Mexico Hospital.
“If you are given a diagnosis of TIA, this means your physician is worried you have risk factors for a clot or plaque that are causing these neurological symptoms you’re complaining of,” continues Dr. Zafar.
“As a stroke neurologist, I take TIAs very, very seriously. However, if you present to the ED and your symptoms are mild and improving, we would consider holding [out] on the clot busting medication.
“Reason being, clot busting medication has a six percent chance of bleeding risks. So with you in the discussion, we have to weigh the risks and benefits of the treatment.
“Obviously, a very minor stroke with mild face numbness would not indicate the clot busting treatment if you were seen by me in the ED.
“Comprehensive TIA workup is needed to make sure we know where the clot or plaque is coming from, and how to ensure it wont act out again.
“TIA’s almost always require some change in treatment regimen. Blood thinner adjustment, cholesterol and blood pressure optimization are critical things your doctor will work with you on after a TIA event.”
A clot busting drug is not the same as a blood thinner such as Warfarin or Eliquis.
So even though you may not receive a clot busting drug, you’ll likely get a prescription for a blood thinner to take daily.
After all, if a TIA can happen once, it can happen again. The condition that causes a TIA is also perfectly capable of causing a massive stroke.
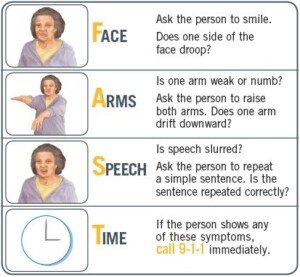
Remember “FAST” if you suspect a TIA or stroke.
More About the Study
The study involved 499 patients. Fifteen percent had at least a minor disability 90 days following their transient ischemic attack.
CAT scans revealed that some of the transient ischemic attack patients’ brains had narrowed blood vessels.
Other patients reported continuing or worsening symptoms.
These individuals were more than twice as likely to suffer disability at the 90 day mark.
For those particular patients, clot busting treatment should be considered.
After all, for every second following a transient ischemic attack, the brain may be losing oxygen.
In 2009, the American Heart Association and the American Stroke Association urged immediate action plus thorough testing for a transient ischemic attack — tests that are very similar to those given after a full-blown stroke.
The report reminds people that even though TIA symptoms “may pass quickly,” you should “immediately go to the hospital” to get the proper scans.
Dr. Zafar is author of the book, “Why Doctors Need to Be Leaders.” His interests include vascular and endovascular neurology, and the neurosciences.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Source: sciencedaily.com/releases/2012/09/120913162437.htm
Best Exercise to Lower Stroke Risk in Stressed People
Are you constantly under stress and worried about getting a stroke?
The good news is there’s a certain kind of exercise that will dramatically lower your chance of getting a stroke.
This type of exercise is called “hormonal.”
I’m a former certified personal trainer and I highly recommend this type of exercise that raises levels of anabolic hormones that counteract the stress hormones that thicken the blood.
What a Doctor Says
“The stress response, triggered by fear, stimulates a profound and sudden flooding of stress hormones, adrenaline and cortisol, into our blood stream,” says cardiologist John M. Kennedy in an interview for a previous article of mine.
A report in the August 2012 Journal of Neurology, Neurosurgery and Psychiatry says that chronic stress, fueled by a major life stressor and a Type A personality, is a high risk factor for stroke.
The Type A personality is the hard-driven, aggressive type, quick to show anger or get into arguments, and prone to fuming in stressful situations.
Though one might argue that this type of personality is also at higher risk for engaging in behaviors that increase stroke risk, such as smoking, drinking and eating junk food, the study (Egido et al) showed that stress is an independent risk factor for stroke.
National Heart Lung and Blood Insitute
Exercise will make a difference, but not just any exercise; it must be “hormonal” exercise — the type of exercise that triggers elevated secretion of human growth hormone (HGH) and testosterone.
These hormones oppose cortisol, the “stress hormone,” and adrenalin.
What is hormonal exercise?
Hormonal exercise helps unthicken the blood that stress thickens. When we are under chronic stress, our body prepares for a fight or flight.
The blood thickens and the blood platelets get sticky (making it more clottable) to protect us from bleeding to death from a gash during the fight or flight.
Problem is … with modern man, the fight or flight never happens.
Instead we remain immobilized in a traffic jam, an office cubicle, a business meeting — places where we can’t act out physically.
Stroke in the Making
Our blood stays thickened and sticky. If your blood remains this way chronically, you are at much higher risk of ischemic stroke (blood clot in the brain), since thick blood is more prone to clotting!
“Getting stuck in traffic can lead to increases in stress hormones which over time can wreak havoc on our cardiovascular tissue,” adds Dr. Kennedy, medical director of preventative cardiology and wellness at Marina del Rey Hospital, and author of the book, “THE 15-MINUTE HEART CURE: The Natural Way to Release Stress And Heal Your Heart In Just Minutes A Day.”
This is why blood thinning drugs are recommended to people at risk for stroke. Another way to “unthicken” blood is via hormonal exercise.
The intense physical exertion from a fight or flight releases HGH and testosterone. These cancel out the stress response that thickens the blood.
In a modern society, fight or flight exercise comes in two forms, both of which incite the hormonal response that opposes stress hormones:
High Intensity Interval Training and Heavy Weightlifting
- Jogging for an hour won’t cut it.
- Standing on wobble boards and pressing little dumbbells overhead won’t cut it.
However, dashing up a few flights of stairs as fast as possible while holding a 10 lb. dumbbell in each hand (or faster without a weight) will spark a completely different environment in your body that will immediately start going to work at hacking away at the stress hormones.

Intense exercise, aka “hormonal,” is a huge weapon against stroke, especially in stressed people.
In a nutshell, hormonal exercise consists of very brief bouts or bursts of HIGHLY INTENSE exertion, alternating with a few minutes or even five minutes of casual effort.
Imagine, for example, sprinting up a hill, multiple staircases or bleacher steps as fast as you can, boom boom boom — until you just can’t take another step.
You then pace very slowly while you gasp for air, letting your body recover. After several minutes you go all-out again — for only 15 seconds, maybe 30 seconds.
This type of workout is often referred to as either high intensity interval training or burst exercise.
Resistance Training and Stroke
Heavy weightlifting such as an eight repetition max of an all-body exercise such as the deadlift will also help lower the risk of stroke in stressed men and women.

Other great exercises include any kind of pulling, such as pulling resistance down from above yourself while in a seat, or pulling resistance horizontally towards yourself while in a seat; and any pressing motion such as a dumbbell press.
Don’t forget the legs; any type of squat works very well, as well as the leg press and sled push.
Exercises like this will change the hormonal environment in your body and protect against chronically thickened blood that leads to blood clots in the brain: stroke!
 Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Sources: sciencedaily.com/releases/2012/08/120829195207.htm; http://www.cdc.gov/stroke/facts.htm
Does Stress Change the Brain to Cause a Stroke?

Could it be that chronic stress creates adverse changes in the brain that eventually lead to a stroke?
An ischemic stroke is a blood clot in the brain that shuts off oxygen supply to the area that the blocked vessel feeds.
If you think that mental stress that causes heart disease can then trigger a stroke from the heart, wait till you find out about a Swedish study that implies that stress does something to the brain that makes a brain-originating stroke more likely.
The type of stroke in this study was the blood clot kind: A blood vessel in the brain gets a clot that obstructs blood flow to whatever part of the brain that the vessel feeds (also known as a cerebral infarction).
This is more commonly called an ischemic stroke, and the clot can originate from the heart (usually from diseased arteries; the clot in this case is a coronary plaque fragment that travels “upstream” from the heart and gets into the brain).
Or, the clot can develop in a blood vessel of the brain itself.
The study comes from the Sahlgrenska Academy at the University of Gothenburg and Sahlgrenska University Hospital, Sweden.
Neurologist Katarina Jood says that interpreting the correlation between mental stress and stroke must be done very cautiously, because for the study, patients who’d had a cerebral infarction were questioned (within 10 days of hospital admission) about their stress levels in the five years prior to their cerebral event.
The problem is that a cerebral event can alter one’s perception or memory of their recent past.
Nevertheless, about 600 patients were asked to fill out a questionnaire, to rate their stress levels over the preceding five years.
Their responses were compared to those of a healthy control group who filled out the same questionnaire.
Findings
There was an independent link between self-perceived mental stress and stroke.
However, this correlation wasn’t the same for the three kinds (in terms of origin) of ischemic stroke that were studied.
– Stress and cerebral infarction were linked when the stroke was caused by blood clots that developed in the brain.
-Stress and cerebral infarction were linked when the stroke was caused by blood clots of undetermined origin.
-Intriguingly, this study did not show a correlation between stress and stroke when the clot originated from the heart.
(Tests are used to determine the origin of the blood clot.)
Might this mean that chronic stress has an adverse effect on blood flow in the brain?
The study was not able to determine why stress seems to play a bigger role in particular kinds of stroke.
Nevertheless, stress and stroke are intertwined.
Your Stress Response

Shutterstock/Charnchai Saeheng
“The stress response stimulates a profound and sudden flooding of stress hormones, adrenaline and cortisol, into our In the modern world, however, the stress response gets triggered much more often – not by saber toothed tigers but by things such as forgetting to pay a major bill, a visit to the dentist or MRI machine, or hearing your boss say in an unpleasant tone, “I need to see you in my office.”
The result, over time, is increased inflammation, high blood pressure and heart rate, and the increased ability of blood to form clots.
“These physiologic changes create the perfect storm for a stroke,” says Dr. Kennedy.
The risk of atherosclerosis goes up. This condition causes plaque formation in blood vessels.
“Eventually, these changes damage the delicate inner lining of blood vessels and lead to a heart attack or stroke.”
 Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
Double board certified in cardiovascular disease and also internal medicine, Dr. Kennedy’s special interest is stress and how it adversely affects a person’s delicate cardiovascular system.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik,katemangostar
Source: sciencedaily.com/releases/2009/10/091001101502.htm
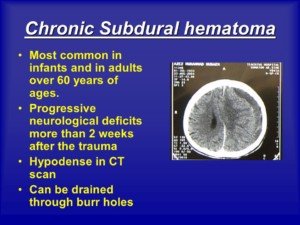
What Happens in the ER for a Chronic Subdural Hematoma?

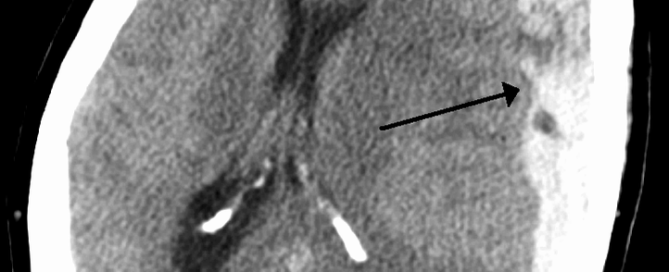
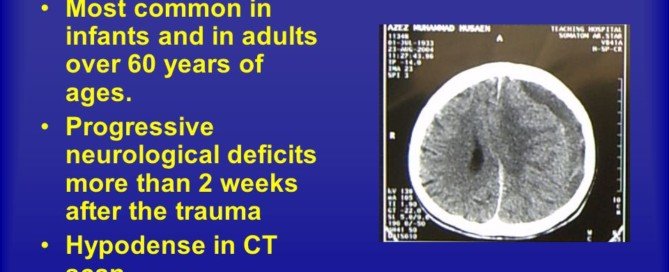
The diagnosis of a chronic subdural hematoma in the emergency room is easy to make: A CT scan easily reveals the collection of blood. But what happens once this diagnosis is made?
My mother went into the ER with alarming symptoms and was ultimately diagnosed with a chronic subdural hematoma.
You may have heard of the words, “subdural hematoma,” and think that this is always an emergency situation that can kill in minutes.
However, there are three kinds of subdural hematoma, says MedlinePlus: acute, subacute and chronic.
Symptoms can occur immediately after a head trauma, or not show up for a few months after the head trauma.
In my mother’s case, the symptoms began appearing six weeks after she fell and hit her head.
In the ER, the doctor suspected a stroke (she had lower body weakness, more so with the left leg, and a bad headache) and didn’t even mention chronic subdural hematoma. A CAT scan with contrast dye was ordered.
Meanwhile the ER doctor gave my mother a neurological exam which included things like asking her to lift her legs against the doctor’s hand resistance.
The CAT scan revealed the chronic subdural hematoma (blood in the brain leaking from torn veins).
In my mother’s case (I am not speaking for ANY or ALL cases of chronic subdural hematoma), she was admitted to the neurology unit of the hospital, and told that she would have surgery the following morning to drain the blood.
I asked why was there a delay; won’t it get really worse overnight? The doctor said that if it were an emergency, they would not wait till next morning to operate.
It was not an emergency and it was not expected that the situation would deteriorate overnight. The doctor believed that my mother’s condition was stable, and told me throughout the night she’d get neurological checks by the nurses.
This was the first time I’d ever learned of the “chronic” type of subdural hematoma.
I’d always believed that if symptoms of a hematoma began weeks after the head trauma, that the situation was just as potentially fatal as when the symptoms occur rapidly right after the head trauma.
The idea of a very gradual, slow leakage of blood had never occurred to me, probably because I first learned of “subdural hematoma” after watching a clip of a boxer receiving the “fatal blow” in a professional match, knocking him out cold.
This had fascinated me because the boxer wasn’t just unconscious, but his body was rigid (“posturing”) as the medics cumbersomely hoisted him (though he was extremely thin) onto the stretcher. This stuck in my mind.
However, when the ER doctor said my mother had a “chronic” subdural hematoma, I instantly realized that this was a less serious form, not to be compared to the one that the boxer had suffered.
A neurosurgeon was contacted and the surgery was tentatively for next morning. The ER doctor was not able to give fine details other than explaining that the procedure involved drilling a hole in the head and draining the fluid.
Though this sounds invasive, the surgery is actually non-invasive and minor. The ER doctor said it was a 10-minute procedure.
My mother was transferred to the neurology wing and set up in her room. Next afternoon she had the surgery which involved general anesthesia, but the neurosurgeon indeed said it would take about 15 minutes and he didn’t seem the least bit worried, as though this was not much more than wrapping a sprained ankle.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: James Heilman, MD/CreativeCommons
Sources:
nlm.nih.gov/medlineplus/ency/article/003300.htm
nlm.nih.gov/medlineplus/ency/article/000781.htm
Chronic Subdural Hematoma: tPA plus Blood Thinners in Stroke Patients

Here’s information concerning risk of chronic subdural hematoma resulting from tPA combined with blood thinners in stroke patients.
Many men and women take blood thinning drugs to help prevent stroke.
Thicker blood is more likely to form dangerous clots, but thinner blood is more likely to cause bleeding in the body, such as a “chronic subdural hematoma.”
This is slow bleeding in the brain; patients over age 65 are at greatest risk compared to other age groups.
Suppose you’re on blood thinners but you have a stroke anyways. Prompt medical treatment will include tPA: a potent clot-busting drug.
But you already have blood thinners in your system, so won’t the addition of tPA put you at risk for a subdural hematoma: a brain bleed?
A new study from the University of Michigan Stroke Program says that risk of brain bleed, under these circumstances, is low for most patients on blood thinners.
The investigation looked at data from 830 patients who’d received tPA for their stroke.
A little under 50 percent of these patients had been on the blood thinner Plavix, or aspirin, prior to their stroke.
After adjusting for variables, the researchers found no substantial difference in the rate of brain bleeding, based on brain scans. This included low-level bleeding that produced no symptoms.
Patients, plus ER teams, need to be reassured that administering tPA to stroke patients, who already have blood thinners in their system, isn’t dangerous or likely to cause bleeding in the brain. The full report is in the March 2013 Academic Emergency Medicine.
Patients Over Age 81 Had Small Increased Risk
The report mentions, however, that patients over 81 did sustain a small increased risk of brain bleeding, though non-symptomatic.
Which blood thinners?
The study examined patients on aspirin and Plavix, not the stronger blood thinners like heparin, warfarin (Coumadin), Pradaxa or Xarelto.
Unfortunately, the study team says that giving tPA to stroke patients on these stronger drugs needs more investigation.
“In light of the long-term benefit that patients receive from antiplatelet therapy,” says lead author William Meurer, MD, “the small increase in risk of intracranial hemorrhage after tPA treatment should not be a game-changer for emergency physicians.”
Dr. Meurer, assistant professor of emergency medicine at U-M Medical School, adds that this study shows that doctors should not hesitate to give tPA to stroke patients who’ve been taking aspirin or Plavix.
A “chronic” subdural hematoma is when the brain bleed doesn’t happen within several days of the causative agent, and instead, begins showing signs or is detected on scan anywhere from a few weeks to 90 days out.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: James Heilman, MD/CreativeCommons
Sources:
sciencedaily.com/releases/2013/03/130313095301.htm
pmj.bmj.com/content/78/916/71.full
Most Common Symptoms of Chronic Subdural Hematoma in Elderly
The most common symptoms of a chronic subdural hematoma in the elderly differ from those in younger patients.
“A chronic subdural hematoma is a collection of blood on the brain’s surface, under the outer covering of the brain (dura),” says Sashini Seeni, MD, a family medicine practitioner with DoctorOnCall, an online doctor and pharmacy.
“It is a common neurological condition affecting the elderly,” continues Dr. Seeni.
The chronic nature means this situation begins showing symptoms at least a few weeks after the head trauma (which in elderly people, may be quite trivial such as banging their head on a car door frame when getting into the vehicle).
“Chronic subdural hematoma enlarges from recurrent bleeding in the subdural space which comes from the leakage of blood of a torn vessel into a space below the dura mater,” explains Dr. Seeni.
The Postgrad Medical Journal (2002, Vol. 78) provides an extensive list of symptoms pertaining to chronic subdural hematoma in the elderly.
Altered Mental State
An altered mental state is the most common presentation, says the PMJ paper.
This occurs in 50-70 percent of patients. The alteration in mental status can mimic delirium or dementia, says Dr. Seeni.
“Thus, they should be considered in the differential diagnosis of elderly patients presenting with neurological signs and symptoms.”
My elderly mother had a chronic subdural hematoma twice: the initial one and a recurrence about 10 days later.
Her mental state with the first one seemed normal, though it was odd that she wasn’t alarmed over her severe leg weakness.
Her mental state with the recurrence was altered: a mild level of impaired reasoning.
The PMJ list includes confusion, drowsiness and acute delirium.
As my mother’s recurrence unfolded, she developed acute delirium, but the ER doctor attributed this to an adverse reaction to the Medrol Pak (oral steroid drug to reduce brain inflammation).
Unconsciousness is another possible symptom of chronic subdural hematoma in the elderly.
Focal Neurological Deficit
This is the next category of most common symptoms of chronic subdural hematoma in elderly patients.
One study, as reported in the PMJ, found that 58 percent of elderly patients suffered weakness on one side of the body. My mother had it in both legs.
Focal (confined to a specific part of the body) deficits will usually remain persistent, rather fluctuate, says the PMJ.
My mother’s significant leg weakness never subsided prior to treatment.
However, it’s not known how insidiously it developed because at around 7 a.m. that morning, she reported feeling normal when she arose to use the bathroom.
She returned to bed and around 10:30 a.m. got up, and that’s when a mobility problem was quite obvious.
Headache
“The pressure of hematoma in the subdural space causes the headache in the elderly,” says Dr. Seeni.

Shutterstock/Prostock-studio
Headache incidence varies from 14-80 percent depending on the study, says the PMJ.
My mother’s initial occurrence included a “crown of thorns” headache, as she had described it at the time.
Though headache is the third category of likelihood of symptoms reported in the PMJ, a headache is a less common symptom in the elderly than in younger people with chronic subdural hematoma.
This is because there’s less space in the bigger brain of a younger person for the fluid buildup to occur.
Falls
A study of 43 elderly patients found that falls occurred in 74 percent, notes the PMJ report.
Ironically, falling as a symptom of cSDH can make the cSDH worse.
Falls as a symptom may result from neurological deficits, altered mental state or postural disturbances.
Seizures
Seizures are a rare symptom of chronic subdural hematoma, though patients with pre-existing epilepsy may have increased seizure activity with a cSDH.
A chronic subdural hematoma can produce a simple partial seizure as its only symptom. This can mimic a transient ischemic attack.
Transient Neurological Deficits
The PMJ says the incidence of TNDs is 1-12 percent. In the elderly the most common TND symptom from chronic subdural hematoma is one-sided paralysis or numbness.
There’s been at least one case reported of on-and-off partial paralysis of the lower limbs due to a cSDH on both sides of the brain.
Rare Symptoms of Chronic Subdural Hematoma in Elderly Men and Women
Vertigo; fast, uncontrollable eye movements; tremoring (Parkinson’s-like); right-left disorientation; unawareness of one’s fingers; inability to write; inability to do simple math; and slowly tilting towards a fall without making postural adjustments due to unawareness of this.
My mother’s recurrence of chronic subdural hematoma produced a most intriguing symptom: left side neglect.
A person with severe left side neglect may refuse to believe that their left leg and arm are theirs.
My mother would make right turns when told to go walk left, and would try to pick things up with her left hand and miss the object, yet think she had it in her hand!
My mother eventually fully recovered from both her chronic subdural hematomas.
 DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: pmj.bmj.com/content/78/916/71.full
Doctor Didn’t Warn of Future Brain Bleed when CT Scan Was Normal

My elderly mother’s doctor didn’t warn her that she could get a chronic subdural hematoma even though her head CT scan was normal.
Elderly age plus head trauma = fair chance of developing a chronic subdural hematoma, and this chance jumps when the elderly individual is on the blood thinner Coumadin at the time of their fall.
It has long been recognized that elderly individuals are more likely to develop a subdural hematoma (brain bleed), particularly from minor trauma.
“As we age our vessels age with us,” says Reena Patel, MD, a board certified family medicine physician who treats patients at Garnet Health Urgent Care in NY.
“Our capillaries, arteries and veins harden — some more than others, depending on history of hypertension, hyperlipidemia and overall health/genetics.
“Some may even experience decrease in overall brain size. This makes it easier for vascular injury.
“A small vessel in the brain can have a break, leak or tear that over time can cause a deep impact.”
Shrunken Brain
When aging causes the brain to shrink, this increases the amount of space between it and the skull from 6% to 11% of the total intracranial space. The bridging veins then stretch.
The brain can move more due to the increased space, and this makes these veins more vulnerable to tearing from getting hit in the head or hitting the head from a fall.
Every elderly patient who has a normal CT scan following a fall or other hit to the head should be warned to be on the lookout for future symptoms.
“Symptoms of a slow brain bleed can include: headache (most common), neurological deficits such as weakness in a limb, balance issues or paresthesias, slurring of speech and confusion, to mention a few,” says Dr. Patel.
Normal Head Scan but Brain Bleed Weeks Later
My elderly mother had a normal CT scan, and then another one 24 hours after that, following a fall and visible injury to her head.
I asked the ER doctor, “What about the chance that a few months down the road, there’s bleeding in her brain?”
The doctor said, “There’s a very slim chance of that.”
Six weeks later my mother awakened with a searing headache and significant lower body weakness, out of the blue.
A CT scan later in the day showed a chronic subdural hematoma.
At the time of her fall, she still had Coumadin in her system (she’d gone off it the day prior).
The original ER doctor had actually known she was on Coumadin.
This doctor never told my elderly mother about the blaring risk factors for a chronic subdural hematoma: hit on head (it’d even been bloodied), elderly age and Coumadin!
Several years later my father had an apparent blackout while standing and fell face down.
He was on Coumadin. The fall resulted in a “goose egg” purple and red swelling on his forehead.
Nobody at the ER informed him that there’s a fair chance that a few weeks or months down the road, he may develop symptoms from a chronic subdural hematoma.
Of course, I then knew this already, and was vigilently on the lookout for neurological symptoms in the ensuing weeks.
“The CT scan is normal,” was all my parents got.
Because elderly patients may not get a warning about chronic subdural hematoma, they and their family often don’t have a clue what’s going on weeks or up to three months later when the neurological symptoms start developing.
The symptoms of these brain bleeds can mimic dementia, stroke and mini-stroke.
If you’re elderly (or know someone who is) and have recently hit your head, and the CT scan was normal, even one 24 hours later — consider the next few months as an incubation or grace period for the development of a chronic subdural hematoma.
In addition to treating many chronic conditions, Dr. Patel treats urgent conditions that affect every part of the body. Instagram: That_dr_next_door
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Source: pmj.bmj.com/content/78/916/71.full
Recurrence of Chronic Subdural Hematoma Missed by Doctor?

Seemed the neurosurgeon was wrong and the layperson was right about recurrence of chronic subdural hematoma.
A neurosurgeon didn’t think my mother’s new symptoms were the result of a recurring chronic subdural hematoma.
My mother awakened one morning in 2011 with neurological symptoms.
Later that day a CT scan showed bleeding in her brain: a chronic subdural hematoma. The next morning it was surgically drained via burr hole.
The neurosurgeon said there was a 15 percent chance of recurrence. A study by Byung-Soo Ko et al says the recurrence rate is 3.7 to 30 percent (after burr hole drainage).
For another article I wrote regarding chronic subdural hematoma and recurrence, I interviewed Kangmin Daniel Lee, MD, a neurosurgeon with New Jersey Brain and Spine.
I asked him about the typical time passage between a primary cSDH and its recurrence (re-bleeding at the surgical drain site).
Dr. Lee explains in that article: “There is some variability with this number depending on the technique, but most recurrences, when it does occur, will happen in the short term. Most published reports range it from the 1-3 week period.”
Chronic Subdural Hematoma Recurrence?
Around 10 days after my mother’s initial draining, she began exhibiting suspicious symptoms.
For example, she began dropping things. She also could not (with eyes open) join the ends together of two paper cups after bringing them towards each other with outstretched arms.
She also couldn’t join her hands in a clap position from an outstretched position.
Believing a recurrence of the chronic subdural hematoma, I reported these deficits to the neurosurgeon. He doubted a rebleed.
I gave my mother more tests, including picking a straw up from a table with her left hand.
She’d attempt to grab the straw but miss it. She’d pull her pants up after using the toilet, but only on the right side, unaware that the left side (including underwear) was still down as she walked away from the bathroom.
My mother was also experiencing escalating headaches. A follow-up CT scan (to the initial burr hole draining) had already been scheduled (and was still several days out).
On Jan. 23, four days prior to a follow-up appointment in his office, I again spoke to the neurosurgeon.
He insisted that there was no recurrence of the chronic subdural hematoma. He then said that sometimes the elderly get weakness in an arm.
Since when is literally grasping for straws and missing them a sign of muscle weakness?
And what about the other symptoms, such as unawareness that her underpants and pants were not pulled up on the left side?
This sure sounded like a recurrence of a chronic subdural hematoma rather than age-related weakness.
I had also described to him the inability to join the paper cups or her hands. I also pointed out that these symptoms were of a relatively sudden onset (several days). The neurosurgeon said, “If you’re concerned, take her to ER.”
He said that headaches normally don’t occur post-drainage procedure, but offered nothing else at that point other than to take her to the ER if she “deteriorates rapidly,” but otherwise, to keep things on schedule.
Results of that follow-up CT scan: The neurosurgeon’s colleague called me and said that the neurosurgeon said there was “nothing significant,” no “significant” mass, and the midline shift appeared normal or unchanged.
I managed to get the follow-up office appointment moved from Jan. 27 to Jan. 26.
Then the neurosurgeon’s physician’s assistant contacted me that the CT scan was “worse” but also “improved” in that the volume of fluid was greater, but density less. There was no new bleeding, however.
According to a report in Advances in Neurosciences and Clinical Rehabilitation, a CT scan can “miss” a chronic subdural hematoma (depending on type) that an MRI can easily show.
This makes me wonder why an MRI was never ordered for my mother.
The neurosurgeon finally confirmed that the increased fluid volume was causing the excruciating headaches and impaired left hand.
When I referred to the left hand malfunction as “significant,” the neurosurgeon promptly corrected me by saying it was mild or not significant, compared to what he sees in other patients, and that “significant” was total paralysis.
I had to bite my tongue hard to keep from criticizing his blasé attitude and inappropriate reference to “other patients.”
After all, I didn’t want to lose brownie points with a doctor who was probably going to be draining my mother’s brain again.
He offered my mother a choice between a Medrol Pak (oral steroids) or a second burr hole draining.
She chose the Medrol, but the redraining was scheduled in case the Medrol didn’t work.
The Medrol didn’t work. Next day my mother underwent the second burr hole draining.
After the procedure the neurosurgeon told me that there was a “new bleed.” I wondered if this “new bleed” was actually a recurrence of the original chronic subdural hematoma. I’ll never know.
What a coincidence that a “new bleed” popped up within that one to three week period following the burr hole draining of the first chronic subdural hematoma.
I have never doubted the meaning of that old adage, “Eighty percent of medicine is common sense.”
Dr. Lee focuses on minimally invasive techniques to treat traumatic and degenerative diseases of the spine and brain tumors. He’s been invited to speak at the regional and national levels on his research areas.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Dr. Miki Katzir, CreativeCommons
Sources:
ncbi.nlm.nih.gov/pmc/articles/PMC2588154/
acnr.co.uk/ND08/ACNRND08_management.pdf
Is Leg Swelling After Knee Replacement Always DVT?

Have you had knee replacement surgery, and have noticed that the other leg seems to be getting bigger or swollen in appearance, even though after the first several days following the operation, it looked as it always had?
One of the leading risk factors for a deep vein thrombosis is knee replacement surgery, says Mayoclinic.com in the site’s DVT section.
If you’re familiar with deep vein thrombosis, you already know that a classic sign is swelling of the leg — a key symptom noted by Mayoclinic.com.
The site says that knee replacement surgery can cause a DVT because of debris that forms during the procedure that can get into the venous system.
Another cause is general anesthesia in combination with post-surgical immobility.
My father had knee replacement (revision) surgery. Five days after the surgery, I thought I began noticing that his non-surgical leg was a tad smoother than it usually looks, especially around the ankle, but I thought it was my imagination.
I’d been watching the non-surgical leg like a hawk since the surgery, so I knew exactly what it was supposed to look like.
Five days after the knee surgery, I took him to the ER upon the advice of his surgeon when the physical therapist suspected an infection.
I asked the nurse and the ER doctor if the non-surgical leg “looked fine,” and they both said it did, even though, by golly, I couldn’t help wonder if I wasn’t imagining things as I studied the leg from behind while my father shuffled with his walker.
The day before this, he had stopped wearing the “anti-emboli” ted hose.
Next day, there was no doubt; the leg was swollen, including the foot and toes.
Even my father admitted it. I was thinking, a DVT has formed because he removed the ted hose the other day.
His primary care doctor wasn’t at all concerned and said it was edema from excessive inactivity. Why did this not occur sooner; why five days later?
Most likely because he’d been wearing the ted hose continuously up till a few days prior.
Once he removed them, the edema (excess fluid in a limb) had a chance to build up. The ted hose (a.k.a. compression stockings) prevented this.
“Half of all DVT cases cause no symptoms,” says WebMd.com. Don’t be led astray by a doctor who makes it seem as though you can’t possibly have a deep vein thrombosis just because there’s no pain or redness with your leg swelling.
WebMD.com lists the following as DVT symptoms: swelling in the leg; tenderness or pain in the leg (may occur only when standing or walking); excessive warmth in the leg; red or discolored skin in the area; visible veins; undue fatigue.
If your non-surgical leg is swelling after knee replacement surgery (even if there’s no pain or redness), or the surgical one is swelling more and more, especially if initially the swelling was going down, get medical attention promptly.
Don’t assume it’s just edema from inactivity. Let a doctor tell you that.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Dave Haygarth
Sources:
mayoclinic.com/health/deep-vein-thrombosis/DS01005
webmd.com/dvt/deep-vein-thrombosis-dvt-symptoms-diagnosis
Barbell Squat vs. Dumbbell Squat for Building Mass: Pros & Cons

Barbell squats or dumbbell squats: which is better for building muscle mass?
The barbell squat and dumbbell squat both have plenty to offer fitness enthusiasts.
When I was a personal trainer at a gym, I’d occasionally be asked which was “better.”
Whether the barbell squat is better than the dumbbell squat, or vice versa, depends upon your goals.
Some people wish to build a lot of muscle mass/size in their upper legs and glutes.
Barbell Back Squat vs. Dumbbell Squat for Mass Building
The ability to build a lot of muscle mass in the legs and buttocks is not possible with dumbbell squats, because with dumbbell squats, you are required to support the dumbbell weights with your hanging arms as you hold onto them.
This is a problem for people who can barbell squat a lot of weight. For instance, suppose you can barbell squat 225 pounds 10 times.
To duplicate this resistance for your legs and butt, with dumbbell squats, you’d have to hold a 110 pound dumbbell IN EACH HAND while lowering into the squat position.
Your legs may be strong enough to support the weight with 110-pound dumbbell squats, but for many people, their upper body will not be able to hold onto those weights.
Women, especially, will find it too much to hold a 100-pound dumbbell in each hand.
In fact, I’d be willing to bet that extremely very few women, who can barbell squat 200 pounds, can maintain holding onto 100-pound dumbbells in each hand for the duration of eight dumbbell squats.
And if all a man can barbell squat is 200 pounds, I can pretty much guarantee that his upper body strength isn’t all that impressive, either, and hence, 100-pound dumbbell squats will be very difficult for his upper body to sustain.
Though a 200-pound barbell squat is impressive for a woman, it’s nothing to brag about for a man.
And then there are men who DO have impressive barbell squats, let’s say 315 pounds. How could he duplicate this effort with the dumbbell version?
First of all, what gym supplies 150-pound dumbbells? Of course, you can purchase these online, but come on.
Secondly, the heavier the dumbbells, the more that the upper body must get involved for these kind of squats.
If the weight is heavy enough, dumbbell squats will simply become impractical. They are not ultimate mass builders.
But don’t underestimate dumbbell squats for building fitness and durability in your legs.

Shutterstock/Jasminko Ibrakovic
Obviously, they are not the choice for building maximum size, maximal muscle mass or maximum strength in the legs.
But I’d like to see one of these men, who can barbell squat 400 pounds, do 30 repetitions of dumbbell squats on an air cushion, holding just 25-pound weights in each hand, reaching down so that their femurs are parallel to the floor — each time.
I can tell you right now, such a beast with the barbell squats will be screaming in pain by the 20th rep — if he even gets that far.
High rep dumbbell squats can be tweaked: Hold the down position for a 2-count and thrust quickly up to the upright position to recruit fast-twitch muscle fibers.
Don’t hang out at the top position; immediately drop down again and hold thighs parallel to the floor for two seconds. Do this 30 times with 20-pound weights on a flat surface.
If you think that was nasty, do it on an air cushion or the flat side of a BOSU board. Good luck.
Summary: When it comes to barbell squats vs. dumbbell squats for building a lot of mass, forget the dumbbells and do the back squat.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.