Why Does Basal Cell Carcinoma Affect the Nose so Much?
Why is it that whenever you hear that someone has basal cell carcinoma, it seems that it’s always on their nose? (more…)
Carnivora vs. Youngevity: Which Is Better for Health?
Are you a “Coast” listener who keeps getting bombarded with the ads for Carnivora and Youngevity?
Which of the two is more hype? Which of the two should you choose if you could only choose one? (more…)
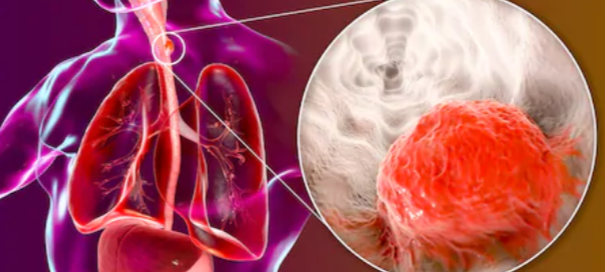
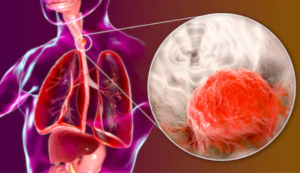
How Long Can Lung Cancer Go Undetected?
Ever wonder for how long lung cancer can grow before it’s detected by a doctor or before the patient begins feeling the symptoms?
“There are two approaches to think about this,” says Alex Little, MD, a thoracic surgeon with a special interest in esophageal and lung cancer.
“The first is to ask how long it takes to cause symptoms and for a symptomatic patient to seek medical attention,” continues Dr. Little.
“Reported numbers differ, but one well-done study (Japanese Journal of Clinical Oncology 1994;24:199-204) found the doubling time for all lung cancers to be 166 days, for adenocarcinoma of the lung to be 222 days, and 115 days for squamous cell lung cancer.”
What does that mean?
For instance, it takes 166 days on average for lung cancer cells to grow from four cells to eight.
Or, it takes 222 days for 32 adenocarcinoma cells of the lung to multiply to 64 cells.
This may seem like the cancers grow very slowly. But this growth is exponential, not linear.
The more that something is doubled at fixed intervals, the faster it gets bigger.
“These data suggest it would take a single malignant cell several years before it would become large enough or be in the opportune location to cause symptoms — such as shortness of breath (most common and very non-specific) or chest pain — that would send a patient to a physician,” explains Dr. Little.
Several years may seem like a sweet slow time for cancer to grow, but once it starts causing symptoms, that doubling growth rate skyrockets.
After 222 days, a five centimeter adenocarcinoma will be 10 centimeters! That is a LOT.
“And more stoic patients will delay medical attention longer than others,” continues Dr. Little.
“The second is to speculate how long it would take for the physician seeing such a patient to evaluate for lung cancer with a chest X-ray.
“It can take some time. As you know, most patients are smokers [around 85%] and have some degree of emphysema which can cause shortness of breath without lung cancer being present.
“This can delay the search for a lung tumor. As for patients with pain, again, there are plenty of reasons for chest or shoulder pain other than lung cancer to attribute the pain to before looking for lung cancer.”
Lung cancer, in uncommon cases, can actually cause shoulder pain if the tumor is in the top of a lung lobe, pressing on a nerve that leads to the shoulder.
“So, more time goes by,” continues Dr. Little. “This is why early detection screening in asymptomatic patients at high risk (smokers over age 55) using low dose CT scans to minimize radiation exposure are now recommended.
“Since a lung cancer can be growing without killing the patient, it probably could be present for even a few years before detection — depending on location, amount of spread, patient stoicism and physician response.”
If all of this scares the pants off of you, then STOP SMOKING.

Freepik.com
And if you’ve never smoked and are feeling “pressure” to take up this nasty-smelling, very pricey habit – then keep repeating the following mantra in your head:
“No person on this planet has ever regretted NEVER having become a smoker.”
Then make a list of all the harmful things that’ll come your way if you do NOT give in to the “peer pressure” to smoke.
Ask yourself if any of those things will matter six months from now, even three months. Even three weeks.
Though lung cancer may seem like a distant future to you as a young smoker, keep in mind that stinky breath, skin, hair and clothes are always smack in your present.
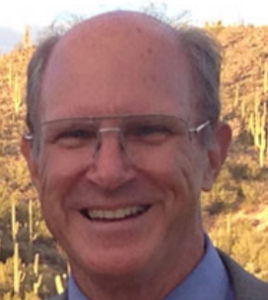 Alex Little, MD, trained in general and thoracic surgery at the Johns Hopkins University School of Medicine; has been active in national thoracic surgical societies as a speaker and participant, and served as president of the American College of Chest Physicians. He’s the author of “Cracking Chests: How Thoracic Surgery Got from Rocks to Sticks,” available on Amazon.
Alex Little, MD, trained in general and thoracic surgery at the Johns Hopkins University School of Medicine; has been active in national thoracic surgical societies as a speaker and participant, and served as president of the American College of Chest Physicians. He’s the author of “Cracking Chests: How Thoracic Surgery Got from Rocks to Sticks,” available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
How Long Can Esophageal Cancer Go Undetected?
How long can an esophageal cancer be growing inside you before it can be detected?
The answer is frightening. (more…)
Why Aren’t All Child Sex Abuse Victims 600 Pound Adults?
Many patients on “My 600 Pound Life” were sexually abused as children, yet most sexually abused children don’t become morbidly obese. Why? (more…)
Why Strangers’ Self-Love Sticky Notes Don’t Help Self-Esteem
Are those anonymous self-love sticky notes in public places overrated?
Or can they really undo the source of a woman’s poor self-esteem?
The person who wrote the “You are worthy” note has never seen you, let alone interacted with you to get a feel for your personality and social skills.
A fair question, then, is how can this phantom person’s little message actually make a woman’s day? And if it does, does this mean she has frail self-worth?
What matters is when a person who’s important to us and a part of our lives says we’re worthy and values our company and thoughts.
If a woman didn’t get this from her parents during childhood, a stranger’s note isn’t going to heal her — though it may uplift her for the next hour or so.
“Generalized self-esteem stickers are about as useful as motivational posters are in workplaces,” begins Patricia Celan, MD, a senior psychiatry resident at Dalhousie University in Canada.
Dr. Celan explains, “There is very limited research on their effectiveness, but the research available for motivational posters indicates that they may possibly have an impact on some employees – not all.
“The same can be assumed for self-esteem stickers. They can trigger a child [or adult] to be reminded of a helpful conversation they had previously, a pep talk that inspired them to think differently about themselves.
“However, unless a self-esteem sticker happens to strike a nerve, we can speculate that generic ones mostly have no effect.
“Even if a child disagrees with the sticker, there is no evidence that these stickers may cause harm such as cementing the negative self-talk.
“Certainly, a sticker has not caused any epiphanies or cured anybody with low self-esteem, as the only way to permanently feel better about yourself is to either seek extensive therapy or find interests, achievements and personal self-improvement.
“These stickers either have no effect on the vast majority of people, or they may inspire some people by reminding them of positive thoughts that they already had from previous experiences but had forgotten.”
Relationship with Parents
If you didn’t feel validated by your parents, and/or if older siblings belittled you, bullied you or otherwise behaved in a way that made you feel worthless INSIDE, how is it possible that a total stranger’s self-worth Post-it Note on a public mirror is going to fix your inner wounds?

Shutterstock/Volodymyr Baleha
Yet apparently, it actually happens – at least on a transient and superficial level.
But if repeated invalidations by family members throughout the developmental years have left a young woman feeling inadequate, “not worthy,” not good enough, dislikeable, defective or too weird for anyone to want to be friends with … these wounds cannot be mended by mere notes by strangers.
Criticisms or negative comments by the parent during childhood don’t necessarily relate to body weight or physical appearance, and in fact, often do NOT.
This is why even kids with conventionally attractive bodies and faces can still grow up feeling awful inside.

Freepik.com
Feeling unworthy as an adult has origins in childhood and is years in the making. A sticky note in public isn’t going to fix this.
If a sticky note in public makes your day, that’s great. But it only makes one’s day. Or maybe hour.
There’s something deeper going on when you need a self-worth note by a stranger, who’s never met you, to feel better about yourself.
That deeper issue needs to be pursued so that you no longer need an anonymous person’s note to feel a transient worthiness.
 Dr. Celan is a post-graduate trainee in psychiatry, working in diagnosing and treating patients with psychiatric conditions. She is passionate about psychotherapy, especially in trauma, anxiety and depression.
Dr. Celan is a post-graduate trainee in psychiatry, working in diagnosing and treating patients with psychiatric conditions. She is passionate about psychotherapy, especially in trauma, anxiety and depression.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
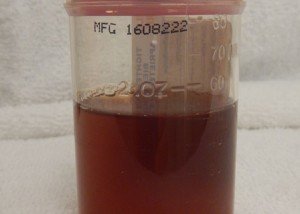
Hydrated but Urine Is Still a Deep Amber Like a Sunset?
You’re nowhere near dehydrated yet your urine is a brilliant amber and leaves salmon-orange stains on the tissue paper when you wipe!
There’s a most likely cause. (more…)
Body Image, Planning Your Workouts and Getting the Results You Want
Scheduling your workouts is NOT a sign of poor body image or lack of self-love.
Keep scheduling your gym time, treadmill time or fitness video time, whatever your mode of exercise is.
Some “self-love” and body-positive influencers tell their followers that they shouldn’t schedule workouts.
You should not take this advice.
Of all the things you schedule in your life…why should exercise be left out of this practice?
What DO you think it’s okay to schedule?
• Bath time for the kids
• Feeding time for the baby and older children
• Housecleaning
• Balancing the checkbook
• Reviewing expenditures for the household
• Oil changes for the car
• Showering
• Shaving the legs
• Washing the hair
• Haircuts
• Walking the dog
Do you do any of the above only when “you feel like it”? Of course not! There is a component of scheduling to every one of those tasks.
Without any scheduling, there’d be big problems, not to mention filthy hungry children and hairy legs.
There Is No Evidence that Scheduling Workouts Prevents Self-Love or Body Positivity

Freepik.com/ senivpetro
When I was a personal trainer, my clients’ workouts were scheduled. Well, of COURSE they were, because I was providing a service, and they were my business clients.
But that aspect aside, having them work with me two or three times/week on the same days and at about the same time helped train their mind to assimilate the concept of sticking to a fitness regimen.
If you decide to do your workouts “whenever you feel like it,” guess what will happen!
Remember what I said about filthy kids and hairy legs? Not to mention a dog pooping all over the house and an overdrawn checking account.
Important events need to be scheduled: business meetings, PTA meetings, HOA meetings, doctor appointments, job interviews, and on and on.
So to think that an appointment to do your body good should not be scheduled is utter madness.
If you refuse to schedule your workouts, you’ll end up not doing them often enough to progress in your level of fitness.
If you want to increase your cardiovascular fitness, muscle and joint strength, low back and knee integrity, improve glucose metabolism, improve bone composition, enhance vascular health, firm up and lose body fat – you absolutely MUST schedule your workouts.
Just like you schedule your pedicures, manicures, haircuts, teeth brushing and anything else in life.
Spontaneous Unplanned Workouts
Hey, I’m all for spontaneous, non-scheduled ventures of physical activity such as that unplanned bike ride, zip-about on your inline skates, hike or some spur-of-the-moment sprints down the street.
But these would be in ADDITION to scheduled exercise sessions. Without scheduling you’ll lose sight of commitment, focus and progress.
Aim for at least three structured exercise sessions scheduled per week.
If something comes up and you miss one of these workouts, then you should do it the next day.
But to eliminate scheduling altogether? This is utter nonsense.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Why Seana’s Story on 600 Pound Life Is One of the Saddest
Seana’s story on “My 600 Pound Life” ranks as one of the saddest and bleakest for several reasons.
At only 22 she was seemingly destined for success with Dr. Now’s program.
(more…)
Joyce, 600 Pound Life: How Much Is Her Mother to Blame?