Trouble Breathing Your Through Nose? Should You Worry?

Difficulty breathing through the nose can be a pretty frightening experience when you swear you don’t have typical nasal congestion.
What may initially come to mind is the onset of a heart attack, since most people know that the so-called shortness of breath is a common symptom of a heart attack — as well as chronically clogged coronary arteries.
Breathing Problem: Trouble with the Nose
“Shortness of breath” is not the same as the sensation that despite deep breaths, you’re just not getting in enough air.
Trouble breathing that feels as though it’s originating in the nasal passages is probably exactly that: an obstruction in the sinuses or nostrils.
“The causes of nasal obstruction are two: structural and congestion,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
“Most people have a combination of both,” continues Dr. Silvers. “Structural causes are a deviated septum (which everyone has to one extent or another).
“The septum is simply the cartilage and bony wall that separates the right nostril from the left nostril. It is the tent pole which holds up the nose.
“The second structural blockage can be large adenoid tissue. The adenoids are the ‘tonsils’ behind the nose; they are lymphatic tissue which typically gets smaller as a person ages.
“If enlarged into pre-teen, teen years or adulthood, they can affect the nasal breathing and quality of life and may need to be removed.
“The third structural blockage can be nasal polyps. These form from severe allergies and are an overgrowth of the mucosa in the nose forming single or multiple nasal polyps.
“Congestion, most typically, can be caused by allergy or a virus. This is when the tissues in the nose swell as a response to allergy or viral nasal inflammation.
“Structural blockages can be surgically corrected. Congestion causes need medications.”
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vladimir Gjorgiev
Hoarse Voice Causes: from Cancer to Reflux to Enlarged Aorta

A hoarse voice can have many causes, and this includes acid reflux, laryngeal cancer and an aortic aneurysm.
Have you been bothered by a hoarse voice lately that doesn’t seem to have a cause such as excessive yelling or a cold?
A hoarse voice in the morning is normal, but what about in general?
“Many things can cause hoarseness,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
“Laryngitis (viral inflammation of the vocal chords); vocal cord nodules or polyps; long-term smoking irritates the vocal cords causing chronic swelling; vocal cancer, and very commonly acid reflux,” continues Dr. Silvers.
“Acid from the stomach comes up and irritates the back of the throat, causing it to swell. This swelling affects the quality of the voice and causes hoarseness.”
Acid reflux is also known as GERD: gastroesophageal reflux disease.
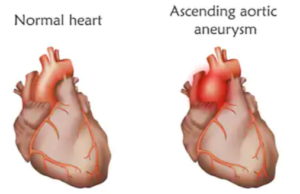
A thoracic aortic aneurysm, though not a likely cause of a hoarse voice can still cause a hoarse voice.
An aneurysm is a dilated (enlarged) or ballooned portion of an artery.
Shutterstock/Veronika Zakharova
The nerve that innervates the vocal cords passes near a section of the ascending aorta, the great vessel (largest in the body) that branches out from the heart.
If part of this vessel, in this location, is enlarged or bulging, it could make contact with the nerve.
So if you’re a nonsmoker and an ENT doctor tells you your vocal cords look normal, that you don’t have GERD or an infection, you haven’t been doing any shouting, yet the hoarseness just won’t go away, it may be time to visit a cardiologist.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Aaron Amat.
Source: stanfordhospital.org/healthLib/greystone/heartCenter/heartConditionsinAdults/thoracicAorticAneurysm.html
Foul Taste in Back of Throat: Causes, Solutions
If you suffer from a foul taste in the back of your throat, read what this ear, nose and throat doctor has to say about this annoying problem.
Have you been suffering from a foul taste in the back of your throat, even though this cannot be explained by anything you’ve eaten or otherwise ingested?
“Foul taste in the throat can be from: chronic sinus problems, acid reflux or tonsil stones,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
Tonsil stones can result, says Dr. Silvers, from the buildup of mucous and old food in the tonsil cavities.
These tonsil stones, also known as tonsilloliths, are small, calcified formations that develop within the crypts or crevices of the tonsils.
Over time, these materials can become trapped in the tonsil’s natural folds and pockets, where they gradually undergo a process of mineralization.
As the debris continues to collect and the stones increase in size, they can contribute to discomfort, bad breath and a sour or foul taste in the back of your throat.
As gross as this sounds, the good news is that it’s not a serious issue such as cancer.
Sinus Infection
“A chronic sinus infection can have a sour tasting mucous that can drip in the throat; more severe foul taste is noted with an acute infection,” contiues Dr. Silvers.
Acid Reflux
“Acid reflux causes stomach acid to come up, causing many patients to experience a sour taste and bad breath.”
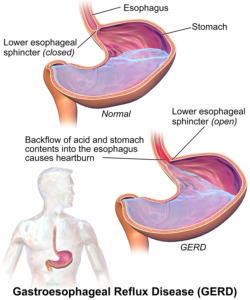
Acid Reflux. Image: BruceBlaus
Another cause of a foul taste in the back of the throat can be stress and anxiety.
Dr. Silvers says that stress is a major contributing factor to the issue of acid reflux.
When you get stressed out, this triggers a cascade of responses in your body.
One of these responses includes an increase in stomach acid production.
The body’s stress response can lead to elevated levels of hormones such as cortisol, which in turn can stimulate the stomach to produce more acid than usual.
As the production of stomach acid increases, the likelihood of acid reflux also rises.
When the acid levels become too high, the lower muscle at the bottom of the esophagus, that adjoins the stomach, may not be able to hold back the acid.
The result? This acid gets past the muscle and into the esophagus.
But the refluxed acid can also get up into the throat, leading to that foul taste in the back and even in the mouth itself.
When acid travels up to the throat and causes symptoms (including a lump feeling, cough and burning sensation), this is called laryngeal-pharyngeal reflux (LPR).
Hiatal Hernia
The annoying symptom of a bad taste in the throat can also be caused by a hiatal hernia, which can cause or aggravate GERD and LPR.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/puhhha
Constant Throat Clearing: Causes, Solutions

An ear, nose and throat doctor explains causes of constant throat clearing, and what can be done about this.
Constant throat clearing isn’t just a nuisance to you if you suffer from this, but it’s also a nuisance to all the people around you who hear it.
“Chronic throat clearing is from acid reflux,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
“Acid from the stomach comes up and irritates the back of the throat,” continues Dr. Silvers. This results in swelling.
“The mucous drips in the back of the throat causing post-nasal drip,” continues Dr. Silvers.
“This mucous is protecting the throat from the acid which will otherwise cause throat ulcers.
“The mucous is annoying, however, and causes an individual to clear their throat constantly, or intermittently to speak, depending on how bad the reflux and how much protective mucous is produced as a result.
“Stress is a big contributing factor to acid reflux,” adds Dr. Silvers.
“Stress will increase the production of stomach acid and the acid can reflux up.”
The more acid in your stomach, the more refluxed acid there will be if the conditions are ripe for reflux in the first place, such as having a weak lower esophageal sphincter (LES).
The LES is normally tight and keeps acid in the stomach where it belongs.
Tourette’s syndrome can also be a cause of the constant or frequent clearing of the throat.
Symptoms of Tourette’s syndrome can be very mild and are often misdiagnosed as other conditions.
Tourette’s syndrome is a neurological disorder characterized by repetitive, involuntary movements and vocalizations known as tics.
These tics can range from simple motor tics, such as blinking or head jerking, to more complex movements and vocalizations like making sounds and repeating words or phrases.
The onset typically occurs in childhood, with symptoms often becoming noticeable between ages five and 10.
It’s also not impossible for autism to be a cause of frequent throat clearing in the absence of a cold, allergies or acid reflux.
In this case, the behavior would be what’s known as a stim: self-stimulatory behavior or repetitive movements — usually for self-regulation. This cause, though, would be at the bottom of the list: possible, but highly unlikely.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Asier Romero
Source: mayoclinic.com/health/tourette-syndrome/DS00541/DSECTION=symptoms
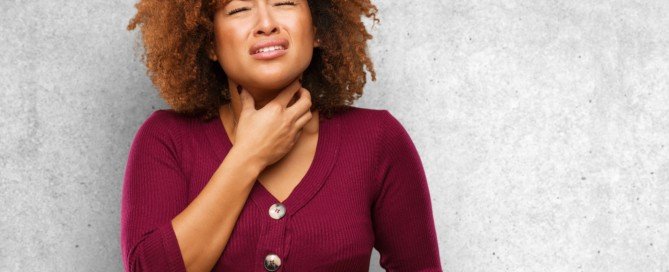
Choking Sensation in Throat: Causes, Solutions

An ear, nose and throat doctor explains the causes of a choking sensation in the throat, and what you should do.
Have you been experiencing a choking feeling or sensation in your throat?
“The most common cause of a choking sensation, without a known foreign body incident, is acid reflux, ‘silent reflux’ with our indigestion or heartburn symptoms,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
“Acid from the stomach comes up and irritates the back of the throat,” adds Dr. Silvers. This causes it to swell.
“This makes it hard to swallow and gives a feeling of a lump in the throat.
“Patients may describe shortness of breath, a choking sensation or trouble swallowing.
“Stress is a big contributing factor to acid reflux. Stress will increase the production of stomach acid and the acid can reflux up.”
Have you noticed that the choking sensation or feeling in your throat tends to subside or even disappear during times that you’re relaxed or absorbed in concentration? This is a tip-off that it’s stress-related.
Signs the Choking Sensation in Your Throat Is Serious
You may have a serious condition that warrants medical attention if the choking sensation in your throat occurs only when you’re trying to swallow food.
This is especially concerning if over a short period of time, the ability to clear food from your throat becomes increasingly difficult, such that you’ve begun switching to more soft foods in your diet.
Another worrisome sign is if the choking feeling comes with new symptoms that seem to be related.
Examples are trouble with speech, a buildup of saliva, a cough that won’t go away, and pain in an ear.
Tests that a doctor will order include an upper endoscopy, a barium swallow, a chest X-ray, pulmonary function and allergy testing.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
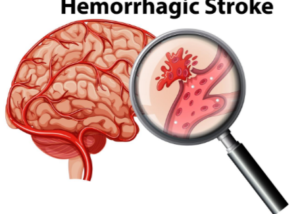
Brain Aneurysm: Surviving a Rupture with Fast Treatment
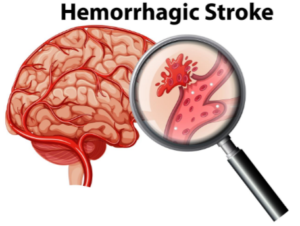
Often, a ruptured brain aneurysm means quick death, and if not, permanent brain damage. But these burst blood vessels do not always have to be lethal.
Surviving a Ruptured Brain Aneurysm
“The sooner the presence of an aneurysm is detected, the more likely it is to be successfully treated,” says Dr. Ezriel Kornel, a neurosurgeon with Somers Orthopaedic Surgery & Sports Medicine Group in NY.
“With a ‘full’ rupture, symptoms range from sudden death to coma to impaired level of consciousness, impaired speech and impaired motor function to simply an excruciating headache that does not let up,” continues Dr. Kornel.
What is the ruptured aneurysm (hemorrhagic stroke) headache like?
Dr. Kornel explains, “Always, it starts with a ‘thunderclap’ headache. About 50 percent of individuals with a full rupture of a cerebral aneurysm die before reaching a hospital, especially in more remote areas.
“A favorable outcome is certainly more likely if the aneurysm is discovered before there is a rupture that results in neurologic deficits.
“Over 60 percent of aneurysms are now treated by coiling, a procedure by which a very fine catheter is introduced into the aneurysm via arteries from the groin, into the head, and tiny ‘coils’ are injected into the aneurysm, filling it and causing it to clot off rather than bleed.
“Those aneurysms that cannot be coiled require clipping of the aneurysm microsurgically via a craniotomy.”
 Ezriel Kornel, MD, FACS, is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments. Known for his pioneering contributions to minimally invastive surgery techniques, he has developed and patented several innovative instrumentation methods that substantially reduce surgical trauma and enhance recovery times.
Ezriel Kornel, MD, FACS, is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments. Known for his pioneering contributions to minimally invastive surgery techniques, he has developed and patented several innovative instrumentation methods that substantially reduce surgical trauma and enhance recovery times.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image credit: Vecteezy.com
How Long Can Brain Aneurysm Leak or Bleed Before Bursting?
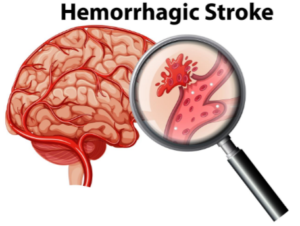
Could a brain aneurysm slowly leak or bleed for a few weeks before rupturing?
To find out if a brain aneurysm could slowly bleed or leak over a period of up to three weeks before finally rupturing, I interviewed Dr. Ezriel Kornel, a neurosurgeon with Somers Orthopaedic Surgery & Sports Medicine Group in NY.
Devastating Misdiagnosis
I was inspired to write this article after proofreading a medical malpractice deposition transcript, in which the plaintiff’s persistent headache was diagnosed by a doctor as a sinus issue, when in actuality, it was related to an aneurysm in her brain.
More than two weeks later she had a seizure, and it turned out that she had suffered a ruptured brain aneurysm.
She survived but with a permanent disability related to her eyes plus dizziness.
Had the brain aneurysm been slowly leaking or bleeding all this time?
“Aneurysms don’t ‘slowly’ leak,” says Dr. Kornel. “What is referred to as a sentinel bleed is an initial very small rupture of an aneurysm that immediately seals itself.
“The sudden expansion of an aneurysm without bleeding may also cause a headache.
“In any case, the initial symptom is a sudden, substantial headache that may linger for hours or days but is not unbearably profound.
“The initial headache is often described as the worst headache of their life.
“The neck may feel achy and stiff as well and light may be bothersome. There may be nausea as well.
“However, speech and mentation are preserved as is movement of the face and limbs.”
The plaintiff also experienced ptosis—a drooping upper eyelid. It never dawned on her to insist upon an MRI of her head, even when she began developing visual problems.
Dr. Kornel explains, “An expanding aneurysm of the posterior communicating artery can cause pressure on the third nerve which impairs the nerve’s function.
“This results in dilatation of the pupil which can result in blurry vision and ptosis or drooping of the eyelid.
“Also, eye movements are limited in the affected eye, so the individual can develop diplopia or double vision.
“All these symptoms with exception of third nerve compression can last for days or weeks and may never be followed by a ‘full’ rupture of the aneurysm.
“However, often, when we see a patient with a ‘full’ or substantial rupture of a cerebral aneurysm, if they give us a history of a prior headache, it is generally a few days to a week or two earlier.”
A brain aneurysm is also known as a hemorrhagic stroke. There are different ways to treat this potentially life threatening condition.
 Ezriel Kornel, MD, FACS, is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments. Known for his pioneering contributions to minimally invastive surgery techniques, he has developed and patented several innovative instrumentation methods that substantially reduce surgical trauma and enhance recovery times.
Ezriel Kornel, MD, FACS, is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments. Known for his pioneering contributions to minimally invastive surgery techniques, he has developed and patented several innovative instrumentation methods that substantially reduce surgical trauma and enhance recovery times.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image credit: Vecteezy.com
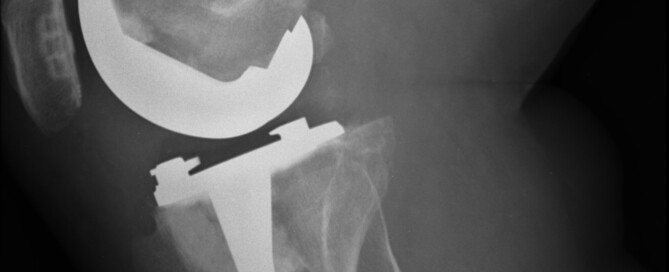
Are You At Risk for a Failed Knee Replacement Joint?

Despite how common total knee replacement is, many patients end up with failed or loosened hardware that causes pain and crashes their hopes of regaining mobility.
Approximately 50,000 people in the U.S. are diagnosed with a failed total knee replacement each year.
Revision surgeries are often required to address the malfunctioning hardware.
Risk Factors for a Failed TKR
“Oftentimes, we don’t know why they loosen,” says Jeffrey A. Geller, MD, Associate Chief, Division of Hip & Knee Reconstruction; Director, Minimally Invasive Hip & Knee Replacements, Columbia University Medical Center, NY, NY.
“It is assumed that some combination of prolonged time since surgery, and active lifestyle, leads to a process where the cement de-bonds from the bone.
“Rarely, prosthetic design may be inferior, leading to earlier loosening, but most popular designs have done well with good medium to long-term results reported in the scientific literature.”
A failed knee replacement can also result from infection or misalignment.
Symptoms of a Loosened Knee Replacement
Pain and swelling in the affected joint
Pain upon sitting and standing
Pain while walking
A sensation of warmth or heat at the knee
A feeling of instability when standing or walking
The symptoms may not occur for a while following the surgery, and thus, the patient may not make the connection, and instead blame the pain on other factors such as nerve compression in the back, which can actually cause pain in the knees.
Nerve compression in the back, particularly in the lumbar (low back) region, can certainly cause knee pain.
This occurs when nerves exiting the spine become pinched or irritated, often due to conditions like herniated discs or spinal stenosis.
The compressed nerves can radiate pain down the leg, sometimes manifesting as knee pain despite the issue originating in the back.
This referred pain is a result of the complex nerve pathways and how they interact with different parts of the body.
Since the replacement surgery may initially be successful, it can take quite some time before the patient realizes the possibility that perhaps the knee replacement has become loose or in some way is not working properly.
The pain can radiate beyond the knee and up the thigh, mimicking iliotibial band syndrome, as well as mimicking the pain in the upper legs that can result from spinal stenosis (narrowing of the spinal canal).
 Dr. Geller specializes in arthritic disorders of the hip and knee. He has extensive training in joint replacements and performs surgery using some of the latest, most advanced minimally invasive techniques.
Dr. Geller specializes in arthritic disorders of the hip and knee. He has extensive training in joint replacements and performs surgery using some of the latest, most advanced minimally invasive techniques.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can a Loose Knee Replacement Be Fixed Conservatively?

If you have a failed or loosened knee replacement, wouldn’t it be fantastic if this could be fixed without surgery — a conservative treatment that can resolve this problem?
To go through another invasive surgery, in which the failed parts are removed and a whole new artificial joint is put in its place, is just too daunting to even think about for many patients.
Knee replacement revision surgery involves replacing some or all of the prosthesis, and this doesn’t paint a pretty picture for patients who face once again going under the knife and having general anesthesia for the three hour operation.
And then there’s another several months of rehabilitation to go through all over again.
Bad News for Those with a Failed Knee Replacement
“If a patient with a loosening knee replacement absolutely cannot have surgery due to multiple medical problems, the only thing that may provide some modest degree of relief will be some type of brace and activity modification, i.e., limited walking,” says Jeffrey A. Geller, MD, Associate Chief, Division of Hip & Knee Reconstruction; Director, Minimally Invasive Hip & Knee Replacements, Columbia University Medical Center, NY, NY.
Dr. Geller explains that the brace requires a prescription. “It is usually fitted and dispensed by a brace specialist, called an orthotist.”
The brace, of course, will not repair a loosened knee replacement hardware. It may only take the edge off of the pain.
What about pain pills?
Pain medications can be limited in their ability to obstruct the pain, as well as be troublesome if the patient experiences unpleasant side effects. Dr. Geller adds that nerve or pain blocks are temporary and not effective.
About 20,000 or so knee replacement revisions are performed in the U.S. every year.
And some end up loosened or failed — and sometimes the reason is not clear why.
Unfortunately there is no way other than surgical to fix this, and the revision surgery may result in yet another failed replacement.
 Dr. Geller specializes in arthritic disorders of the hip and knee. He has extensive training in joint replacements and performs surgery using some of the latest, most advanced minimally invasive techniques.
Dr. Geller specializes in arthritic disorders of the hip and knee. He has extensive training in joint replacements and performs surgery using some of the latest, most advanced minimally invasive techniques.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, peoplecreations
Can a Single Fasting Glucose Over 100 Mean Prediabetes?
Did you get one fasting glucose reading over 100 and under 126 and are now panicking that diabetes will soon be a part of your life?
“One individual reading of a fasting glucose over 100, does not impart a diagnosis of prediabetes,” says Richard Kelley, MD, a practicing physician in Texas for 20+ years, and author of “The Fitness Response,” “The Three-Hour Appetite” and the ebook, “The Fitness Response ‘Diet’ for Women.”
Dr. Kelley continues, “However, it is generally felt that two or more fasting glucose tests which fall above 100 and below 126 on two different days, would be reasonable to assess as prediabetes.”
Research in the field of how sleep impacts glucose metabolism is relatively young, but the research results are solid, including the report in a 2010 Journal of Clinical Endocrinology & Metabolism that just one night of sleep deprivation can cause insulin resistance, a type of prediabetes that’s a forerunner of type II diabetes.
If your fasting glucose is over 100 and under 126, don’t panic. Evaluate your sleeping habits.

Has your sleep been disrupted lately due to anxiety?
Chronic stress can also cause a higher than normal fasting glucose result.
Ongoing stress/anxiety causes blood sugar to rise, to be available as a quick energy source for muscles —the body interprets stress as a sign of an imminent fight or flight.
The fight or flight response uses up the sugar and restores normal chemical balance.
In our modern world, people don’t fight or flee; they sit and seethe.
The blood sugar (glucose) remains elevated, always on standby for a fight or flight that never occurs.

Regular gym workouts may not be enough to lower blood sugar below 100 in some of these cases.
“By the same measure, two different fasting glucose tests that are done on different days, and found to be 126 or higher, and especially if one is symptomatic (increased thirst and urination, weight loss, easy fatigue) is generally enough to assess a diagnosis of diabetes,” adds Dr. Kelley.
“Symptoms of diabetes tend to be more prominent the higher and longer blood glucose levels remain outside of the norms for a healthy blood glucose range.”


























 Richard Kelley, MD,
Richard Kelley, MD,