Actinic Keratosis Prevention with Retin A ?

Actinic keratosis is a so-called precancerous lesion caused by sun damage.
Can these lesions be prevented with application of retin A?
Retin A is also known as retinoic acid.
To find out if retin A could have a preventive effect against actinic keratosis, I consulted with dermatologist Richard Bezozo, MD, President of MoleSafe, the world’s most advanced melanoma screening program.
Dr. Bezozo’s answer is: “No.”
Just what is actinic keratosis?
“AK is also known as solar keratosis,” says Dr. Bezozo.
“They are scaly crusty growths that develop slowly.
“Typically an eighth to one-fourth inch in size and caused by sun damage, AK indicates a risk for skin cancer.”
Actinic keratoses are extremely common in people over 40.

Actinic keratosis on the ear. Future FamDoc, CreativeCommons
Just what does “precancerous” mean for this condition?
Dr. Bezozo says, “Ten percent will advance to squamous cell cancer.”
However, you need to keep this information in the proper context:
The advancement occurs in 10 percent of untreated cases; and many times, a person fails to seek treatment — giving the lesion ample time to get worse.
Sometimes, the patient is unaware of the presence of a developing lesion (it may be, for instance, on their scalp).
Squamous cell carcinoma kills about 3,500 Americans a year and grows slowly, and many people just don’t realize something sinister has been slowly growing on their face, neck and other sun-exposed areas for a long time, and may shrug the lesions off as benign signs of aging skin.
Preventing Actinic Keratosis
Dr. Bezozo says: “Prevention techniques include using a broad spectrum UVA/UVB sun protection. By the time you get them the damage has been done. Retin A is typically used to treat acne.”
Though most patients are over 40, younger people are not immune to actinic keratoses.
Application of retin A may help manage other conditions, but this is not one of them.

Richard Bezozo, MD
There are more new cases yearly of skin cancer than breast, prostate, lung and colon cancers combined. The MoleSafe system produces high-resolution diagnostic images and creates a profile for your skin that’s monitored for any changes in moles.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dermatology11
Melanoma Risk in Blondes Who Tan vs. Always Burn

Does melanoma risk differ in blondes who always tan and blondes who always burn?
If you’ve heard that blonde hair is a risk factor for melanoma, perhaps you’ve wondered about olive skinned people who have naturally blonde hair, or natural blondes who simply tan easily but don’t have olive skin.
“We do not segregate blondes who never tan as a particularly vulnerable group,” says Richard Bezozo, MD, President of MoleSafe, the world’s most advanced melanoma screening program.
“We discuss melanoma risk regarding fair skin individuals (people with freckles, light blonde or red hair and blue eyes as well). All of these people fall under the category of a Fitzpatrick 1.”
Dr. Bezozo explains, “Thomas Fitzpatrick was a Harvard dermatologist who came up with a scale in regards to individual’s skin types in 1975.
“It is a useful tool for identifying people at risk for various skin diseases, for example, how likely you are to get skin cancer.
“The scale can also be used by dermatologists to recommend facial treatments.”
Dr. Bezozo describes this system as follows:
Fitzpatrick 1- a person with light skin, light hair, blue eyes and who burns easily and often.
Fitzpatrick 3 – a person with cream white skin, fair with any eye or hair color who sometimes burns and gradually tans.
Fitzpatrick 6 – a person who is dark skinned and never or rarely burns.

Melanesian children. Their hair color is natural, due to a gene mutation in their population.
He adds, “The lighter the skin the more the damage from the sun’s rays. Since skin damage is cumulative, blondes who always burn (Fitzpatrick 1s) have a higher risk for melanoma.”
Dr. Bezozo says the following individuals should get early melanoma detection screening:

“Blondes who never tan and always burn, people who have had more than one blistering sunburn in their lifetime, people who have more than 10 moles, people with a family history of skin cancer, people who have previously had skin cancer or people with a weakened immune system.
“Light skinned people should also avoid excessive UV exposure (tanning beds).”

Richard Bezozo, MD
There are more new cases yearly of skin cancer than breast, prostate, lung and colon cancers combined. The MoleSafe system produces high-resolution diagnostic images and creates a profile for your skin that’s monitored for any changes in moles.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Stage 1 Melanoma Look Like a Normal Mole?
Learn more about stage 1 melanoma and its appearance.
It’s a smart question: Can stage 1 melanoma look like a normal (benign) mole?
“A stage 1 melanoma can look like a normal or featureless mole even to a trained naked eye,” says Richard Bezozo, MD, President of MoleSafe, the world’s most advanced melanoma screening program.
“The changes that occur with a melanoma may not be visible for some time.
“Stage 1 melanoma is when melanoma is in the outer layers of the skin and has not spread to lymph nodes.
“Stage 1 varies, but for melanomas that are less than 1 mm in depth the risk of metastasis is almost zero.”
Just because a stage 1 melanoma may look normal to the naked eye, doesn’t mean that it looks the same as it did a month ago.
This is why it is so vital to get to know your moles and other “spots” (and this includes where they’re not), so that you can tell if one’s been changing in appearance, or if a spot or “freckle” is brand new.
Sometimes a very tiny scab can pass for a “new” mole if its location prevents an up-close visual inspection by the patient.
It’s important to realize that a new spot or lesion isn’t necessarily a mole or malignant.
Dr. Bezozo says, “Dermoscopy as used in the MoleSafe program can identify melanomas in stage 1. Dermoscopy can reveal subtle changes to your skin that’s not visible to the naked eye.”
How does this skin cancer detection technology work?
“MoleSafe incorporates the total body photography, digital dermoscopy, serial monitoring and risk assessment procedures to diagnose melanoma at the earliest possible stage,” explains Dr. Bezozo.
“Using the system, a patient’s images can be evaluated by the dermoscopist (a dermatologist who specializes in reading dermoscopic images) quickly and effectively, often reducing the number of unnecessary biopsies.”

Richard Bezozo, MD
There are more new cases yearly of skin cancer than breast, prostate, lung and colon cancers combined. The MoleSafe system produces high-resolution diagnostic images and creates a profile for your skin that’s monitored for any changes in moles.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
How Common Is a Blue Melanoma?

Maybe you’ve heard that melanoma can be blue, but how often is this?
What is the answer to how common or often is a melanoma blue?
“Not common. They are rare, aggressive and often lethal,” says Richard Bezozo, MD, President of MoleSafe, the world’s most advanced melanoma screening program.
Dr. Bezozo adds, “They are also known as malignant blue nevus.”
A nevus (pronounced knee-vus) is the medical term for mole.
“These are melanomas arising in association with a blue nevus or those arising spontaneously in the skin which resemble a blue nevus,” he continues.
“If you see something new or changing on your skin, have it checked out by your dermatologist. Blue nevi tend to be large, 1-3 cm in diameter and they can be elevated or smooth.
“Typically they are greyish-blue to blueish-black. They are often solitary and can be found on your buttocks, your lower back, or your hands and feet. Still, they are very uncommon.”
A blue appearing mole isn’t necessarily a melanoma. In a benign mole of this color, the pigment cells are deeper in the skin.
“Often solitary” does not mean, however, that blue melanomas can never be clustered, as in the metastatic melanomas below.

Keep in mind that a condition such as this does not develop overnight.
- You should check the skin on your entire body on a monthly basis for anything that looks suspicious, including a new blue color to a previously brown mole.
- Get to know your moles so that if changes begin happening, you will be aware of this.
The patient pictured above obviously either failed to regularly examine their skin and thus was unaware of the changes in their skin early on, or, was aware of the ongoing development of all the blue lesions but failed to seek medical intervention.
Melanoma as it progresses eventually becomes visually alarming.

Richard Bezozo, MD
There are more new cases yearly of skin cancer than breast, prostate, lung and colon cancers combined. The MoleSafe system produces high-resolution diagnostic images and creates a profile for your skin that’s monitored for any changes in moles.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
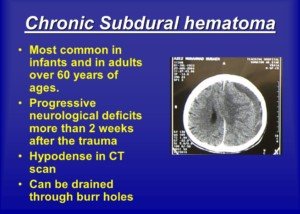
Prediction of Chronic Subdural Hematoma: Symptoms After Fall?
Find out if neurological symptoms at time of head trauma that soon vanish are predictive of chronic subdural hematoma even with normal CT.
Is a person more likely to develop a chronic subdural hematoma if, at the time of getting hit in the head, they have neurological symptoms, even if the symptoms dissipate soon after?
“Some patients strike their head and do not remember the fall, so it is hard to obtain a history in those patients,” begins John M. Abrahams, MD, chief of neurosurgery at Northern Westchester Hospital, and founder of the Westchester Neuroscience Research Foundation which is studying the genomic profile of malignant brain tumors.
“The stronger the ‘hit,’ the greater the chance of developing a chronic subdural hematoma,” he continues.
“Another predisposing factor is the use of blood thinners.
“Some patients are on these medications for other medical conditions and each has an increased risk for brain bleeding with general use.
“The symptoms can be helpful in terms of predictive value, but not every mild-to-moderate concussion patient does not develop a hemorrhage.”
 Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ michaelheim
Elderly on Coumadin, Hits Head: Subdural Hematoma Risk?

Learn more about the odds of an elderly patient on Coumadin developing chronic subdural hematoma after hitting their head.
It’s not a pretty trio:
1) Coumadin therapy
2) Getting hit in the head
3) Elderly age. After all, this is a significant threesome in terms of risk of chronic subdural hematoma.
Suppose you have an elderly relative who’s on Coumadin (an anticoagulant), and this individual falls and hits their head.
A CT scan soon after would be a smart idea, even if the patient is lucid.
Most elderly people in this situation will not develop a chronic subdural hematoma, but the number who will carries statistical significance.
“Anticoagulation to conventional intensities increases the risk of intracranial hemorrhage 7- to 10-fold, to an absolute rate of nearly 1%/year for many patients,” says John M. Abrahams, MD, chief of neurosurgery at Northern Westchester Hospital, and founder of the Westchester Neuroscience Research Foundation which is studying the genomic profile of malignant brain tumors.
“Most (70%) anticoagulant-related intracranial hemorrhages are intracerebral hematomas (approximately 60% are fatal),” says Dr. Abrahams. This is bleeding inside the brain.
“The bulk of the remainder are subdural hematomas,” says Dr. Abrahams.
The bleeding of a subdural hematoma, including chronic, occurs between the brain and the tissue that’s one layer above it, called the dura (“sub” means beneath). The tissue between the brain and dura is called arachnoid.
“Predictors of anticoagulant-related intracerebral hematoma are advanced patient age, prior ischemic stroke, hypertension and intensity of anticoagulation,” he continues.
“In approximately half of anticoagulated elderly] patients with intracerebral hematoma, the bleeding evolves slowly over 12 to 24 hours, and emergency reversal of anticoagulation is crucial.”
If the elderly patient has symptoms immediately following the head trauma, is this predictive of a chronic subdural hematoma?
“If the patient has symptoms right after the fall, then they have a greater than a 50% chance of developing a real intracranial hemorrhage of some sort,” says Dr. Abrahams.
What if the symptoms go away fairly quickly?
“If the symptoms dissipate in an hour, then they are probably fine.”
Even two hours means they’ll likely not develop complications down the road.
Is location of the “bump” on the head predictive of a cSDH?
“Location can indicate where the headache may arise, but only in some patients, and is not a clear indicator.”
 Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photographee.eu
Percent of People with Normal Head CT Who Develop Brain Bleed

A neurosurgeon answers the question of what percent of people with a normal CT scan after hitting their head develop a chronic subdural hematoma.
Out of all the people who have a normal CT scan of their brain after experiencing a hit to their head or a fall, a certain percentage will go on to develop a chronic subdural hematoma.
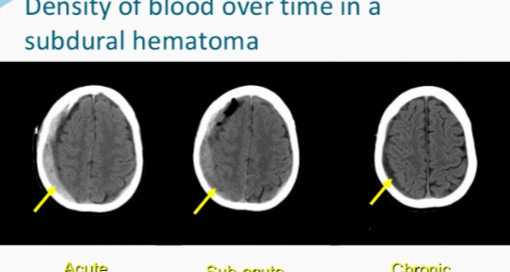
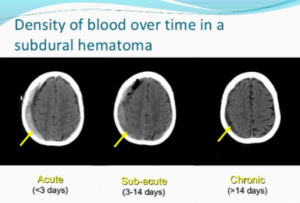
A subdural hematoma of the chronic type means that the bleeding is occurring at a slow rate over time.
The symptoms begin anywhere from three weeks to three months out from the initial head trauma.
The blood leaks from tears in the tiny veins underneath the dura mater of the brain.
How many with a chronic subdural hematoma initially had a normal head CT?
“The number of people who strike their heads is difficult to quantify,” says John M. Abrahams, MD, chief of neurosurgery at Northern Westchester Hospital, and founder of the Westchester Neuroscience Research Foundation which is studying the genomic profile of malignant brain tumors.
“Overall, most patients who develop chronic subdural hematoma did not have an incidental CT scan at the time of the fall.
“In general, the number of patients who fall and develop chronic subdural hematoma is quite small, probably on the order of less than 1%.”
This percent figure will differ if specific age brackets are explored.
For instance, more people over age 70 with an initial normal head CT will go on to be diagnosed with a chronic subdural hematoma, when compared to those age 40 to 50.
Being over the age of 65 is a risk factor for one of these brain bleeds.
That’s because of age-related brain atrophy (shrinkage), which stretches the bridging veins, making them more prone to tearing.
Even minor head trauma can lead to bleeding in this population.
Additionally, older adults are more likely to use anticoagulant or antiplatelet medications (blood thinners), which impair blood clotting and increase the likelihood and severity of bleeding within the subdural space.
Some cases of cSDH in the elderly have no known associated head trauma or fall, and may arise simply from a combination of age-related brain shrinkage and anticoagulation therapy (like a daily aspirin or Coumadin).
 Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/uzhursky
Time of Day Chronic Subdural Hematoma Symptoms Usually Start?
Is there a time of day that symptoms of chronic subdural hematoma typically begin?
You may be wondering if there’s a particular time of day that a person, who’s destined to develop a chronic subdural hematoma, will begin experiencing the neurological symptoms caused by this condition.
A subdural hematoma literally means collection of blood beneath the dura mater of the brain.
In the acute type, the hemorrhaging occurs soon after the blow to the head and is life threatening.
In the chronic type, symptoms from the bleeding (e.g., headache, nausea, change in mental status, weakness) begin occurring three weeks to 90 days out.
Do symptoms of a chronic subdural hematoma usually arise in the morning soon after the patient awakens? Or can they strike at any time?
“The symptoms usually do not depend on sleep-wake cycle,” says John M. Abrahams, MD, chief of neurosurgery at Northern Westchester Hospital, and founder of the Westchester Neuroscience Research Foundation which is studying the genomic profile of malignant brain tumors.
“Rather, they depend on severity and can affect someone all day.
“If the patient has difficulty walking or standing, symptoms would be worse upright rather than lying or sitting.
“If the patient has a headache, it can be better when lying flat rather than standing upright.”
If the patient has pre-existing medical conditions, it can be difficult to determine when the onset of the cSDH symptoms begin.
For example, the patient may already have some level of mobility impairment from a past accident or stroke.
The mobility symptoms of a cSDH can mimic that of a stroke.
They may also be in the midst of recovering from, say, knee replacement surgery, and are already physically compromised.
Nevertheless, symptoms of chronic subdural hematoma can begin kicking in at any time during the day, night or middle of the night.
Chronic subdural hematoma generally has a favorable prognosis, especially with surgical treatment.
Studies report survival rates ranging from 80% to 95% post-surgery, depending on patient age, comorbidities and neurological status at presentation.
Note: Survival doesn’t equate to permanent neurological damage following treatment.
Permanent neurological damage after treatment can result from prolonged brain compression before intervention, leading to irreversible injury.
Additional factors include delayed treatment, recurrent bleeding, brain atrophy in elderly patients, or complications such as seizures, infections or stroke.
Damage may also stem from preexisting conditions or impaired cerebral blood flow during the hematoma’s development, all of which can hinder full neurological recovery.
A recurrence of a cSDH occurs in about 10-20% of cases.
 Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
Dr. Abrahams is a highly regarded, board certified neurosurgeon who specializes in the treatment of complex disorders of the brain and spine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Collagen Injections Cause Misshapen Lips?

Ever wonder if those horrid lip jobs are the result of botched collagen injections?
You’ve probably seen photos of women with grossly enlarged lips that go beyond the infamous “trout pout.”
Can collagen injections ruin a woman’s lips to this extent?
Certainly, many women want a fuller, sexier pout and have been considering collagen injections.
“Misshapen lips that cannot be improved usually happen from procedures where permanent fillers/implants were utilized,” says Allen Gabriel, MD, board certified plastic surgeon with PeaceHealth Medical Group Plastic Surgery in Vancouver, WA.
Collagen injections last three to nine months, and are certainly a practical alternative to something that’s more permanent and has more potential to cause a misshapen appearance.
If lips have become misshapen from a permanent filler or implant, Dr. Gabriel says, “This is when additional surgical procedures are needed to remove the product and can further misshapen the lip.”
This is probably what has happened in most of those hideous photos of “botched jobs” you’ve seen.
Is there an alternative to collagen injections?

Shutterstock/Olena Chukhil
“The nice thing about getting injected with hyaluronic acid products is that this can be immediately reversed if one is not happy with the results.
“There is a solution that can be injected and will immediately dissolve it, and after the swelling goes down, one is back to the original lip shape and size.”
In addition, fat transfer for lip augmentation involves harvesting fat from one part of the patient’s body, processing it and then injecting it into the lips.
This procedure enhances lip volume and contour using your own fat, offering a natural alternative to synthetic fillers.
Results can be long-lasting but may require multiple sessions.
 Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Best & Safest Way to Plump Lips Medically & Look Great

A plastic surgeon explains what works best to medically make lips plumper and fuller.
There’s more than one way to make lips plumper and fuller medically, but is one particular way the best?
Let’s face it: Plump, full lips are a draw. Name one female movie star who didn’t have a good set of lips.
Okay, there might be a very tiny few. But let’s see how easily you can come up with the names of those few.
In the ’70s and ’80s, quite a few TV stars did not have plump lips, such as Farrah Fawcett, Kate Jackson and Cheryl Ladd. By today’s standards, they had thin lips.
But these days, or perhaps beginning in the early ’90s, a trend began kicking in: Want to make it big on TV? You’d better have a killer pout.
Women who star in TV shows that involve a lot of close-up shots while they speak almost always have very well-endowed lips (Jennifer Garner in “Alias,” anyone? How about Leah Remini in “King of Queens”? And let’s not leave out Jeri Ryan in “Star Trek: Voyager”).
Best Way to Get Plumper Lips Medically

Shutterstock/ Sergey Golenko
“Medically ‘plumping’ up lips includes creating a fuller and plumper lip (upper and lower) and reducing fine lines around the mouth,” says Dr. Gabriel.
“Injections of collagen or hyaluronic acid can achieve this with varying lasting results” — three months for collagen and nine months for hyaluronic.
“Additional procedures with implantable products and fat injections can also be done, and these are longer lasting to permanent, but not necessarily the best options as it can lead to unnatural feel of the lip.”
If you want to medically plump your lips, consider the temporary method first.
“When fillers are used for lip plumping one can assess its results and decide if this is something they would like to pursue since the results are temporary,” says Dr. Gabriel.
“If happy with results, discussion of longer lasting procedures should take place with your board certified plastic surgeon or dermatologist.”
 Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.