Can a Mole Turn into Squamous Cell Carcinoma?

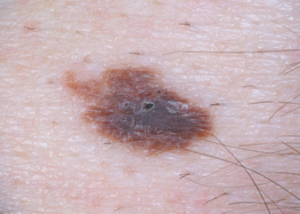
Normal mole under magnification
Can a normal mole ever turn into squamous cell carcinoma, which kills about 3,500 Americans every year and is considered the second-deadliest of all skin cancers?
It’s a good question: Is it ever possible for a squamous cell carcinoma to arise from a pre-existing typical mole.
“No, we do not usually see squamous cell carcinoma arising from a mole,” says Dr. Susan Weinkle, a board certified dermatologist with a private practice in Bradenton, FL.
Thus, as you may already know, the deadliest skin cancer, melanoma, comes from moles in about 25 percent of melanoma cases, but moles cannot turn into squamous cell carcinoma.
What does squamous cell carcinoma look like?

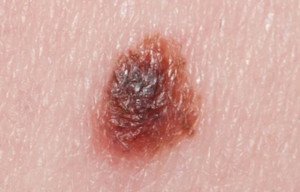
Squamous cell carcinoma. Shutterstock/Dermatology11
Dr. Weinkle explains: SCC usually appears as growing lumps, often with a rough, scaly, or crusted surface.
They may also look like flat reddish patches in the skin that grow slowly. They commonly occur on sun-exposed areas of the body such as the face, ear, neck, lip, and back of the hands.
Sometimes, they form in the skin of the genital area and they can also develop in scars or skin ulcers elsewhere.”
A precancerous skin condition called actinic keratosis can have the appearance of early squamous cell carcinoma.
Some dermatologists actually consider actinic keratoses and SCC to be on the same continuum, or, to put it another way, actinic keratosis is squamous cell carcinoma in its earliest form.
However, this is not the general consensus among dermatologists. If left untreated, most actinic keratoses will not morph into squamous cell carcinoma.
And when they do, it takes years for this to happen. If you’ve been diagnosed with actinic keratosis, don’t panic; don’t get alarmed.
Actinic keratoses are curable, and only rarely (5-10 percent) become squamous cell carcinoma, and that’s when they are left untreated.
And out of those that become squamous cell carcinoma, only 10 percent actually spread to other parts of the body – and those are the ones that are not caught early enough to be cured.
Most squamous cell carcinomas are slow-growing, and when they spread, it’s because the patient either:
1) became aware of it but brushed it off as a sign of aging or nothing to worry about, or 2) the tumor developed in a location that the patient didn’t readily see, such as behind an ear or on top of the head.
It’s important to check your moles every month, as well as non-mole areas of skin, for any suspicious spots or new lesions, including squamous cell carcinoma, and have a dermatologist check your skin annually.
 A skilled surgeon with 30+ years’ experience, Dr. Weinkle is also a Fellow in the American College of Mohs Surgery. She is past President of the American Society for Dermatologic Surgery.
A skilled surgeon with 30+ years’ experience, Dr. Weinkle is also a Fellow in the American College of Mohs Surgery. She is past President of the American Society for Dermatologic Surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Will Having Normal Moles Removed Prevent Melanoma?

Melanoma can arise from a pre-existing mole, so you might be thinking that it’s smart to have your normal moles removed to at least prevent the development of melanoma from these moles.
If you have many moles, the idea of having them electively removed will be even more appealing, since having many of these skin lesions is one of the risk factors for melanoma.
Having moles electively removed, out of melanoma fear, can also be referred to as “de-moling.”
However, “The principal always followed in medical care is according to Hippocrates’ oath, ‘First do no harm,’” says Maria M. Tsoukas, MD, PhD, Assistant Professor, Dermatology Section, University of Chicago.
In medicine and specifically in dermatology, we keep a very low threshold in clinical examination and in deciding which nevi need to be biopsied or removed.”
A nevus is the Latin term for mole, and nevi is the plural form. “Pending on each individual case history and clinical exam as well as family history of melanoma, we decide which moles need to be removed,” says Dr. Tsoukas.
“We are focused on clinically appearing atypical nevi that under microscopic examination may have some abnormal features; however, do not meet all criteria to be identified as malignant melanoma.”
A patient may be concerned about one or two particular moles, perhaps due to size (they’re bigger than all the others on the patient’s body), or maybe they stand out because they’re darker than the rest.
For peace of mind, the patient then decides to have the moles electively removed. After all, the mindset might be, I know I can’t prevent melanoma from arising anywhere in my body, but at least I can prevent it from developing in these two particular moles.
Insurance won’t cover the cost of this if the only reason is peace of mind or anxiety.
Reimbursement logistics aside, Dr. Tsoukas says that in medicine, management and intervention are justified based on certain criteria and facts.
Otherwise, somebody would have medical care or intervention randomly decided.
Another reason that a person may have a mole electively removed is because of its location; it’s difficult for the individual to examine the mole as part of routine monthly skin exams.
But what if you have a lot of moles peppered all over your body?
It’s not practical to have every one of these spots systematically cut out or even “shaved” off.
On the other hand, what if many of these moles are on your back, which compounds the difficulty in keeping track of them for possible changes?
How do you draw a “mole map” of the spots on your back, unless you have an elaborate set-up with mirrors that frees up your hands (for sketching) and provides a clear view?
What if your ability to draw spots in a “map,” that accurately aligns with what you see in the mirror, is in sad shape?
And add to that this: Elective removal of many moles will cost a pretty penny and create a lot of hassle due to bandaging and removal of stitches.
If you have many skin lesions, including normal looking ones, it’s wise to get a yearly full-body skin exam.
A dermatologist will address moles that are clinically benign, those that show atypical features, and those that should be removed and biopsied.
“In addition,” says Dr. Tsoukas, “dermatologists use the mole mapping technique which combines photography, dermoscopy and a body map file created and saved electronically for each patient.”
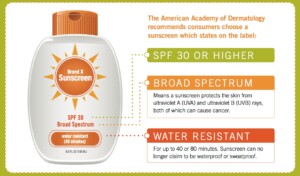
In addition to the skin exam, your dermatologist will explain additional risk factors for melanoma, which include skin type, family history of melanoma, sunburn history, age and even history of medications you’ve taken. You will also learn about sunscreen protection.
Dr. Tsoukas’ clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.
clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Suspicious Mole? Get Biopsy; Don’t Rely on Handheld Lenses

Only a biopsy has the final word on whether or not a worrisome mole contains melanoma cells or is entirely a melanoma.
That suspicious mole should be biopsied, even if your dermatologist says it “probably isn’t” melanoma after viewing it through a handheld lens known as a dermoscope or dermatoscope.
Though statistically, chances are in your favor that the questionable mole is benign, you should still get a biopsy.
“Whether you feel uneasy or your doctor is recommending a biopsy for a suspicious spot, it’s important to get the spot checked,” says Dr. Gretchen Frieling, MD, Triple Board Certified Boston Area Dermatopathologist.
“When you feel nervous about a spot, you can consult your skin specialist who will assess the spot and recommend a biopsy,” continues Dr. Frieling.
“If the doctor feels the spot may be something else, they can advise you accordingly. But when it comes to melanoma, the benefit of getting tested and finding the condition in time outweighs any risk of being overly cautious.”
Though melanoma has gotten a lot of media attention over the years, and coverage seems to be increasing, it’s still rare for moles to transform to melanoma.
However, about two-thirds of melanoma tumors arise in areas of skin where there was no pre-existing mole.
At Frontiers in Optics 2010 (Oct. 24-28), Duke University scientists presented a new technique for aiding dermatologists in helping to differentiate normal moles from melanomas, by using high-resolution snapshots of moles that appear suspicious.
About 25 percent of dermatologists use a dermatosope for routine checks of a patient’s moles.

Dermatoscope. Shutterstock/LightField Studios
Certainly, you can imagine how long it would take for a routine skin inspection if the doctor used the dermatoscope to inspect every one of a patient’s 150 moles. Some people have even more moles.
On the other hand, some doctors don’t use this tool even for patients with a small number of moles.
It’s perfectly okay for the patient to request that the practicioner use this special magnifying device.
But this special lens is not a diagnostic tool. Though it enables the doctor to see things that he can’t with the naked eye, it’s still no match for a biopsy.
My doctor took me by surprise during one of my annual skin exams by saying, “You have a mole on your upper arm that gets my attention, and I’d like to get a biopsy on it.”
This was after she examined it with the dermatoscope. (The biopsy was done – entire mole removed).
She said a few times that it was “probably benign,” but you’ll want your doctor to always be ahead of the wave. My mole turned out to be benign.
In short, a mole that gets even only the attention of the patient should be biopsied. Trust your gut.
Cancerous changes can take place too deep within the mole to be seen with the handheld lens, though there are cases in which the physician not only can clearly see cancerous signs with the instrument, but with the naked eye as well.
However, there are times when even a biopsy nets disagreement among doctors.
So what about that study?
The Duke researchers proposed a two-photon microscopy technique that infuses a small quantity of energy into the two kinds of pigments that are found in skin: pheomelanin, and eumelanin.
The energy redistributes to yield high-resolution images of the pigments’ distributions, indicating possible melanoma or not.
“No one has been able to look at where different melanins are organized in skin,” says the lead researcher in the report. “This opens up a whole new pathway of looking for melanoma.”
At any rate, whenever you have a mole removed, even just for cosmetic purposes, insist upon a biopsy, just to play safe; a normal looking mole may end up being melanoma after all.
 Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
Dr. Frieling’s website is gfacemd.com. In addition to 15+ years of experience in dermatology and dermapathology, Dr. Frieling provides advanced micro-enhancement techniques to optimize the health and beauty of her patients’ skin.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Albina Glisic
Source: sciencedaily.com/releases/2010/10/101020194811.htm
Mole Removal with Laser Causes Regrowth of Moles

If you want a mole removed with a laser, the mole might grow back.
Traditionally, the idea is that a laser beam will penetrate the mole’s surface area to disintegrate any abnormal cells, and the expectation is that any remaining cells will be absorbed by the body.
But there’s a problem: Laser light can rejuvenate skin cells, and this includes mole cells.
In fact, not only can laser treatment cause moles to grow back, but it can also cause a regrowth of other skin deviations that a person believes will be removed with laser treatment.
“The latest research conducted on the effectiveness of lasers, and its use for mole removal, revealed laser treatments stimulated growth of moles, warts, and skin tags, causing many to reappear after removal,” says Dr. Geoffrey Rappert, a member of the American Board of Dermatology, speaking in a hospital interview, as presented in a news release.
This doesn’t mean that every single laser mole removal treatment results in the spot growing back.
It means that sometimes the mole grows back. “This has to do with the way laser light gently donates energy or waves of photos causing rejuvenation of the cell,” says Dr. Rappert.
Another Reason a Mole Grows Back After Laser Treatment to Remove It
“The only way to [completely] remove a mole is surgically,” says Adarsh Vijay Mudgil, MD, double board certified in dermatology and dermatopathology, and founder of Mudgil Dermatology in NY.
“Lasers can reduce/eliminate pigmentation (they target melanin, not the melanocyte itself).”
A melanocyte is a specialized cell in the skin that produces the pigment in a mole. The pigment is called melanin.
“Moles that are treated with laser have a very high rate of recurrence, because if the melanocyte itself remains viable, it can resume the production of melanin,” says Dr. Mudgil.
Why then, settle for laser treatment?
Even if your desire to have a pigment spot removed is purely cosmetic, or for convenience (e.g., the mole keeps getting rubbed by clothing), you may as well rely upon more effective, sure ways of treatment: freezing or excision by a dermatologist.
And, if you’re going to have a mole removed, it’s always smart to have it biopsied, even if it looks normal.
I once read about a very young woman who, for cosmetic purposes, had a large mole on her shoulder removed.
Apparently, the doctor removed only the superficial portion, leaving behind portions of the growth beneath the skin.
Because this was a cosmetic procedure, the patient was satisfied because the pigmented area was no longer visible. But this didn’t mean the melanocytes were no longer there.
They were. And what remained there in the young woman eventually morphed into melanoma skin cancer.

Melanoma. Laurence Meyer, MD. cancer.gov
At the initial visit just to have the spot removed, the doctor threw away the portion he had removed, instead of sending it out for a routine biopsy.
He didn’t use laser removal for the mole; he cut it out, but didn’t go deep enough.
At Kaiser Permanente, if you go in to have a mole removed purely for cosmetic purposes, they will automatically send it to the pathology lab for a biopsy, even if it looks normal.
Yes, this will create an additional out-of-pocket expense to patients, but it can be life-saving.
The woman who had the shoulder mole removed eventually died from her melanoma.
It has been speculated that had her doctor sent the removed portion to be biopsied, that the early stages of melanoma could have been detected.
 Dr. Mudgiltreats infant to geriatric patients, and is versed in all aspects of medical, surgical and cosmetic dermatology. He has published extensively in the medical literature plus has lectured at numerous national meetings.
Dr. Mudgiltreats infant to geriatric patients, and is versed in all aspects of medical, surgical and cosmetic dermatology. He has published extensively in the medical literature plus has lectured at numerous national meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock, Ekaterina Vidyasova
Source: prweb.com/releases/mole-removal/treatment-options/prweb868604.htm
Mole Mapping at Home: Melanoma Screening Techniques
Learn how to produce a very reliable mole map at home for melanoma screening.
I have been “mole mapping” for three years and have learned along the way some excellent mapping techniques, for melanoma screening.
The technique I will describe has one caveat; you must be able to illustrate.
If a mole is on a part of your body that allows you to visually inspect it while your dominant hand draws it, this is a great mapping technique.
I was once watching a mole on my upper inner thigh, and decided to draw it. I held a magnifying glass over it, and with my dominant hand, drew and rendered what I saw.
In order for illustrative mapping to be reliable, you must be able to capture the mole’s nuances, subtle tone variations and other details – and draw them to an enlarged scale.
I drew the mole a lot bigger than its actual size (which was about 2 millimeters).
I drew another one that was on my lower abdominal region (it actually turned out to be a seborrheic keratosis, which can look very much like a mole; it had changed in appearance so I drew it).
The drawing should be a rendering, not merely a line drawing.
This way you can monitor for changes in color tone variation. Another reason to render is because often, the tone variation is gradual or gradated, rather than with a definitive demarcation.
With an illustration at hand, every time you check the mole, you don’t have to wonder if you’re imagining that a certain part of it is darker; or if the darker part of it has spread to fill up more of the mole; or if a darker or lighter part of it has changed shape or spread to take up more of the mole.
Because all you need to do is refer to the illustration, and you can see exactly how the spot appeared last time you checked it, and match the drawing up to what you’re now seeing.
Another way to illustratively do mole mapping is to imprint in your mind what the particular spot looks like.
This is applicable for moles that are located in areas that make it impossible to draw them.
I had one on the back of my neck that I thought was changing, so I imprinted it in my mind: border shape; the shape of the darker portion of it; any gradations.
With a ballpoint pen I drew it enlarged to scale and rendered it. I then monitored it based on this illustration. Soon after, a dermatologist said it was a seborrheic keratosis (these can change).
Being an illustrator also means you can measure whether or not a tiny mole is getting bigger. A “birth mark” on my shin had taken on a reddish tinge, but it was not bigger.
In anticipation that it might be getting bigger (since it was changing colors), I drew this little spot with a pencil to its exact size, on the edge of an index card.
I then could place the stiff edge of the card perpendicular to my shin, against my shin, just a tiny bit away from the mole, which then enabled me to make an accurate visual size comparison.
To add even more accuracy, I drew a spot next to the first drawing that was a little smaller, and one on the other side that was a little bigger.
I’d compare the mole to the middle drawing and it was a spot-on duplication of the size and shape (1 millimeter). After a few days, I noticed that the mole was a hair bigger than the original drawing!
I then lined the mole up with the larger rendition, and they matched in size! This was objective proof that the mole had increased in size!
So, not only had this previously solid brown spot taken on a reddish tinge, it had increased in size.
I had it removed and biopsied. Diagnosis: lentigo simplex (translation: irritated sun spot). The dermatologist’s nurse told me that it had probably been inadvertently rubbed or scratched, even maybe in my sleep.
What a Doctor Says About Moles
“A mole which is reactive to scratching or irritation, and does not have the cardinal signs of melanoma is still considered a benign lesion,” says Dr. Joshua Fox (not my dermatologist), founder and director of New York and New Jersey-based Advanced Dermatology P.C.
“It is benign and not dangerous in any way, even if it were to have some characteristics of the appearance of melanoma.
“It may require symptomatic treatment and observation; however, it will not be treated as melanoma.”
Mole mapping should include, when possible, drawings of your moles, for optimizing melanoma screening.

In 1987 Dr. Fox founded the AAD Melanoma and Skin Cancer Prevention Program in Queens, NY. He has been chief of dermatology of several major teaching hospitals including Mt. Sinai Hospital of Queens.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Small, Tiny Moles Turn Into Melanoma?

Can melanoma come from small, tiny moles?
Do you believe a mole can never turn into melanoma as long as it’s small or tiny?
If, during your monthly skin exams for cancer, you’ve decided to skip past your small, tiny little “birth marks” – you’re making a big mistake.
Historically, the rules for self-screening for melanoma have been to pay attention to the ABCDs of mole inspection, in which the “D” stands for diameter.
And typically, the diameter to be suspicious of is anything larger than 4 millimeters, or “the size of a pencil eraser.”
That got me thinking, because what’s so magical about 4 or 5 millimeters such that any mole smaller would be resistant to turning into melanoma?
“When I was training in dermatology in the mid-1970s, the ‘rule’ was that if a mole was less than 4 mm in diameter (one-sixth of an inch), then it couldn’t be a melanoma already,” says Neal Schultz, MD, a dermatologist with a private practice in the NYC area, and founder of dermTV.com.
“We now know that moles as tiny as 1 mm (1/25th of an inch) can already be a melanoma.”
I saw two red melanomas on a 27-year-old man’s forearm that were about 1 millimeter or so.
However, they had not sprung from pre-existing spots or “birth marks.”
Can a pre-existing, normal mole, that is small … say, around 1 millimeter … ever transform into melanoma?
Dr. Schultz continues, “People often wonder whether melanoma arises from normal pre-existing moles, or whether they arise ‘de-novo,’ meaning just from a single melanocyte (pigment cell) in the skin, which then becomes cancerous and goes crazy.”
Between 2003 and 2007, 150 melanomas that Dr. Schultz had diagnosed were analyzed in the laboratory for a retrospective study.
It turned out that 23 percent of the cancers were shown to have originated within a precancerous spot – and this included 1 millimeter moles.
“But then you have to understand that when a melanoma is really advanced and far developed, even if it develops in an abnormal mole, it may have destroyed the original mole.
“So the 23 percent number is a minimum, but not a maximum, since some of the melanomas that I diagnosed may in fact have arisen in moles, which the melanoma completely destroyed, and therefore there is no way on knowing that in fact, it started in a mole.”
Pay close attention to your small birth marks, brown spots, freckles, sun spots, what-have-you.

Just because a pigmented lesion is very small doesn’t mean that the DNA in it is resistant to the mutational changes that lead to melanoma.
If a tiny little “birth mark” seems to be getting bigger or darker, have a dermatologist look at it.
Interestingly, whether or not small moles can ever turn into melanoma has not received any fine-tuned verdict by the medical community.
Dr. Schultz says that some physicians believe “melanomas never arise in preexisting benign moles, and other physicians such as myself believing that as many as 20-25 percent of melanomas arise in preexisting benign moles, which in my view is substantiated by studies such as the one I mentioned.”
Many patients have reported that they’d been aware of a mole for years, appearing stable, and then one day they noticed that the spot was changing – with the diagnosis ultimately being melanoma.

Melanoma under magnification. Shutterstock/Nasekomoe
So we know that melanoma, in the minority of cases, comes from pre-existing pigmented spots.
Many of these pre-existing lesions, in these cases, have always appeared normal, and were unchanging for years, present since childhood or birth.
Then the patient one day realizes that the spot’s been looking darker, or seems just a little larger.
- The big question, then, is what percentage of melanomas-from-pre-existing-moles comes from spots that were only 2 millimeters small originally?
- Only 1 millimeter?
- Only just a tiny speck?
This data has not been established. Nevertheless, by all means, during your monthly skin exams for anything suspicious or questionable, do not dismiss any tiny moles that you know have “always been there.”
This is especially true if you’re not sure that the little speck has always been there in the first place, which is why it’s a very smart idea to create a map of all your skin’s lesions.
This way, you can use it as a reference point every time you examine your skin for signs of melanoma.
 Dr. Schultz has been treating his patients’ dermatologic conditions for 30+ years, with particular emphasis in skin cancer prevention and treatment, acne treatment and laser surgery.
Dr. Schultz has been treating his patients’ dermatologic conditions for 30+ years, with particular emphasis in skin cancer prevention and treatment, acne treatment and laser surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Albina Glisic
How Much Does an Adult Sunburn Raise Risk of Melanoma?

You’ve heard that severe childhood sunburns raise melanoma risk, but what if you had no childhood sunburns, but got them as an adult?
Don’t think for a moment that the absence of a sunburn during your childhood means you don’t have to worry about melanoma.
Sunburns in Adulthood Count
“It has been commonly taught that 50 percent of sun damage occurs before the age of 18,” says Dr. Joel Schlessinger, MD, a dermatologist with a private practice in Omaha, NE.
“Dermatologists are changing their thought processes on this, however, as the abundance and availability of indoor tanning has increased.”
More and more adults are getting socked with unnatural (tanning booths) doses of ultraviolet radiation.
And let’s not forget the strong doses of sunlight from tropical vacations.
“For this reason, it is likely that sun exposure risks not only continue, but increase, as individuals age,” says Dr. Schlessinger.
“Sunburns are a sign of lack of protection and major damage to the skin. Melanomas are clearly linked to the numbers of sunburns that an individual has over a lifetime.”
The risk of melanoma from sunburns, then, does not stop when one turns 18.
Dr. Schlessinger continues, “Furthermore, sun adds up over the years and magnifies damage as well. With thinning skin as we age, individuals have less protection for their skin as they grow older.
“Many people are able to spend more money on tanning sessions as they age, which further damages their skin.
“Also, sun damage mounts over time, eventually reaching a crescendo where even small amounts of sun exposure or tanning bed exposure can cause significant and irreparable harm.”
The thing with sun exposure is that the damage isn’t instant, like the damage from a car accident.
This suppresses an adult’s awareness and insight into just how damaging cumulative sun exposure and sunburns are.
“Sun exposure doesn’t cause skin cancer right away, which unfortunately leads to people going back to the sun or tanning beds and thinking they ‘got away’ with the sessions/exposures before,” explains Dr. Schlessinger.
“This couldn’t be further from the truth. What actually happens is that they end up waiting about 20 years before the damage is evident.
“Twenty years is a long time, and during the years leading up to finding out what the initial sun exposure damage will cause, they are usually causing further damage!”
This is scary news, because for many adults, what ultimately happens is that they start developing a slew of precancerous lesions and even cancerous lesions (not necessarily melanoma). By then it’s too late to stop this cascade of recurring lesions.
“Additionally, any interventions to stop exposure will result in minimal benefits until another 20 years has passed,” says Dr. Schlessinger.
The solution is to just avoid tanning booths and unprotected sun exposure. Always wear sunblock.
Try to avoid being in the sun between 10 a.m. and 4 p.m.
Otherwise, use that sunblock and reapply every 2-3 hours, and more frequently if you’re swimming, says Dr. Schlessinger.
There are clothing lines with built-in sunscreen.
Sunburns in adulthood contribute to melanoma risk, and there is no way around this fact.
 Dr. Schlessinger, founder of LovelySkin.com, has 25+ years of experience treating many skin conditions including melanoma. He’s founder of the Advanced Skin Research Center, a clinical facility that investigates new medications and treatments.
Dr. Schlessinger, founder of LovelySkin.com, has 25+ years of experience treating many skin conditions including melanoma. He’s founder of the Advanced Skin Research Center, a clinical facility that investigates new medications and treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Chondroitin and Glucosamine Be Taken with Antidepressants?

Is it safe to take glucosamine and chondroitin with antidepressants?
Are you taking an antidepressant and would like to also take chondroitin or glucosamine?
There are certain compounds that should not be taken with antidepressants — for instance, narcotic painkillers, which can suppress the therapeutic effects of an antidepressant.
But what about chondroitin and glucosamine with antidepressants? Can taking chondroitin or glucosamine with an antidepressant create problems?
I wondered about this, and asked Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
Wegmann explains: “Chondroitin occurs naturally in the body and is a major component of cartilage — connective tissue that cushions the joints.
“Some scientific studies suggest chondroitin may be effective for osteoarthritis, but others have not shown any positive effects associated with its use.
“I cannot find any contraindications associated with taking chondroitin in conjunction with antidepressants, so I would say the combination is fine.”
What about glucosamine with antidepressants? Wegmann says: “Same as for chondroitin; taking antidepressants in combination with glucosamine is fine, no reported contraindications.”
So if you’re on a medication such as Cymbalta, Effexor, Lexapro, Zoloft, Pristiq, Paxil or Prozac, it’s perfectly okay to take chondroitin or glucosamine; neither will suppress the actions of selective serotonin/norepinephrine reuptake inhibitor (SS/NRI) drugs.
In fact, if you’re thinking of taking narcotic painkillers while on an SS/NRI, beware:
Narcotics suppress, or depress, the central nervous system; that’s how they numb pain.
Examples of narcotics are Vicodin, Norco, Darvocet, Percocet and codeine.
Since narcotics depress the central nervous system, they will “fight” against your antidepressant.
It’s quite possible that a narcotic painkiller can pretty much cancel out the effect of an SS/NRI, and/or the SS/NRI can cancel out the pain-numbing effect of a narcotic.
Another point to consider:
A possible side effect to narcotics is depression and anxiety. Of course, read the insert to your SS/NRI medication, because depression and anxiety can also be side effects of antidepressants.
However, it’s very possible to experience no side effects from a drug like Cymbalta, Effexor and Pristiq, and yet suffer miserable side effects from the use of a prescription narcotic, which can include depression and even mental confusion.
If you are having joint pain while being treated for depression, consider first taking chondroitin, glucosamine or aspirin/ibuprofen, since these will not interact with antidepressants.
Sometimes these work for pain, and sometimes they don’t, but there’s only one way to find out. Another effective treatment for joint pain is structured exercise.
 Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Do Sleeping Pills Prevent Awakening from Pain?

So will that sleeping pill keep you from waking up with pain?
If you have pain, be it from a knee injury, back injury, tendonitis in the shoulder, carpal tunnel syndrome or a pinched nerve in the neck, taking a sleeping pill will not prevent the pain from awakening you.
It’s amazing how many people will take sleeping pills, thinking that these drugs will keep pain from waking them up.
This is not what sleeping pills are designed for.
Here is what a doctor says: “Be aware that sleep aids generally do not work for sleep that is disrupted by pain,” says Joseph J. Ruane, DO, a sports medicine specialist with OhioHealth Physician Group.
In order for a sleeping pill to induce a slumber strong enough to be impenetrable from pain, the drug would essentially have to be a powerful painkiller — which it is not.
Ambien and Lunesta are frequently advertised on TV as sleep aids, not painkillers. And over-the-counter sleep drugs will be just as useless as far as enabling a person to sleep through pain.
Dr. Ruane continues: “People think sleep is sleep and a sleeping pill should help you sleep if you’re having any sort of trouble.
“Over-the-counter medicines such as Tylenol PM or even prescription medicine made to help people sleep will generally not help if pain is the problem.
“Most of the time, the body ignores sleep aids and the pain will still wake you, so don’t be disappointed.”
The mechanism by which sleeping pills assist in slumber is not the same mechanism by which, for example, narcotics like Percocet, or anti-inflammatories like ibuprofen, work.
It’s two completely different pathways. Pain will barge right through the sedative properties of a sleeping pill and awaken you.
If you are free of pain and are having trouble falling asleep due to stress, poor eating habits or outdoor noise, then a sleeping pill can aid in making you drowsy enough to eventually fall asleep and stay that way.
But if you have a recurring pain problem in, say, your hands from carpal tunnel syndrome, or migraine headaches, then that pain will override the sleeping pill – easily, and wake you up outright.
 Dr. Ruane’s practice is dedicated to comprehensive, nonsurgical musculoskeletal care. He is active in clinical research and is a nationally recognized speaker and educator.
Dr. Ruane’s practice is dedicated to comprehensive, nonsurgical musculoskeletal care. He is active in clinical research and is a nationally recognized speaker and educator.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
Cymbalta Fights Depression Caused by Narcotic Painkillers
Cymbalta is an antidepressant that can be used to treat depression caused by narcotic painkillers such as Norco/Vicodin, Percocet, OxyContin, codeine, etc.
Yes, narcotic painkillers can cause serious depression as a side effect. This side effect, if disabling enough, can be treated with Cymbalta, an SNRI antidepressant that also has an on-label use as a painkiller; namely for nerve discomfort.
I asked questions about Cymbalta for depression caused by narcotics to Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “From Fatigued to Fantastic!”
Fibromyalgia is a nerve pain disorder that causes pain throughout the entire body, and one of Cymbalta’s on-label uses is for treating the discomfort of fibromyalgia.
Suppose a person has been taking narcotics for pain and develops clinical depression as a side effect.
What do you think of taking Cymbalta (or any SNRI type of drug), to fight this depression?
This is a two-pronged question, because on one hand, the person might continue taking the painkillers, and on the other hand, the person might stop the narcotics but the depression lingers, so in essence, they transition from painkillers to Cymbalta to mop up the depression.
And in that last scenario, at what point might they quit the Cymbalta (via tapering) with the idea that the narcotic depression is long gone from their system?
Dr. Teitelbaum: “Very reasonable to add Cymbalta to the narcotic to help BOTH the pain and depression. I would likely, when both pain and depression are controlled, consider slowly tapering off the narcotic — but would be okay with continuing both as long as needed.
“I would note that I would be treating the underlying causes of the pain using “SHINE” —
Sleep,
Hormonal support,
Infections/Inflammation/Impingement,
Nutritional support, and
Exercise as able.
“Remember, pain is your body’s way of saying that something needs attention, like the oil light on your car’s dashboard. Add oil and the oil light goes out.
“Treat with SHINE, and the pain often goes away. Other treatments can be tailored to the specific type of pain as well (e.g., vitamin B6, thyroid and wrist splints for carpal tunnel syndrome).
“Six months into pain being relieved, it is reasonable to taper down the dose of pain meds if pain relief persists.”
If you’ve been incapacitated by depression that seems to have developed at about the same time you began taking narcotics, there’s a real possibility that this mood dysfunction was caused by the painkiller itself; or, the mood disorder may have been pre-existing in a milder form, and then intensified from narcotics use.
Taking Cymbalta in conjunction with your prescription painkillers to combat this secondary depression is something to strongly consider.
If you decide to ask for a Cymbalta (or other SNRI drug) prescription, your doctor needs to know that you believe your depression is being caused or aggravated by your narcotics use.
The narcotic induced depression may also be caused by B vitamin or testosterone deficiency caused by the narcotics, and these deficiencies can be easily treated.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.