Should Virgins Get Pap Smears?

Should a virgin get a Pap smear?
Pap smears are very effective screening tools for cervical cancer, which is primarily caused by the sexually transmitted human papillomavirus (HPV).
Recommendations for when women should begin getting Pap smears always reference sexual activity.
Lisa B. Bazzett, MD, a gynecologic oncologist (cancer specialist) at Ochsner Medical Center in New Orleans, states:
“The current recommendation for initiation of Pap smears from the American College of Obstetricians and Gynecologists is that girls and women should begin cervical cancer screening approximately three years after initiation of sexual intercourse, but no later than age 21 years.”
Where do virgins fit in here as far as Pap smears?
Every single time we see something about women and Pap smears for cervical cancer, there never seems to be any mention about how this may or may not apply to virgins. So I began wondering, Should virgins get a Pap smear?
Or are virgins exempt from HPV transmission? I posed this very interesting question of whether or not virgins should get Pap smears, to Dr. Bazzett.
Do virgins need to get Pap smears?
Dr. Bazzett: It is true that HPV is transmitted during intercourse, but it can also be transmitted during other, non-penetrative, sexual acts.
This is due to the mode of spread of the virus being different than other sexually transmitted diseases that are transmitted in bodily fluids. HPV is not transmitted in bodily fluids, but in skin to skin, or surface to surface contact.
Therefore, if two individuals engage in close contact of the genitals, but don’t actually have “penetrative intercourse,” the virus can still be transmitted.
This is why it’s safer to simply choose an arbitrary age to begin screening, even if a women is a “virgin,” because there are other sexual acts that may transmit the virus that a patient would not necessarily consider “sex” when her sexual history was being taken by a healthcare provider.
But if a woman is a virgin, chances are pretty high that she also abstains from any close contact of the genitals.
A woman who chooses to stay a virgin (regardless of reason) will typically avoid all close contact with the genital area.
So, to refine my question, should committed virgins, or nuns, for that matter, get Pap smears?
Dr. Bazzett: It is reported that 99% of all cervical cancers are caused by HPV. There is a very rare type unrelated to HPV that most gynecologic cancer specialists will see only once or twice in their careers, as opposed to the unfortunately all too common HPV-induced cervical cancers.
HPV is also responsible for other female gynecologic cancers including the vagina, the vulva and the anus.
Therefore, it is certainly much safer to include virgins in the standard cervical cancer screening recommendation, with yearly Pap smears, than to miss an HPV related disease in its precancerous, curable state.
So this means that virgins, i.e., women who have never even been on a date, should nevertheless get Pap smears?
Dr. Bazzett: The recommendation from ACOG is yes, at age 21, and I would never go against that recommendation.
As I stated, there is a very rare type of cervical cancer unrelated to HPV, and to simply not do Pap smears, or exam of the cervix or genitalia in a woman, could put her at risk, so I would still recommend a Pap smear at age 21.
If a woman is a virgin and not engaging in any sexual activity, it is always up to the discretion of her and her physician what is best for her.
She may not need a Pap every year, but should still be getting a pelvic exam, as there are other problems that can arise from the uterus, the ovaries, that require yearly pelvic exams.
 Dr. Bazzett specializes in the treatment of malignancies of the female reproductive organs including that of the ovary, uterus, cervix, vagina and vulva.
Dr. Bazzett specializes in the treatment of malignancies of the female reproductive organs including that of the ovary, uterus, cervix, vagina and vulva.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Ovarian Cancer May Be Caused by Too Many Periods

Too many periods may contribute to the cause of ovarian cancer — the deadliest of all gynecological cancers.
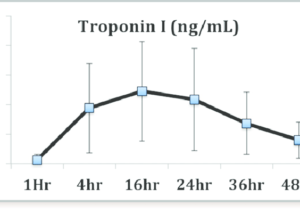
Atrial Fibrillation & Elevated Troponin: Prognosis

An episode of atrial fibrillation may cause a mild elevation (“indeterminate range”) in troponin, but does this relate to a mortality or heart attack risk?
“In of itself, A-Fib does not cause a rise in troponin unless underlying coronary artery disease is also present,” says Dr. Adam Splaver, clinical cardiologist and co-founder of NanoHealth Associates, a practice that explores the molecular level of cardiovascular disease.
If atrial fibrillation is a suspected issue in a patient who presents in the ER with mildly elevated serial troponin results (that are falling), the next course of action would be to monitor the heart rhythm outside the hospital setting.
“Holter monitors, event recorders and loop recorders are just a few of the tools used to detect this arrhythmia, or disturbance in the heart’s normal rhythm,” says Dr. Splaver.
A-Fib is not treated with any kind of implanted device, but instead, with medications or ablation.
But it first has to be established that a patient even has A-Fib — and that’s done with the event monitors.
According to a report in the European Heart Journal, a mild elevation in troponin I in patients with atrial fibrillation is associated with increased risk of cardiac events and mortality. The report’s abstract states:
In patients with atrial fibrillation, minor troponin I elevation is regularly detected.
The study authors conclude that their findings may be important for risk stratification in such patients.
A report in Circulation has the same conclusion, except that the subjects also had an accompanying rapid ventricular rate:
Even mild troponin elevation in the setting of AFib with RVR predicts a significant increase in risk of MI at 1 yr. MI means a heart attack.
What would be very intriguing is a study of subjects, who’ve had CABG (coronary bypass surgery), who’ve had a mildly elevated troponin result as a consequence of atrial fibrillation.
Would the presence of bypass grafts impact the risk of future cardiac events and mortality?
Would it be slightly lower than patients in the same boat (severe heart disease) but who never had revascularization (bypass surgery)? Would the difference be negligible?

Dr. Splaver is board certified in cardiology, internal medicine and echocardiography, and is a registered physician in vascular interpretation and trained in age management medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources:
eurheartj.oxfordjournals.org/content/32/5/611.full
circ.ahajournals.org/cgi/content/meeting_abstract/118/18_MeetingAbstracts/S_818-a
Is Colon Cancer Always Caused by Polyps?

Though most colon cancers arise from what was once a benign (and removable) polyp, there are a number of circumstances in which the tumor starts growing without first transforming out of a polyp.
Not all cases of colon cancer are caused by polyps.
Colon cancer usually arises from polyps, but the question then becomes: Is colon cancer always caused by polyps?
All we seem to hear about in the media is how polyps can be discovered in a routine colonoscopy and removed, thereby going a very long way in preventing colon cancer, since malignancies can arise from these polyps if not removed.
Greater than 90 percent of colon tumors are believed to “go through the polyp cancer sequence over many years,” says Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
“Examples where these trends do not apply include familial genetic syndromes (i.e., hereditary non-polypyosis colorectal cancer syndrome HNPCC, familial polypyosis), inflammatory bowel disease, ulcerative colitis and Crohn’s disease, immunosupressed patients.”
How could it be discerned that ulcerative colitis and Crohn’s can lead to non-polyp colon cancer?
Dr. Jones explains, “By non-polyp colon cancer, we mean that the usual small polyp to large polyp to early cancer to late cancer (about 10 years for these changes to occur) is skipped or accelerated.
“Persons with Crohn’s colitis or UC should undergo more frequent screenings after 10 years’ duration of disease, because of just this pattern of tumor growth.
“There are many reports in this population of inflammatory bowel disease who have developed cancers in the period between surveillance intervals presumptively from an accelerated carcinogenesis (genetic pathway).”
How often should this population, after 10 years’ disease, have colonoscopy screenings?
Dr. Jones explains, “Once the diagnosis of Crohn’s or ulcerative colitis (the more of the colon involved, the higher the risks of cancer development with ulcerative colitis) has been made, then regardless of the age of diagnosis, an increased screening regimen should begin after 8-10 years.”
Suppose a doctor discovers a malignant tumor upon colonoscopy. Is there a way for lab analysis to determine if the mass arose from a polyp, versus colon cells (no polyp transition phase)?
Dr. Jones says, “Yes, by pathology. The fact is that in almost all colon cancers, there is associated adenomatous tissue within the specimen. These findings are what lead in part to the polyp — cancer sequence theory.
“A variety of new genetic tests, including micro-satellite instability assays, are available and emerging.
“These tests also help us prognosticate on the tumor behavior after tumor removal.”
Why would inflammatory conditions increase risk anyways?
Dr. Jones says, “There are direct effects on the DNA through inflammatory pathways leading to DNA mismatch, repair errors, proto oncogene activication, and others.”
Dr. Jones emphasizes that the best time to be screened for colon malignancy is when you have no symptoms and are feeling just fine.
Waiting until symptoms set in means that a colonoscopy is no longer a screening procedure; it’s a diagnostic procedure — to find out what’s wrong. Don’t wait.
Colon cancer symptoms are typically not warning signs of early disease; they mean the disease has spread beyond the colon.
The emphasis by the media is on polyps that have the potential to transform to cancer in the colon.
But as you have just read, there are circumstances under which a colon cancer can develop without first being a benign polyp.
All of this can sound frightening. Getting regular colonoscopies can ease your fear tremendously.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Rabbit2Dsign
Colon Cancer in People Who Didn’t Have Routine Colonoscopy
What percentage of people, diagnosed with colon cancer, did not have a colonoscopy within 10 years of the diagnosis?
Colonoscopies to screen for colon cancer are recommended every 10 years beginning at age 45 for people at average risk for this disease, the second-leading U.S. cancer killer of men and women combined.
The colonoscopy is a marvel of modern medical technology in that it can detect precancerous changes in the large colon, years before these abnormal cells mutate into full-blown malignancy.
As amazing as this technology is, why is colon cancer so prevalent in the U.S., with over 139,000 new cases (men and women combined) in 2006?
As for that percentage of people newly diagnosed with colon cancer, who did not have a colonoscopy within 10 years of this crushing diagnosis, “This figure is not well-documented,” says gastroenterologist Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
“The vast majority of colon cancers are diagnosed in people who have never had a prior colonoscopy.
“In my own practice (1994-present), I have had five people diagnosed with colon cancer within the intervals which should have been appropriate for screening or surveillance purposes.
“Versus approximately 300 who have been diagnosed with colon cancer at their first index colonoscopy for screening or at a diagnostic colonoscopy for digestive signs or symptoms suggestive of colon cancer.”
Colon cancer is not a “man’s disease.”
Though slightly fewer women in the U.S. are diagnosed as compared to men, the 2006 statistic has women coming in at just over 1,400 cases fewer, out of that 139,000-plus total.
So if you’re a woman, don’t assume you have some natural gender protection against this frightful disease.
Contrary to what some people, who’ve had colonocsopies, claim, preparing for it is not as “messy” or as “uncomfortable” as it’s sometimes made out to be.
The prepping involves ingesting only clear liquids, which include soda, the day prior to the exam.
And then you must drink quite a bit of a laxative that has a slightly syrupy texture.
The result is that you will be going to the bathroom quite often and expelling very liquidy diarrhea.
This is to clean out the GI tract so that the doctor can have the best view of it during the exam.
If during the colonoscopy, the doctor discovers a polyp, he will remove it and send it out for a biopsy.
Polyps have the potential to transform into malignancy.
By the time colon cancer causes symptoms, the disease usually has spread outside the intestinal cavity.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: ©Lorra Garrick
Source: cdc.gov/cancer/colorectal/statistics/
Can Colon Cancer Be Prevented with a Colonoscopy Every 10 Years?

Would a routine colonoscopy prevent colon cancer if done every 10 years, since this type of cancer grows so slowly and usually starts as a benign polyp?
The colonoscopy is a marvel of medical technology that allows physicians to detect precancerous growths in the large colon called polyps.
If you know that colon cancer can take years to develop (and hence why a routine colonoscopy is recommended for average-risk people every 10 years beginning at age 45), you may wonder this:
If, in a 45-year-old who has a clean colonoscopy, colon cancer can be prevented. if he or she continues having colonoscopies every 10 years?
After all, how quickly can a polyp form and morph into a malignancy between 10-year screenings?
“First, there are outliers in terms of age of cancer development; some sporadic cases in their 20s or 30s,” begins Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
“The 40-year age group is a different question altogether.”
Thus, the question pertains strictly to average-risk (of colon cancer) people who begin having the routine colonoscopy.
Unless there is a family or personal history of colon cancer, a person will not be advised to begin colonoscopy screening until age 45 according to the U.S. Preventive Services Task Force as of 2021.
Dr. Jones continues, “Second, there are outliers in terms of the biological behavior and rapidity of growth of the classic polyp-to-cancer sequence that have aggressive growth, resulting in cancer in small growths that evidently turn into cancer, and may even spread to blood vessels and lymph nodes while being very small (i.e., sub 1 centimeter).”
Finally, Dr. Jones explains that there are technical issues. He says, “All cancer screening tests are by their nature imperfect:
“Polyps are missed (up to 10-15 percent); blind spots for the endoscopist in the colon are a reality despite evolving technology; preps are not always optimal; there are significant performance differences between individuals who perform colonoscopy.
“Standardized preps including split dose preps, withdrawal time tracking and adenoma detection-rate tracking are helping endoscopists improve on this third and important variable.”
Despite the “imperfect” nature of the colonoscopy, it’s a glaring fact that the number of people who avoid colon cancer screening via colonoscopy is directly related to the mortality rates of this disease.
By the time symptoms first start presenting (e.g., change in bowel habits, change in stool caliber, diarrhea, blood in stools, ribbon-like or pencil-thin stools, abdominal pain, nausea, vomiting, fatigue, unexplained weight loss, constipation — especially if it alternates with diarrhea), the malignancy has likely already spread beyond the large colon and even into surrounding organs.
Thus, routine colonoscopies are life-saving and make a tremendous difference in the development and survival rates of colon cancer.
Note: If you have any of the above symptoms, don’t jump to the conclusion it must be a malignancy.
The above symptoms are common and can be explained by many benign gastrointestinal disorders.
However, if symptoms haven’t resolved within two weeks, see a gastroenterologist — with the exception of bloody or “tarry” stools: In that case, make an appointment ASAP.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Chinnapong
Why Do Colonoscopies Normally Begin at 45? Why Not Sooner?

There’s good reason why 40 is that “magical” number for when a typical person should begin getting colonoscopies for colon cancer screening.
A colonoscopy is a minimally invasive procedure that can detect colon cancer, or precancerous polyps.
“Colon cancer is generally a disease of the elderly,” says Mitchell S. Cappell, MD, Chief, Division of Gastroenterology & Hepatology, William Beaumont Hospital, Royal Oak, MI.
“Nearly 95 percent of colon cancers occur in people more than 50 years old.
“This phenomenon is due to the fact that colon cancer generally comes from chance biochemical abnormalities, called mutations, in the genes (DNA) of individual colon cells.”
Colon cancer (like all malignancies) does not happen overnight; there are a number of stages of transformation that a healthy cell undergoes before it becomes a malignant cell.
In the case of colon cancer, a normal cell, due to accumulated mutations, will proliferate out of control, initially forming a benign polyp – which a colonoscopy can detect. On the spot, the physician removes the polyp(s).
If you don’t have screening for colon cancer, the polyp will continue growing and may sustain more mutations – enough to morph it into a malignant tumor.
Dr. Cappell explains that this disease “occurs mostly in the elderly because this sequence of changes, the accumulation of chance mutations, is a long process that takes many years.”
This doesn’t mean that people younger than 45 are immune to colon cancer.
Dr. Cappell adds, “About 2 percent of people developing colon cancer are younger than 40 years old.
“About 20 percent of people who develop colon cancer when less than 40 years old have special risk factors that place the patient at a very high risk of developing colon cancer.”
These risk factors are 1) familial polyposis coli (abbreviated as FPC), and 2) Lynch syndrome (also called HNPCC).
In FPC, patients have many benign polyps, and malignancy is likely because out of so many polyps, it’s inevitable that one or more will become malignant.
In Lynch syndrome, the patient develops just a few benign polyps, but these particular polyps have an intrinsically high risk of morphing into colon cancer.
“Patients less than 50 years old generally do not undergo screening for colon cancer because they have much lower risks than patients more than 50 years old,” continues Dr. Cappell.
If someone is diagnosed with FPC or Lynch syndrome, he or she will be urged to have colonoscopies beginning at a much younger age.
Just how young can a person getting a colonoscopy be?
Dr. Cappell says, “Patients with a close blood relative with familial polyposis coli need colonoscopy at a young age, during their early teens, to diagnose or exclude this disorder.
“Likewise, close blood relatives of patients with Lynch syndrome need early colonoscopy beginning in their mid-20s.
“Patients with a family history of colon cancer in first degree relatives (e.g., mother or father) should generally undergo colonoscopy at age 40 years or earlier.”
So if you’re 25 and have no family history of this dreadful disease, and do not have Lynch syndrome or FPC, this does not give you the green light to practice lifestyle habits that are risk factors for colon cancer, such as:
1) a sedentary lifestyle, 2) a meat-based diet, 3) eating lots of processed meats, 4) diet low in fiber, high in “bad” fats, and 5) smoking and heavy drinking.
You have no green light because, as Dr. Cappell explains, colon cancer (in the absence of Lynch syndrome or FPC) is decades in the making, and how you treat your body during your younger years influences your risk of developing the disease.
Dr. Cappell says, “In summary, colon cancer usually occurs in patients more than 50 years old, and colon cancer is unusual in patients less than 50 years old. However, no age group is immune from colon cancer.
“I saw and diagnosed one patient with incurable colon cancer at age 20, a few weeks before his planned wedding.”
Symptoms of this Common Disease
Constipation, diarrhea, and especially with a recent dramatic shift in bowel movements (such as from regular bowel movements to constipation); blood in the stools (may be bright red, or tar-like); abdominal pain; abdominal bloating; unexplained weight loss; unexplained fatigue; and appetite suppression.
Note: Having some of these symptoms doesn’t mean you have the disease.
In fact, the symptoms of irritable bowel syndrome can be very similar, though over time, in untreated colon cancer, the symptoms will get worse.
“Colon cancer may also present as anemia due to iron deficiency unexplained by blood loss during menstrual periods or by numerous childbirths,” says Dr. Cappell.
“Patients should routinely undergo screening colonoscopy at age 50 years even without symptoms or risk factors for colon cancer.”
Recommended Age to Begin Screening for Colon Cancer Drops in May of 2021
The U.S. Preventive Services Task Force (USPSTF) updated their guidelines in 2021 to recommend that individuals of average risk begin colon cancer screening at age 45.
This recommendation applies to people who are at average risk for colorectal cancer and doesn’t take into account any other risk factors like family history or genetic predisposition.
Dr. Cappell has been in practice for over 30 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Nasal Congestion Relief: Humidity vs. Dry Air
You’ll be surprised which turns out the winner between humidity and dry air when it comes to nasal congestion relief, and why.
The kind of air you breathe, in terms of how dry it is or humid it is, can significantly impact the perception of nasal congestion.
The feeling that you have congestion, or a stuffed-up nose, is not necessarily related to actual mucus buildup in the sinuses.
Rather, the sensation of a stuffy nose can originate from the airflow through the nasal passages.
“It’s very common for the nose to feel congested or blocked without mucus,” says Inna Husain, MD, an ear, nose and throat specialist with Community Healthcare System of Indiana.
“The lining and tissue of the nose can congest and decongest in response to inhalant allergies, but what most people don’t know is that it is also affected by non-allergic stimuli such as temperature.”
This can explain why your nose feels stuffed or blocked, yet no matter what you do, nothing comes out, even after irrigating the nose.
The Monell Chemical Senses Center
Monell Center researchers found that the sensation of nasal congestion relates to air temperature and the level of humidity.
So if you’re one of the 33 million people in the U.S. with a nose that feels blocked up, keep reading.
Perhaps you’ve seen a doctor and he couldn’t find any physical cause of your sinus congestion.
You may actually have a sensory-related issue.
When the feelings of nasal congestion are sensory-related, says the research, this opens doors for more targeted treatment.
One example of a targeted treatment is that of focusing on restoring the optimal humidity and temperature in a patient’s nasal airflow.
The Monell study had 44 healthy participants breathe air from three boxes and then rate any symptoms of a nasal congestion.
One box contained cold air; the second box contained room temperature dry air; and the third offered room air that was at normal humidity.
Which box produced the lowest report of sinus congestion? The cold air box.
Reduced nasal congestion was also perceived when the participants inhaled from the dry air box.
The room air, normal humidity box did not result in these perceptions.
In short, lower humidity was found to be associated with reduced sensations of nasal congestion.
Nasal cooling is influenced by the interaction of humidity and air temperature as air moves through the nose’s cavities, say the researchers.
“Cool sensors” in the nose detect the nasal cooling, and the detection can feel like easy breathing — or obstructed.
The researchers point out that if someone is in a desert, with all other things being equal, they should feel less congested than if in a jungle.
That’s becauuse a desert has low humidity. This means more evaporative cooling inside their nose, making the temperature of their nasal passages lower.
This creates the sensation of a greater airflow.
Additiona Reasons for a Blocked Feeling in Both Nostrils

Shutterstock/natali_ploskaya
“There is also a process known as the nasal cycle which is the spontaneous congestion and decongestion of nasal mucosa that cycles side to side,” says Dr. Husain.
“Also, nasal congestion or obstruction can occur due to structural reasons in the nose — for example, a septal deviation.”
 Dr. Husain is an otolaryngologist affiliated with Community Hospital, Munster, IN, Community Stroke and Rehabilitation Center, Crown Point, IN, and St. Catherine Hospital, East Chicago, IN. She received her medical degree from Southwestern Medical School at Dallas. Follow her on Instagram and TikTok.
Dr. Husain is an otolaryngologist affiliated with Community Hospital, Munster, IN, Community Stroke and Rehabilitation Center, Crown Point, IN, and St. Catherine Hospital, East Chicago, IN. She received her medical degree from Southwestern Medical School at Dallas. Follow her on Instagram and TikTok.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2011/10/111013184803.htm
Hearing Loss from Motorcycles: Engine vs. Helmet Wind
Which is worse for the motorcycle rider’s hearing: the roaring engine or the roaring wind?
Hearing loss is a real threat to the toughest motorcycle rider, and it seems as though the volume of wind noise gushing past a helmet has gotten much more attention than the volume of the bike’s engine.
“Both can be damaging to the ear — but surprisingly few motorcyclists realize the risk to their ears,” says Rivka Strom, AuD, CCC-A, chief audiologist at Central Hearing LLC in NY.
“Studies have shown wind noise to be high in level and increasingly louder as the speed picks up.
“Although there are helmets to protect motorcyclists’ ears, they are not always efficient at reducing necessary levels, and each one must be evaluated for effectiveness for the rider.”
A Study Shows the Loudness of Wind Against a Helmet Using Microphones
A study in 2011 by researchers at the University of Bath and Bath Spa University placed microphones at varying locations around a helmet that was on a mannequin’s head, to determine the precise location of greatest volume of wind noise (produced by fans for this study).
However, it had, by the time of the study, already been well-documented (e.g., McCombe) that the “whooshing” wind sound over a biker’s helmet as he speeds down roads will surely lead to some degree of hearing loss.
The greater attention to the helmet issue may be because few motorcycle riders would ever suspect wind rushing over a helmet as a possible cause of hearing loss.
Though the helmet wind volume may exceed a particular bike’s engine volume, this in no way invalidates the potential for motorcycle engines to play a prime role in hearing loss.
Consider that often, a biker will rev the engine while in idle. The biker gets plenty of loud-engine exposure without the noise of wind stealing the show.
So just how loud is a motorcycle’s engine?
University of Florida researchers revved up the engines of 33 different bikes:
About half delivered volumes over 100 decibels (a dB is a unit of sound volume). In fact, at 65 mph, a motorcycle’s engine can reach up to 116 dB.
The Occupational Health and Safety Administration warns that exposure to 100 dB is safe for only 15 minutes.
The University of Florida report says that nearly all the motorcycles that were tested reached “action-level noise, which in the workplace would require ear protection.”
A motorcycle enthusiast may think, “Well, what’s a little damage from my engine or helmet, what with all the rock concerts I attend?”
A rock concert can generate volume at 120 dB, which, according to OSHA, is safe at only seven and a half minutes of exposure!
The motorcycle rider may also figure why bother worrying about engine and wind noise, when he spends a lot of time using power tools?
Every bit of concern helps.
A motorcycle rider should wear earplugs. Custom-made work best and last a lot longer than store-bought ones.

Dr. Strom is a member of the American Speech Language and Hearing Association and has received several awards including Brooklyn College’s Excellence In Audiology Award.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sources:
sciencedaily.com/releases/2011/07/110729175559.htm
ncbi.nlm.nih.gov/pmc/articles/PMC539364/ mcCombe
hear-it.org/page.dsp?page=3597
motorcyclecruiser.com/streetsurvival/0710_crup_motorcycle_hearing_protection/index.html
Baldness Increases Skin Cancer Risk; Bald Men Beware

Bald men need to be aware that, though bald may be beautiful, bald can also be deadly.
Though skin cancer that grows on the scalp comprises only 2 percent of all skin cancers, this is actually a significant percentage, because every year in the U.S., over a million skin cancer cases are diagnosed.
Two percent of one million is 20,000. If you’re balding, that figure is nothing to sneeze at.
“The top of the head (and back of the neck) is something many guys forget about,” says Adam J. Mamelak, MD, a board certified dermatologist and founder of Sanova Dermatology in Austin, TX.
According to the journal Dermatologic Surgery, a certain type of skin cancer of the scalp can be particularly aggressive.
This skin cancer is called squamous cell carcinoma, and about 250,000 Americans are diagnosed with it every year.
A balding and especially completely bald head is highly vulnerable to sun damage.

Freepik.com
In fact, according to the Journal of the American Academy of Dermatology, about 90 percent of visible changes to skin are incorrectly blamed on aging, when in fact, they are caused by sun damage.
So why is that bald head at such notable risk for skin cancer?
First of all, think of all the exposure a bald head or partially bald pate gets to the sun.
Secondly, people tend to subscribe to the idea that if you can’t see something, you don’t need to worry about it.
How many bald or partially bald people even occasionally take a look at their scalp, let alone inspect it on a monthly basis?
Other variables are at play here, because a bald man may be tall; how many family members are taller than him such that they can spot suspicious lesions on top of his head?
If the baldness is the type where sparse strands of hair are combed over the skin surface, the presence of the hair can mask much of the cancerous or precancerous lesions.
And here’s another variable: A man may think he has a full crop of hair on top of his head, when in fact, he has a nice bald spot there, one that exposes skin to significant amounts of sun.
And if you are bald, and you faithfully use sunblock, when’s the last time you actually applied sunblock to your scalp, especially if you have sparse strands of hair over it?
“You can apply sunscreen to the top of the head,” says Dr. Mamelak. “It works well, just like it does on other parts of the body.
Sparse strands of hair, or the infamous “comb-over,” do not protect skin from cancer.
“Wearing a hat, however, is probably the easiest and best way to protect your head from harmful UV rays,” says Dr. Mamelak.
“A hat with a wide brim is even better, as it shades and covers the ears from sun damage.”
Does your primary care physician examine your scalp during annual physicals?
Request that your doctor do so, even if you yourself have been doing so (which should be monthly).
The layperson can miss an early squamous cell carcinoma, basal cell carcinoma and precancerous lesions.
In fact, precancerous lesions can be very faint and hardly visible. Have your partner inspect your balding pate on a monthly basis.

The light pink patch is a precancerous lesion. Source: Future FamDoc/CC






























 Dr. Mamelak
Dr. Mamelak