Which Lowers Stroke Risk More: Off Pump or On Pump CABG?
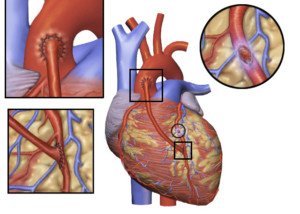
Stroke is a real risk during and following coronary bypass surgery — which may be on or off pump.
There are actually four kinds of CABG, but which one has the lowest risk of stroke?
The four kinds of CABG are:
1) Off-pump, or “beating heart,”
2) On-pump with beating heart,
3) On-pump with a stopped heart,
4) On-pump with hypothermic circulatory arrest (the body is cooled; the heart is stopped; circulation is at a near standstill).
The risk of stroke is present in all four coronary bypass surgery strategies.
“There are many articles that show a decreased stroke risk with off pump CABG,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“This is thought to be due to less manipulation of the ascending aorta — no need for cross-clamp, cannulation, and no need for the unnatural state of being on the heart/lung machine,” explains Dr. Fiocco.
“Conversely, there is data that shows no difference in stroke rates between off and on pump.
“This may be due to patient selection, surgical technique and even the degree of postop anticoagulation.
“Our own data shows a decrease in stroke with off pump surgery to less than 1%. Oddly, it is not 0% with off pump.”
What about beating heart surgery plus the cardiopulmonary bypass (pump)?
A 2011 issue of the Journal of the American Medical Association reports on a study of over 45,000 patients who had CABG between 1982 and 2009.
On pump with a beating heart showed to have the lowest risk of stroke.
Over the past 30 years, says this study, the risk of stroke from CABG procedures has decreased.
The study that’s in JAMA reported that, of those 45,000-plus patients, 705 (1.6%) had a stroke.
Of these 705 patients, 58% had their stroke post-surgery, and 40 percent had their event during their coronary bypass.
The study identified stroke risk factors during and post-CABG as being:
Stroke history, older age, atrial fibrillation (abnormal heart rhythm) prior to the coronary bypass, and type of CABG: on-pump with the hypothermic circulatory arrest.
This is the type of CABG that my mother underwent, and, no pun intended, it was quite chilling to hear the doctor describe how he was going to perform this surgery (a quintuple bypass).
My mother did not have a stroke; the surgeon had informed me that the risk was “one to three percent.”
In the study, the on-pump with hypothermic circulatory arrest had a stroke rate of 5.3%.
The lowest rate (zero percent, actually) was for the on-pump with beating heart.
The second lowest rate (0.14%) was for off-pump. And for on-pump with stopped heart, it was 0.50 percent.
So why has the incidence of stroke decreased during the CABG or post-operatively?
The researchers attribute this to better preoperative assessment, improved anesthesia and surgical techniques, and post-surgical care.
The overall picture, however, is that stroke risk is lower with off pump CABG (beating heart) than with on pump (stopped heart).

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2011/01/110125172309.htm
Is Same Day Angiogram, Bypass Surgery, Valve Replacement Safe?

Can angiogram, bypass surgery and valve replacement be done in the same day?
And if so, how life-threatening could this trio be?
Coronary angiogram, coronary bypass surgery with heart valve replacement, all in the same day — it was done with my mother.
In the same day she had a coronary angiogram, coronary bypass surgery and mitral valve replacement.
The catheter angiogram is an invasive procedure that carries the following risks: cardiac arrest, blood clot, arterial damage and infection.
The angiogram is the gold standard for detecting blockages in coronary arteries as a result of heart disease.
If the blockages are extensive enough, a surgeon will deem the situation an emergency and want to operate as soon as possible.
Otherwise, delaying the coronary bypass surgery by even a few days can put the patient at risk if a heart attack is imminent.
“Your mother is stabilized,” I was told by the internal medicine doctor after I learned she needed quintuple bypass surgery.
She had undergone an angiogram and the worst I had expected was the need for a stent or balloon angioplasty.
Imagine my horror when the internal medicine doctor said, “She’s going to need bypass surgery.”
I was a bundle of nerves as I waited in the corridor after the doctor went back into a restricted area.
Soon, I was told that the surgery would be sometime next week; it was now Friday, and I was concerned that in the interim, she’d have a heart attack.
I didn’t feel too confident that the heparin drip and supplemental oxygen would be very preventive.
Neither did the cardiothoracic surgeon; next thing I knew, a doctor told me that the surgery would be “this evening.”
This spared me the anxiety of having to wait several days for it and fear that during that several days’ wait, a heart attack would come.
I was also informed that she had mitral valve regurgitation and would require a tissue valve replacement; the tissue would be from a pig.
I asked if there was any danger in performing the coronary bypass surgery so soon after the invasive angiogram, and I was told that there was no great danger there (I don’t recall the specific words, but the translation was: no great danger).
It’s not uncommon for someone to undergo coronary bypass surgery the same day as a catheter angiogram.
This is called emergent coronary bypass surgery; the image shows vessels so severely blocked, that the physician determines that a heart attack can happen at any time, and thus, decides to perform the operation as soon as possible.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ChaNaWiT
Does the Heart Lung Machine Cause Cognitive Impairment or Not?
The heart-lung machine used in coronary bypass surgery is a two-edged sword.
The cognitive problems that are associated with it have led to the name “pump-head” to describe some patients who — seemingly — are in a permanently worsened cognitive state since their coronary bypass surgery.
“Although there may be temporary cognitive impairment after open heart surgery, this resolves over several weeks,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“It is difficult to determine if this is only related to cardiopulmonary bypass, but more likely is due to multiple factors.
“Sleep deprivation, narcotic pain meds, change in environment, and the stress of this physical and emotional trauma all are likely contributors.”
What about alleged cases of permanent worsening of mental faculties that were noted only since the bypass operation?
Dr. Fiocco explains, “Long-term cognitive impairment is rare and almost always associated with preop subtle cognitive loss that has gone undiagnosed — and is brought to light by this stressful event.”
There simply has not been any way to determine just how many patients — with perfectly intact cognitive function prior to cardiopulmonary bypass — ended up permanently cognitively impaired after the procedure.
For all we know, there may be patients who experienced that temporary post-surgical cognitive impairment that Dr. Fiocco mentions — and it lasted perhaps around two months.
But in the course of the last month, by sheer coincidence, the patient began showing the first early signs of dementia — which would have occurred even without the heart surgery.
But due to the coinciding timeline, the dementia (or “cognitive impairment”) is blamed on the heart-lung machine.
In such a patient, just as the temporary effects of the surgery and all of its associated stressors are beginning to resolve, the first signs of dementia are kicking in, overlapping.
This scenario is entirely possible because so many CABG patients are over 65.
Many may die (of any cause) before a formal diagnosis of Alzheimer’s disease is made.
Absence of this diagnosis strengthens the argument that the heart-lung machine can cause permanent cognitive impairment.
Nevertheless, it’s a hardcore fact that for many patients, the post-op period includes mental impairment to some degree.
A Research Study
A research team set out to see if minimizing surgical trauma to the heart’s aorta during bypass surgery would cut down on the post-op cognitive problems.
The study results appear in the Journal of Thoracic and Cardiovascular Surgery (Jan. 21, 2006) and was conducted by Wake Forest University School of Medicine.
Beginning in 1992, the team from Wake Forest has been investigating the cognitive problems that proceed coronary bypass surgery when the heart-lung machine is used.
For the study, 237 patients were involved. Some patients had the coronary bypass surgery with the heart-lung machine plus standard manipulation of the aorta (cross-clamp), while others had the same operation except a single clamp was used.
The single clamp moves the aorta less than does the cross-clamp.
Surgery without the heart-lung machine was also in the comparison.
The patients received psychological tests before their operations, then 3-5 days after, then 3-6 weeks after, and then six months after.
The Results
One week after the operation, at least 60 percent of the subjects in all three groups (1: heart-lung machine with cross clamp; 2: heart-lung machine with single clamp; 3: no heart-lung machine and thus no aortic clamping) had neurological deficits.
After six months, group 1 had the highest percentage (57 percent) of remaining neurological deficits.
Group 2 and 3 had percentages of 30 percent and 32 percent, respectively.
Wake Forest’s researchers’ monitoring techniques track particles — emboli and gaseous bubbles — that make their way to the brain during standard coronary bypass procedures. The emboli are believed to be the cause of the deficits.
The people who did not have the heart-lung machine during their bypass had much fewer emboli than subjects who had the heart-lung machine plus the cross clamping.
Keep note that this is an older study, but even today, there is still speculation when it comes to the heart-lung machine.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2006/01/060123165002.htm
Beating Heart vs. Heart Lung Machine in Bypass Surgery

If you need bypass surgery you might wonder about having it done without the heart lung machine and instead with the “beating heart” procedure.
The absence of the heart lung machine is called off-pump or beating-heart bypass surgery, and research has shown that it reduces the problems that are associated with the heart lung machine.
A 2007 Journal of Cardiac Surgery reports that off-pump procedures are a safer option than heart lung machine procedures and reduce complications.
Off-pump surgeries also reduce hospital stays and costs, cut the need for blood transfusions and have been shown to reduce respiratory dysfunction.
But does this mean that off-pump heart bypass has advantages over cardiopulmonary (heart lung machine) bypass?
“I once was performing 80% of my CABG case off pump, but have cut back to 10% because the data just doesn’t support it as beneficial,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Logically, one would think that eliminating the heart lung machine and all that goes with it (large cannula in the aorta, clamping the aorta, etc.), the patient would have fewer complications, but that is not the case.
“It is now reserved for those who are sicker, e.g., COPD, kidney insufficiency, calcified aorta, etc.
“There is clearly a benefit in those patients, but the low risk patient doesn’t seem to benefit.
“Also, it is technically more demanding, so most surgeons shy away from it.”
Prepping for Cardiopulmonary Bypass
In order for the heart-lung machine to be used, certain things must be done to the patient’s body.
For example, the heart is bathed in high-potassium fluids that stop the beating.
Tubes from the heart lung machine are connected to the heart, and the blood is rerouted into this device.
The blood comes in contact with the membranes of a porous plastic (where it is believed the blood may pick up micro-particles that eventually end up in the patient’s brain, causing cognitive problems).
But the blood must be routed this way to be oxygenated. It’s also cooled to around 82 degrees before being pumped back into the patient’s body.
The patient’s body temperature is also dropped. It is believed that after surgery is completed, quickly rewarming the patient’s body poses higher risk of cognitive damage than does gradually rewarming it.
That all sounds like a tremendous amount of prep activity, but the overall picture is that on-pump heart surgery is less tedious to carry out than is off-pump.
The heart lung machine does increases risk of stroke two to four percent, and can induce kidney damage, plus heighten risk of post-op infections.
Though earlier studies have linked the heart lung machine to residual post-op cognitive issues, newer research shows that the greatest predictor of post-op cognitive issues is the patient’s pre-surgical mental state, says Dr. Fiocco.
Your Surgeon Has Probably Never Performed Off-Pump Heart Surgery. This Is Not a Shortcoming.
The beating heart technique was pioneered way back in 1965 by a Russian surgeon, but not received with open arms in the States.
However, in the mid-1990s, the off-pump procedure was revisited due to development of new tools that stabilize small areas of the heart, permitting the surgeon to create bypass grafts.
At around 1996, just one percent of cardiothoracic surgeons were trained in off-pump surgery.
As of around 2004, nine percent of coronary bypasses were done without the heart lung machine.
Though beating heart bypass surgery is still not the norm and not considered standard, it’s been performed on over 45,000 people worldwide as of 2001.
And as scary as the heart lung machine sounds, the big picture is that the vast majority of the hundreds of thousands of patients every year in the U.S. who undergo on-pump surgery have successful outcomes.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pfree2014
Sources:
ucdmc.ucdavis.edu/news/beating_heart.html
noblood.org/news-hot-topics-such-hepatitis-c-sars-aids/1258-heart-bypass-surgery-method-assessed-beating-heart-results-more-failed-grafts.html
sciencedaily.com/releases/2007/01/070131155322.htm
Sleep Requirements Following Coronary Bypass Surgery (CABG)

How much sleep should you get during recovery from coronary bypass surgery?
A healthy amount of sleep is so very important following CABG: coronary artery bypass grafting surgery.
“Most patients have difficulty returning to their normal sleep patterns for several weeks after surgery,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“It is easy to fall asleep, but difficult to stay asleep for more than three or four hours in a row.
“This is caused by many factors, including post-op discomfort, anxiety, and an overall feeling of fatigue, causing napping during the day and therefore fewer consecutive hours of sleep at night.”
My mother had quintuple bypass surgery, and she slept a lot (in the hospital as well as at home) following the CABG procedure.
Of course, a ton of sleeping will occur in the first few days following coronary bypass surgery, partially due to lingering effects of general anesthesia, plus side effects of painkillers.
Once the patient is in the cardiac wing for continuing recovery from bypass surgery, a lot of sleeping may continue to occur, if for no other reason that there’s not much to do in a hospital room between brief periods of walking therapy and attention from medical staff, unless you have a steady flow of visitors.
Dr. Fiocco continues, regarding once the CABG patient is home: “Also, many patients find it easier to sleep in a reclining chair compared to the bed (easier to get in and out), which may also limit sleep at night.
“These sleep issues are almost always self-limiting and resolve in several weeks without intervention. Occasionally a sleeping pill is necessary but only for a limited time.”
Dr. Fiocco also points out: “The trauma of major surgery combined with the emotional aspects of cardiac surgery lead to significant fatigue, which likely begins with loss of sleep before the surgery due to the anxiety leading up to the operation.”
In my mother’s case, there was little time for pre-surgery anxiety because she had only two hours’ notice of the bypass surgery!
And upon being told she needed emergent bypass surgery, she was already sedated from the preceding catheter angiogram procedure.
Dr. Fiocco says that the uncomfortable hospital bed doesn’t exactly encourage quality sleep, nor do the “interruptions for vital signs and blood draws, and sleeping in a strange environment.”
The CABG patient may be quite exhausted while in the hospital, but unable to sleep for significant chunks of time due to the various distractions (medical procedures, visits, even noisy floor cleaning machines in the corridor).
“Sleeping more than 10 hours/day may be a warning sign of depression, but it is more likely to be expressed in a lack of motivation to walk, read or get out of the house and begin normal activities,” says Dr. Fiocco.
The coronary bypass patient should listen to his or her body, follow cardiac rehab protocols (which will be supplied in booklet form) and keep in continuous contact with the post-surgery cardiac care team.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/gpointstudio
Can CABG (Heart Bypass Surgery) Disrupt Thyroid Function?
Can thyroid levels be affected by heart bypass surgery?
The thyroid controls metabolism. And metabolism is a lot more than how many calories per hour your body burns at rest.
“Metabolism is the process by which cells utilize oxygen for their performance in the human body,” says Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital, one of the nation’s top 50 heart hospitals.
Thus, it’s intuitive that coronary bypass surgery could somehow affect thyroid function in some patients.
“The simple answer is yes and likely in everyone, although only rarely is it of any clinical significance,” says Dr. Fiocco.
“Any patient in a stressful environment may have hypothyroidism based on laboratory measurements, but the majority resolve with the withdrawal of the stress (i.e., ICU, severe pain, cardiopulmonary bypass).”
Hypothyroidism means underactive, or low, thyroid: This gland isn’t producing sufficient amounts of the hormone thyroxine, which gives instructions to the body to carry out various functions.
Dr. Fiocco continues, “As far as the patient is concerned, they should be sure that their thyroid function is normal leading into the surgery, and then any small change due to the stress of surgery will not be a problem.”
A blood test that is given pre-surgery, as part of a workup to make sure that the patient can withstand the surgery, will reveal if thyroid levels are low.
Low thyroid is treated with a daily dose of bioidentical hormone replacement (to replace thyroxine).
When the dose is right, a blood test will show a TSH (thyroid stimulating hormone) numerical value that’s within a normal range.
A person with low thyroid may end up needing coronary bypass surgery (almost half a million CABG procedures are performed yearly in the U.S.), and pre-surgery, the patient’s TSH level may be normal.
However, post-surgery, even though the patient continues to take the oral dose of hormone replacement, the TSH level may not be normal; it may be off a little bit — enough to cause some symptoms that are typical of hypothyroidism.
“Yes, coronary bypass surgery can suppress the conversion of T4 to the active T3, making the thyroxine less effective,” says Kent Holtorf, MD, a thyroidologist and founder of Holtorf Medical Group.
T4 is another name for thyroxine, and T3 is triiodothyronine.
“The problem is that the TSH does not go up, but rather, down, so the tissue hypothyroidism is not detected by standard testing based on the TSH,” continues Dr. Holtorf.
“A TSH over 5 typically means that the thyroid is low, but with CABG, there are low thyroid levels with a normal TSH.”
“The significant physiologic stress associated with bypass will lower TSH production, which lowers T4, but more importantly, it reduces the T4 to T3 conversion inside the cell and increases reverse T3, which blocks the thyroid effect.
“Both these complications are extremely common and very treatable with supplemental T3, but it is rarely done because they are misdiagnosed as normal thyroid based on a normal TSH.”
So is a disruption in the so-called thyroid levels uncommon or common?
The best answer is to know the symptoms post-CABG that are suspicious for a thyroid issue.
Dr. Holtorf says, “The major symptoms of low thyroid levels post-CABG are heart failure and arrhythmias, such as atrial fibrillation, post-operatively.
If a patient has been pre-surgically receiving treatment for low thyroid, could coronary bypass surgery render their preexisting Synthroid or Levothyroxine insufficient?
Dr. Holtorf says, “Yes, it is especially a problem with those with preexisting thyroid dysfunction and on T4-only preparations.”
Symptoms of low thyroid include unexplained weight gain, feeling cold when nobody else does, unusual hair loss, fatigue and exercise intolerance.
However, hypothyroidism symptoms can also include: constipation, excessive sleepiness, elevated cholesterol, joint pain and stiffness, a puffy face, hoarse voice, muscle weakness, heavier than normal menstrual bleeding, depression, confusion, irrational thinking and memory problems.
If a person who, prior to coronary bypass surgery was normally upbeat and well-grounded, turns out to be uncharacteristically depressed, irrational and sluggish after surgery (taking into consideration the timeline for healing and emotional adjustment), the patient should have his or her TSH and T3 levels checked for possible low thyroid.

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: mayoclinic.com/health/hypothyroidism/DS00353/DSECTION=symptoms
Why Don’t More Heart Surgeons Do Off-Pump Bypass?

Why don’t more heart surgeons perform off-pump (beating heart) surgery?
Off-pump heart surgery carries less risk of stroke and other serious issues when compared to on-pump heart surgery (i.e., operations that use the heart-lung, or cardiopulmonary bypass, machine).
I wondered why, in this day and age, off-pump surgery isn’t the standard for heart surgeons; why is it still the exception.
Coronary artery bypass grafting surgery is known as CABG.
“I have performed 80 percent of my CABGs off-pump for the past nine years with a dramatic reduction in blood utilization, stroke and renal failure,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
With beating heart surgery, post-operative depression occurs less frequently.
Dr. Fiocco continues, “The medical literature has a mixture of articles saying off-pump is better, off-pump is the same as on-pump, and even some that say off-pump is worse.
“Bottom line, in the hands of skilled and experienced off-pump surgeons, the results are better.”
Why don’t more cardiothoracic surgeons do beating heart procedures?
“The reason that only 25-30 percent of cases nationwide are performed with the heart beating is because it is technically more demanding,” explains Dr. Fiocco.
“It also requires very skilled assistants and dedicated anesthesiologists.
“Most surgeons do not have the patience to work their way through the learning curve to become skilled enough to approach the majority of cases off-pump.
“It is a challenging technique, but I feel very strongly that off-pump surgery will become even more important to learn as the population ages more and more.”
Who benefits most from this kind of surgery?
“Elderly patients see the greatest benefit from off-pump surgery, while a patient less than 60 probably benefits very little,” says Dr. Fiocco.
Can you elaborate?
“Age is only important as it relates to the disease state of the patient. Most younger patients tend to be healthier, less likely to have kidney, lung or vascular disease.
“Elderly patients are more likely to have renal insufficiency, COPD, history of stroke, calcification of the aorta, etc.
“These are the patients who see a marked risk reduction with off-pump CABG.
“That being said, there are some 80-year-olds who are healthy and I have no problem doing on-pump, and some 50-year-olds who are sickly and worrisome.
“But, in general, the younger are healthier and will tolerate either method.”
What kind of patients would probably do better with the heart-lung machine method?
“Off-pump surgery requires manipulation of the heart to visualize all areas,” says Dr. Fiocco.
“This is remarkably well-tolerated in most, but some patients develop a drop in blood pressure or EKG changes severe enough that they must be placed on-pump.
“Patients with a large heart, thick heart muscle due to high blood pressure, and cases that are true emergencies are usually the ones which can’t be performed off-pump.”

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ igorstevanovic
What if Coronary Bypass Patient Keeps Eating Junk Food?

How long do the grafts from coronary bypass surgery last if the patient continues eating a junk food diet?
Is coronary bypass surgery a green light to continue eating a junk food diet, and how long will the surgical bypass grafts last if the patient won’t quit his junk food diet?
About half a million coronary bypass surgeries (aka CABG) are performed in the U.S. every year, and you can believe that out of this gigantic number, a substantial amount of patients continue with their junk food diet after the surgery.
“Many factors determine how long CABG grafts will last,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
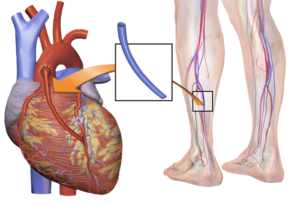
“The internal mammary artery graft (IMA) is superior to saphenous vein grafts (SVG), with a patency greater than 95 percent at five years and likely at 10 years.”
The saphenous vein comes from the leg. The patency for the SVG is 82 percent at five years, and 65 percent at 10 years, according to a small study. Dr. Fiocco says there are problems with these numbers.
“First, this is a sample of patients; not everyone returns to have their grafts looked at, which used to require cardiac catheterization, but now can be done with CT scan,” says Dr. Fiocco. The CT angiogram will reveal any dangerous narrowing of the arteries.
Dr. Fiocco continues, “Second, this sample includes those who lead a heart healthy lifestyle after surgery and those who didn’t, so the smokers and junk food eaters certainly bring these numbers down.
“Thirdly, a closed graft does not necessarily mean a failed surgery or the need for another operation.
“If you have CABG x 4 or 5, and one graft closes, chances are you are doing fine and won’t need any other intervention.”
There have been no extensive studies on just how damaging a junk food diet (or smoking) is on a revascularized heart.
But do we really need research to know that if a patient continues with a bad diet after coronary bypass surgery, he will shorten the life span of his bypass grafts?
The junky diet is what got him in trouble in the first place (along with any other heart-harmful variables such as smoking, lack of exercise and mismanagement of diabetes).
Dr. Fiocco explains, “Diet and exercise, along with smoking cessation, will improve the longevity of the grafts, but to put a number on it is difficult since the quality of the vein, quality of the artery being sewn to, and the technique are all important as well.
“I tell my patients that they will at least get 10-15 years out of bypass surgery if they follow a heart healthy lifestyle.”

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Coronary Bypass Surgery Cause Orthostatic Hypotension?
Can orthostatic hypotension be caused by coronary bypass surgery?
If you’re wondering if orthostatic hypotension can be caused by coronary bypass surgery, you’re not alone.
“Hypotension after surgery is a common problem and takes several different forms,” says Dr. Michael Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
“Orthostatic hypotension means the blood pressure drops when going from a sitting or lying position to a standing position. This may be accompanied by lightheadedness or dizziness.”
In some cases of orthostatic hypotension, the patient will start blacking out and even completely faint.
However, an all-out fainting episode can be arrested if the patient takes a seat.
The tricky thing is that sometimes, once a fainting spell begins unfolding, the patient will not be able to self-correct the situation, and thus will fall to the floor.
This can have devastating consequences if the head takes the brunt of the fall.
Dr. Fiocco continues, “The major causes are dehydration, over-medication (too much antihypertensive med) and a poorly understood third cause felt to be related to vascular tone and/or hormone levels (thyroid/cortisol).”
Immediately following coronary bypass surgery, a patient actually retains fluid, and is given diuretics to drain the fluid – unless the patient’s kidneys have been acutely damaged from the coronary bypass surgery (diuretics impose stress on the kidneys).
Longer-out from coronary bypass surgery, when there is no longer edema (fluid retention), and the kidneys have rebounded, the patient may still be experiencing orthostatic hypotension – from dehydration.
Lingering effects of the general anesthesia, and/or the heart-lung machine that was used during the coronary bypass surgery, could temporarily alter taste, making water consumption unpleasant.
Coronary bypass surgery. Shutterstock/Medical Communications, Inc.
“Obviously, medication adjustments can be made by eliminating certain meds or decreasing the dose,” says Dr. Fiocco.
For instance, Lopressor (used to help heart rhythm after coronary bypass surgery) can cause low blood pressure or dizziness.
Amiodarone, another drug commonly given after coronary bypass surgery, can cause low blood pressure.
Dr. Fiocco says that adjusting medications solves the overwhelming majority of orthostatic hypotension cases.
“The vascular tone/decreased hormone patients tend to be hypotensive, whether sitting or standing.
“These patients may require an IV medication to support their blood pressure while in the hospital until the vascular tone returns and/or the hormones are replaced. This may prolong the hospital stay to as long as 5-6 days.”
So just what is vascular tone?
Dr. Fiocco explains, “Everyone has a certain degree of vascular tone. Medications to treat high blood pressure are designed to decrease vascular tone or relax the blood vessel wall which consists of, among other things, smooth muscle.
“Relax the muscle, the vessel dilates and blood pressure comes down. Why this occurs after surgery, particularly coronary bypass, is unclear.
“Likely it is multifactorial involving general anesthesia, pain medication, exposure to various drugs in the OR and maybe most important, preoperative medications.
“Rarely, it can be caused by hypothyroidism or hypoadrenalism (lack of steroid production by the adrenal glands).”

Dr. Fiocco specializes in treating artery disease, valvular disease and aortic aneurysm. His heart care expertise has earned him recognition by Baltimore Magazine as a Top Doctor in 2010, 2011, 2013, 2016 and 2017.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Does the Heart-Lung Machine Affect Sense of Taste?

Does the heart lung machine (cardiopulmonary bypass) affect sense of taste?
The heart lung machine is used during cardiac surgery so that the surgeon can make repairs on a completely still heart (no pumping), but can the heart lung machine cause a change in taste perception of the patient?
Some controversy surrounds use of the heart lung machine (“on-pump” surgery), as it has been suspected as a cause of neurological problems in a small percentage of coronary bypass patients – problems that were non-existent before their operations.
It is not unheard of for a coronary bypass or other cardiac procedure patient, whose surgery included use of the heart lung machine, to post-op complain of taste problems.
“Change in taste is most commonly due to a disturbance in the sense of smell, known as the olfactory system,” says Michael Fiocco, MD, Chief of Open Heart Surgery at Union Memorial Hospital, one of the nation’s top 50 heart hospitals.
“The heart lung machine may play an indirect role in altering taste. Most commonly patients complain of a) metallic taste b) tastes bad and c) no taste.”
Food may taste like cardboard or be extremely bland, and water may have an unappealing taste.
Interestingly, certain foods may taste just fine post-op to the coronary bypass patient who reports a change in taste.
“The heart lung machine’s contribution to this is likely its propensity to cause edema or swelling,” continues Dr. Fiocco.
“This can occur throughout the entire body, including the brain, thus affecting the olfactory system (smell) which, as noted above, will alter the sense of taste.”
However, if you’ve recently had coronary bypass or other cardiac surgery, and were connected to a heart lung machine (cardiopulmonary bypass), and … if you’ve noticed a change in the way food or beverages taste … this alteration isn’t necessarily the result of the heart lung machine.
Dr. Fiocco explains, “Separate from the heart lung machine, but related to bypass surgery, is the change in taste associated with general anesthesia as well as the side affects of many medications.
“The majority of patients resolve their taste problems within a few weeks without treatment other than occasionally having to change or withdraw certain meds.”
In conclusion, if you have had coronary bypass surgery, and are having difficulty eating due to a change in taste, keep reminding yourself that the diminished or unpleasant taste sensation is temporary.
Also keep reminding yourself that following coronary bypass surgery, you need to eat like an athlete, because your body has been subjected to significant (though controlled) trauma, and is in desperate need of nutrients, particularly protein, for the healing process.