Can Pneumonia in the Elderly Be Only Mild ?

Is there a such thing as MILD pneumonia in an elderly person, and if so, is this any less of an urgent situation?
Ever wonder if it’s possible for an elderly person to experience a pneumonia that’s only mild?
“Of course it can, in folks who are generally healthy,” begins Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“But in the frail elderly, even a cold can cause significant issues.”
Though pneumonia in an advanced-age patient doesn’t always produce serious symptoms, this doesn’t mean one should be any less vigilant with recovery.
Pneumonia in the elderly can produce what appears to be mild symptoms, as was the case with my mother, who at the time was over age 70.
Initially she appeared to just have a nagging cough. It would come on suddenly and she’d have a spell of hacking.
I tried to get her to describe the nature of this cough, but her feedback was not reliable, as she’s not someone who’s very tuned into her body or symptoms.
My mother’s cough sounded really bad and was producing phlegm, and I began suspecting pneumonia, something coming up from her lungs.
Even though my mother kept saying she felt fine, other than feeling tired or weak “from all the coughing,” I couldn’t dismiss pneumonia as a real possible trigger of the coughing.
And when my mother said she felt “fine,” save for being de-energized from the physical exertion of all the coughing, I had to wonder if she was able to make the distinction between feeling tired from hacking and feeling tired from general fatigue due to infection.
There were no other symptoms; no fever, shakes, chills or shortness of breath – pre-diagnosis.
The diagnosis at the ER was “a little” pneumonia.
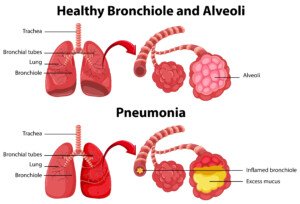
The next day, my elderly but very mobile mother reported feeling weak.
Throughout the course of her recovery from pneumonia, once it was diagnosed and she was taking an antibiotic and albuterol puffs from an inhaler, the symptoms other than the coughing were that of weakness/fatigue, at least a few incidents of shortness of breath and one incident of minor shaking.
Otherwise, my mother was functional, though I, who was staying with my parents throughout this, wouldn’t let her do any housework beyond simple kitchen work. She took it very easy and slept a lot.
The shortness of breath could have also come from the antibiotic, and the shaking, though a possible symptom of pneumonia, was clearly indicated as a possible side effect by the albuterol inhaler guidelines.
All in all, my elderly mother’s bout with pneumonia presented a mild picture as far as symptoms, and perhaps that was because treatment began early.
A stubborn cough in the elderly, whether that person is a “young” elderly or a frail elderly, should never be brushed off.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, bearfotos
What Besides Depression Causes Pain All Over the Body?

There are causes of pain throughout the body other than depression.
As you may already know, depression can cause pain all over your body, but other things too can have this effect.
“To tell if you are depressed, ask yourself the simple question: ‘Do I have many interests?’” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “From Fatigued to Fantastic!”
“If you have many interests but are frustrated because you don’t have the energy or you are in too much pain to do them, then you are likely not depressed,” continues Dr. Teitelbaum.
“In addition, people know if they are depressed. If you feel depressed, then you probably are.
“If not, then you’re not. This has actually been demonstrated in scientific research to be highly accurate.”
Have you been suffering with body-wide pain and have gone to one doctor after another seeking the cause and treatment, and instead have found yourself at a dead-end?
Or perhaps you’ve been told that it’s stress related or “all in your mind”?
First see if fibromyalgia, a pain disorder that can affect mood, can be ruled out.
Dr. Teitelbaum says there are specific exams and tests that, depending on the results, can strongly point to fibromyalgia as the primary problem.
One of these tests is called the tender point exam. Blood tests should be given that can rule out other conditions such as a thyroid problem.
Now, if fibromyalgia, thyroid problems and other “physical” conditions can definitely be ruled out as the cause of your symptoms, you may indeed be suffering from a primary depression.
Substance P
Dr. Teitelbaum continues, “Increasing serotonin [a neurotransmitter], such as with antidepressants, may decrease depression, but also decreases the level of a key pain transmitter molecule called substance P.
So interestingly, where antidepressants are only modestly effective in treating mild to moderate depression, they can be very effective for treating pain.”
My mother at one point complained of pain throughout her entire body.
She also had deep depression (which was caused or aggravated by hypothyroidism).
The pain disappeared the day after she went on Cymbalta, which has been marketed extensively as an antidepressant.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Stasique
4 Natural Ways to Lengthen Telomeres & Make Cells Younger
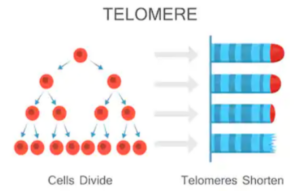
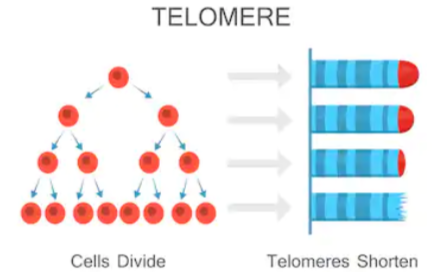
Longer telomeres mean a longer healthier life; you can actually lengthen the telomeres in your cells with any one of four natural ways.
This has been shown by research from UC San Francisco and the Preventive Medicine Research Institute scientists.
Dean Ornish, MD, says in the paper that the length of telomeres can fluctuate, including lengthen. Longer telomeres are associated with longer life and fewer diseases.
Telomeres are somehow linked to the aging process, to how rapidly or slowly cells divide and when they cease dividing.
These structures contain DNA and protein, and protect the ends of chromosomes. The shortening of telomeres is associated with the aging of cells.
Larger studies are called for, says the report, and this small study lays the groundwork.
“We believe that increases in telomere length may help to prevent these conditions [e.g., cancer, stroke, diabetes] and perhaps even lengthen lifespan,” says co-senior author Peter R. Carroll, MD, in the paper.
The full report appears in the online The Lancet Oncology (Sept. 16, 2013).
In summary, the four natural ways to lengthen telomeres are: 1) plant-based diet, 2) moderate exercise, 3) stress reduction, and 4) a support group that would apply to whatever challenges you’re facing.
What is moderate exercise?
The definition depends on whom you ask. As a former personal trainer, my best definition is that which is somewhat challenging and that gets you feeling worked — but not worked over.

Moderate exercise isn’t measured by duration, but by what kind of effort you’re putting into it.
What’s moderate to one person may be mild to another, and intense to yet another.
Thus. moderate exercise is also not measured by speed, revolutions per minute, pedal resistance, incline or amount of weight lifted.
To help lengthen your telomeres, you should do both aerobic and resistance workouts. If you can easily carry on a conversation by doing either, the effort level is in the mild range, rather than moderate.
Another way to gauge intensity is the rate of perceived exertion.
On a scale of 1 to 10, a subjective rating of 5 or 6 would fall within the moderate range.
Exercise will also help reduce stress, which will further benefit teleomere length.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Fancy Tapis
Source: sciencedaily.com/releases/2013/09/130916203946.htm
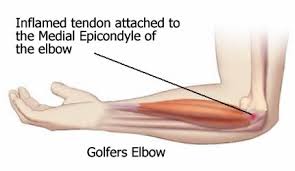
How Long Does It Take Golfer’s Elbow to Heal?
How long does it take to get rid of medial epichondylitis, also known as golfer’s elbow?
I developed a case of medial epichondylitis (golfer’s elbow) after doing high reps, low weights, with a close-grip on a cable pull-down (palms facing each other).
The discomfort initially wasn’t that great, and I actually continued working out full-force with rows and even doing chin-ups and neutral-grip pull-ups with full body weight.
Over the next few weeks the discomfort morphed into pain—not sharp pain but a strong dull pain, if that makes any sense.
I realized I had medial epichondylitis—couldn’t deny it any longer. It’s called golfer’s elbow because it happens a lot to golfers, but one need not be a golfer to get medial epichondylitis.
This is an inflammation of the tendon on the inside of the elbow. I went to an orthopedic doctor to see what she had to say, and she diagnosed it as medial epichondylitis.
She told me to avoid strength training exercises that aggravate it. She gave me a wrist brace to wear at night to prevent wrist movement, explaining that the problem is linked to wrist action.
She also said take an anti-inflammatory, ice the elbow, and over the next 3-4 months, it will heal.
A Mr. Olympia bodybuilding champion told me something a bit different.
At the time, I was editor of a fitness magazine that he contributed a column to, so that’s how I knew him.
He said to strengthen the wrists by doing wrists rolls, because this would strengthen the forearm muscles, which tie into elbow function: Strong wrists mean strong elbows.

Wrist roll with a dumbbell. Shutterstock/Philip Date
I wore the brace most nights (I’d sometimes forget); avoided offending activities; initially took an anti-inflammatory but stopped; and did the wrist rolls.
I also did what has proven to be very effective at healing my past tendon injuries (I’ve always lifted weights), and that is to (believe it or not) perform the offending activities but with a very light resistance—not enough to induce discomfort.
Chin-ups and neutral-grip pull-ups were out, but standard pull-ups were in, as these didn’t cause pain.
However, I did, with very light weight, close-grip pull-downs, plus biceps curls and rows. There was only slight improvement over the next 3-4 months.
I eventually stopped doing the wrist rolls, mainly because I kept forgetting to do them.
Then I injured my fingers rock-wall climbing (not acutely, but over a period of several climbing sessions, I strained them).
Unexpected Cure for Golfer’s Elbow
Treatment for this was a special way of using a hand grip device, which of course, strengthens the wrists and forearms. I did this over the next six weeks, healing the injury.

Hand grip device
How I Did the Hand Grip Exercise
- The tension should allow you to easily close the handles all the way.
- When opening or releasing the handles, take 8 to 10 seconds. No quicker. Count the seconds as you SLOWLY open.
- Close at normal speed.
- Slowly open again for 8-10 seconds, and repeat for 10 to 12 reps.
- Rest a few minutes; repeat for two more SETS.
- Do this daily.
Not long after, I became aware that the medial epichondylitis didn’t seem to be as bad. I just didn’t feel it as much, and slightly increased the weight on the offending activities.
There was no discomfort, but I could sense that if I were to go all-out on these activities, I’d feel the golfer’s elbow.
Over several weeks, I gradually increased resistance, and with each increase, did not feel the golfer’s elbow.
I’d perform the offending activities three times a week at the conclusion of weight workouts.
Eventually, the resistance was at a point where it began slightly taxing me (still no golfer’s elbow pain), and not long after, I dropped it down to twice a week, since the resistance was now heavy enough to qualify as a mild work set.
This improvement continues. The resistance is nowhere near what would be a true work set for me (I like to go heavy for an 8-12 rep max), but it’s heavy enough to induce a feeling of some work, albeit mild.
I expect to continue increasing this weight incrementally, so that eventually, I’m doing an 8-12 RM.
So how long have I had medial epichondylitis or golfer’s elbow? A year and a half.
That stinks. But I anticipate full recovery, finally, and look forward to blasting out those chin-ups.
Edit: I have fully recovered from golfer’s elbow and have no pain deadlifting very heavy weight or doing pull-ups/chin-ups.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/KDdesignphoto
Brain Aneurysm Risk & Women: Quit Smoking, Lower Blood Pressure

If a brain aneurysm scares the heck out of you, quit smoking and make sure your blood pressure is normal–especially if you’re a woman.
Did you know that when a brain aneurysm ruptures, the survival rate is only 40 to 50 percent?
A recent study shows a very strong link between developing, and dying from, a ruptured brain aneurysm, in women who smoke and have high blood pressure.
An aneurysm is an abnormally dilated blood vessel. When this vessel ruptures in the brain, a subarachnoid hemorrhage (bleeding) results.
The study reports that an aneurysm can be treated before it actually ruptures, but not all of these abnormal dilations ever do rupture.
Doctors just can’t tell which ones will and which ones won’t.
Stop Smoking. Get Your Blood Pressure Under Control

Freepik.com
The Finnish study was long-term and the details appear in PLOS ONE (Sept. 9, 2013).
Incidence of subarachnoid hemmorhage varied from eight in 100,000 to 171 in 100,000 inividuals.
The variance depended on risk factors. And the strongest risk factors are smoking, high blood pressure and female gender.
Women with high blood pressure who were smokers had a 20-times higher rate of a ruptured brain aneurysm than did non-hypertensive men who never smoked. So this risk especially affects women.
The study authors believe that in women who smoke and have high blood pressure, and have been diagnosed with a non-ruptured brain aneurysm, the abnormality should be treated.
And if such is found in a never-smoking man with low blood pressure, it may not need treatment.
The Finnish study is the largest on SAH risk factors, and it revealed three new risk factors: previous heart attack; history of a stroke in a person’s mother; and elevated cholesterol levels in males.
Conclusion
High blood pressure and smoking are very strong risk factors not only for death from ruptured brain aneurysm, but also for the actual development of one of these abnormal dilations.
The study authors recommend that women who smoke quit once and for all, and to work on lowering their blood pressure.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com,rawpixel
Source: sciencedaily.com/releases/2013/09/130909201245.htm
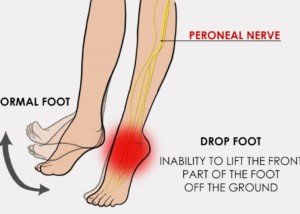
Foot Drop Evaluation: What Is the Best Medical Test?

There is a simple, painless and non-intimidating test to evaluate foot drop, which can have many causes.
If you’ve been experiencing foot drop and want a medical test to evaluate this symptom, there’s a particular procedure that you should ask your doctor about.
The procedure is a high resolution ultrasound — which did very well as a tool, according to a study.
What is foot drop?

Pagemaker787, CC BY-SA
Foot drop is when a person experiences inability or difficulty moving the ankle and the toes, and this problem causes the foot to slap about when walking, unable to clear the floor or ground.
Why the ultrasound test for foot drop?
The study was conducted at the Feinberg School of Medicine, Northwestern University in Chicago.
The nice thing about ultrasound is that it’s non-invasive.
The targeted body part is exposed to high-frequency ultrasound waves that create pictures of the patient’s insides.
When someone has foot drop, the typical tests done are EMG and MRI.
However, some people dread the idea of getting pricked by needles during an EMG, or being confined inside an MRI “tube” with its loud knocking sounds.
Tom Grant, DO, led the study of 15 patients with foot drop.
For these patients, the ultrasound was “highly effectdive” for characterizing the common peroneal nerve — which controls foot/ankle movement.
Ultrasound was able to detect that all of the patients had pathology of the peroneal nerve.
Though this was a very small study, it brings to light that in some patients, ultrasound for foot drop can be quite effective.
But it may also produce a normal result.
If the ultrasound results are normal, then the patient should undergo an EMG (electromyography) as well as an MRI (magnetic resonance imaging).
“I have a high-resolution ultrasound in my office and I use it frequently to diagnose a wide plethora of musculoskeletal problems,” says Dr. Velimir Petkov, DPM, surgeon and sports medicine specialist of the foot with Premier Podiatry in Clifton, NJ.
“That being said, as good as the newer high-resolution ultrasound units are, the gold standard is still MRI.
“If you are unsure about a certain soft tissue pathology, always order an MRI – it can literally show you things that no other imaging modality can.”
 Dr. Petkov diagnoses and treats numerous ailments related to the lower extremities, and has special interests in sports medicine, wound care and the most advanced minimally invasive procedures for plantar fasciitis and Achilles tendonitis.
Dr. Petkov diagnoses and treats numerous ailments related to the lower extremities, and has special interests in sports medicine, wound care and the most advanced minimally invasive procedures for plantar fasciitis and Achilles tendonitis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Skumer
Source: sciencedaily.com/releases/2010/05/100506083440.htm
Too Skinny? Can’t Gain Weight?
If no matter what you do you can’t put weight on your skinny body, here’s why, and what you can do to solve this problem.
Rigorous exercise is one sure way to increase appetite.
Raise the body’s energy demands, and it will seek out more energy than it normally uses.
If there’s not much fat (stored fuel) in the body, it will seek it out in food-and hence, appetite will get bigger.
But if food isn’t consumed by the skinny individual to meet a significant increase in physical output, then a catabolic effect will result. The body will feed off its own muscle tissue.
Eat high-glycemic foods.
Though white rice is not a preferred grain because it’s heavily processed, it really does wonders to induce hunger pangs.

Shutterstock/monticello
The best bet is organic white rice. Next in line, and healthier, is organic white basmati rice.
Rice is not cheap in calories, and a bowl, eaten with a meal, can cause annoying hunger within one to two hours of finishing the meal.
Though whole potatoes are medium-glycemic, they too, can cause a lot of hunger shortly after being eaten.
High-glycemic foods include: dates, watermelon, mashed potatoes, corn flakes, millet, white bread, rice pasta, puffed-rice snacks, rice cakes and graham crackers. Some people report that hunger becomes intense after eating carrots or onions.
Foods ridiculously high in calories.
All nuts, but this can be a two-edged sword in that a bowl of nuts may kill appetite for hours. Best time to eat nuts for weight gain, then, would be close to bedtime.
High-calorie foods that are sold in organic, all-natural versions: cheese, jams and jellies, nut-swirl breads, nut butters and peanut butter, flax and olive oil, salad dressing, dark and milk chocolate, some “energy” bars, many cereals (no sugar added), pancakes and waffles (opt for whole-grain varieties), corn, beans, muffins, potato salad, avocado salad, and whole-grain cookies containing chocolate chips and various nuts–just to name a few!
Stuffing mixes, when a canola spread is added (this substitutes for butter) are outrageously high in calories per indicated “serving size.” The whole box prepared can fit a giant cereal bowl: 1,000 calories.
Of course, animal products are usually high in calories, but err on the side of a plant-based diet.
You can still enjoy the cheese-omelet and preservative-free sausage/bacon, and the porterhouse steaks, but these kinds of foods should be eaten sparingly.
There are plenty of healthier ways to put on weight. Whole foods stores also sell weight-gainer shake mixes.
Weight gain is possible without loading up on the more classic high-calorie foods such as gravy, fried foods, fast-foods and pastries.

Shutterstock/Gts
One giant cinnamon roll, complete with icing, is around 800 calories. Something like this should not be eaten on a regular basis in the name of gaining weight.
Better to get 800 calories in the form of a shake made with weight-gainer’s protein powder, juice, strawberries and a banana, for example. Slurp it up with a straw and it’ll be gone in no time.
For people who have a sweet tooth, whole-foods stores do sell all-natural pastries, ice cream, cakes, brownies and other such items, and these are always better than the conventional versions that are full of preservatives, artificial flavor/color, and other strange ingredients.
But it’s still wrong to load up on these kinds of foods, even in the organic or additive-free versions. Muscles need complex carbohydrates and healthy sources of protein to grow.
Eat six or seven meals a day.
Ironically, this is recommended for weight loss, but the “meals” are supposed to be small in that case. But some thin people do only eat a few times a day.
Eating more meals (or more frequently) eliminates having to stuff one’s self at a single sitting to get in more calories.
How to Add Calories Without Feeling Stuffed
– Add the following items to vegetable salads that already have high-calorie natural dressings: sunflower seeds or nuts, shreds of cheddar cheese, and croutons.
– Add a tablespoon of flax oil to most frozen dinner dishes, pasta dishes, casseroles, or any other meal that would taste better with nutty flavor added to it. Some people consume flax oil straight off the tablespoon.
– Add organic chocolate syrup to organic milk.
– Add canola spreads, jams, jellies, apple and nut butters to bread.
– Try peanut butter on an apple or banana.
Reasons People Fail to Gain Mass
• Too many simple carbs, not enough high-quality protein.
• Weight workouts not intense enough to trigger new muscle growth.
• Inconsistency, missing workouts.
• Overtraining. If muscles aren’t allowed to recover, they won’t grow.
• Not doing the very routines (multi-joint) that can really accelerate muscle growth, such as barbell squats, leg presses, deadlifts, bench presses, dumbbell rows and other dumbbell routines.
But these must be performed with heavy enough weight to bring on severe fatigue in 5-8 reps.
• Not doing enough free-weight routines; too much focus on selectorized equipment.
Free-weight routines force stabilizer and synergistic muscles into action; the more muscles worked per routine, the more likely new mass will result.
• Not doing cardio. Three times a week for 30-45 minutes will do the trick, and don’t go through the motions. Get the heart pumping good.
• Doing cardio on the same days as weight-training. Doing cardio before weights will strip the body of energy needed to perform muscle-blitzing routines. Doing cardio afterweights will interfere with muscle recovery.
It’s okay to do brief, light cardio as a warm-up and cool-down, but save the actual cardio sessions for their own days.
• Not getting enough sleep (7-8 hours).
• High alcohol intake.
• Not drinking enough water.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Why You Should Never Ignore a Transient Ischemic Attack!

A TIA should never be ignored; this can lead to your death, even if the mini stroke lasts only seconds.
A transient ischemic attack (TIA) is also commonly called a mini stroke, but don’t let the terminology of “mini” trick you into thinking that a TIA is nothing to get overly concerned about.
If TIAs were called something like “stroke forerunners,” maybe they’d be taken more seriously by the general population.
Have you ever downplayed the seriousness of a transient ischemic attack because it’s usually called a mini-stroke or TIA? Don’t get snarled in this deceptive web.
“A TIA is a focal CNS disturbance caused by vascular events such as a micro-embolism or occlusion [blockage] leading to ischemia [deprived oxygen supply],” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
“They last less than 24 hours, and there is a full recovery.
“Speaking generally, if someone has a TIA it increases their stroke risk x 7 compared to the normal population.
“It shows that they have this increased tendency to form clots of platelet aggregates.
“Five to 10 percent of these arise from the heart. Other medical problems are risk factors for both TIA and stroke.” These include diabetes and high blood pressure.
“If someone has had a TIA there’s a fair chance that one of these other factors is playing a part — and a 30 second TIA needs to be referred and investigated as quickly as a 10 minute TIA.”
Serious Disability from Ignoring a TIA
A study on TIAs says that serious disability can be the outcome. The report is in the journal Stroke and also adds that often, doctors don’t take mini strokes very seriously.
The paper points out that in some cases, a doctor may not give a patient a clot busting drug because the transient ischemic attack was mild.
However, a TIA or mini stroke is a significant risk factor for future disability and needs early assessment and treatment.
Don’tn let “only a few moments” of blurred vision or feeling heavy on one side trick you into thinking “it’s nothing.”
Those who’ve had a TIA should be imaged early on, and treatment should be aggressive, says the paper.
It doesn’t matter how minor the symptoms are in a mini stroke, because if imaging detects a blockage, that is serious business. A treatment called thrombolysis can dissolve blockages.
The Study
Nearly 500 patients who had a TIA took part in the study, and 90 days after experiencing their mini stroke, 15 percent had at least one mild disability.
CAT scans showed narrowed blood vessels in the brains of some patients. Other subjects reported continued or worsening of symptoms.
Amazingly, it wasn’t until 2009 that the American Heart Association and American Stroke Association recommended swift action and complete testing for a transient ischemic attack — exams that can detect a blockage in brain blood vessels.
These blockages are potential gateways to a catastrophic event.
So never mind if mini stroke symptoms pass quickly, because if you have them, this means get to the ER stat to receive the proper scans.
The study warns that ignoring a transient ischemi attack can lead to death, because not getting treatment means a massive stroke may be lurking just around the corner.
A TIA is never benign. Never.
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/JL-Pfeifer
sscpywrt26
Source: sciencedaily.com/releases/2012/09/120913162437.htm
Reduce Stroke Risk After a TIA with Cardiac Rehab

Cardiac rehab will help you reduce your risk of stroke after having a transient ischemic attack.
If you’ve been diagnosed with a transient ischemic attack (TIA), then you know this is a mini stroke which means you’re at significant risk for suffering a major stroke in the near future — unless you take measures to prevent this.
A TIA results when a blood clot in the brain chokes off oxygen to the area that the blood vessel, where the clot is, feeds.
The clot usually dissolves within minutes, so the symptoms are transient or temporary.
A report in Stroke: Journal of the American Heart Association has something to say about transient ischemic attacks.
The senior researcher, Neville Suskin, notes that cardiac rehab addresses the risk factors for a stroke.
The Suskin study was small and looked into mild stroke and TIA rather than major stroke.
Nevertheless, if you suffer a TIA or mild stroke, these are still harbingers of a major stroke in the near future.
For the study, the participatns — all whom had a TIA or mild stroke the prior year — did cardio rehab for over seven months and then were re-evaluated for risk factors.
What was the cardiac rehab?
It involved exercise, nutrition education, medication management, smoking cessation and stress reduction.
Eighty people completed the cardiac rehab. The report says that “overall,” the subjects improved quite a bit in their risk profile.
This includes peak exercise capacity. Other improvements included blood lipids, waist circumference, body mass index and blood pressure.
Eleven additional patients were recategorized to lowest death risk after initially being at moderate or high risk of dying during the following year.
Self-Cardiac Rehab
If you’re afraid of getting a transient ischemic attack or have already had one, do the same things that you’d do to prevent a heart attack.
“There are two main types of risk factors in getting stroke [or TIA] which are modifiable and non-modifiable,” says Sashini Seeni, MD, a family medicine practitioner with DoctorOnCall, an online doctor and pharmacy.
“By knowing your risk factors, you might be able to manage them accordingly to lower your chance of getting stroke.
“Routine blood pressure measurement. The higher the blood pressure, the higher the chances of getting stroke. Check your BP routinely.”
According to the American College of Cardiology and the American Heart Association, it should be under 130/80. Otherwise, consult with your physician.
“Stop smoking,” says Dr. Seeni. “It is one of the major risk factors.
“Get a healthy balanced diet. Lower your cholesterol intake, get more fiber, fruits and veggies in your menu.” Lentils and beans are particularly high in fiber.
Finally, Dr. Seeni urges people to exercise. Housework and walking Fluffy around the block don’t count.
Sign up for group fitness classes or work out at home to videos. Join a gym. Take up yoga or martial arts. Go on hikes. Buy a pair of dumbbells. The list is endless.
 DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Brian A Jackson
sscpywrt26
Sources:
sciencedaily.com/releases/2011/09/110922164200.htm
stroke/article_em.htm#transient_ischemic_attack_tia_overview
Unsuspecting Stroke Risk: Getting Hit in the Head

There’s yet one more reason why you should try not to get hit hard in the head: It may increase your risk of a stroke.
The stroke at issue here is the ischemic type, in which a blood clot in the brain blocks blood from reaching the area that the vessel supplies.
People with traumatic brain injury (TBI), or, to put it more simplistically, a severe hit in the head, are more likely to suffer an ischemic stroke, says a paper in the June 26, 2013 online Neurology.
But there’s a reason you should not let this study scare you into thinking that the clobber in the head by a baseball you suffered in high school will give you a stroke later on.
“While this paper makes some interesting associations between TBI and ischemic stroke, the level of evidence for this study is level 4 out of 5,” says D’Wan Carpenter, DO, a board certified physical medicine and rehabilitation physician with SIMEDHealth in FLA.
The report goes as far as stating that the association between TBI and stroke is just as significant as is the link between high blood pressure and stroke.
Though stroke has some very identifiable risk factors, including smoking, diabetes and obesity, its risk factors remain perplexing to doctors, especially when the victim is under age 65.
How was this study done?
Two groups of patients were investigated: 1) adults who went to the ER or were admitted to a hospital for traumatic brain injury, and 2) those with other trauma but no TBI. Over 1.1 million patients were followed.
Results
1.1 percent of patients with TBI had a stroke over an average of 28 months after their TBIs, and 0.9 percent of patients with trauma but no TBI had a stroke.
Patients who had a TBI were 30 percent more likely to suffer from an ischemic stroke than subjects who had some kind of trauma but NO injury to the brain.
But this study, as interesting as it is, had limitations.
“It raises questions about this connection, given that individuals with TBI tend to be younger and take more risks, which may place them at risk for stroke due to lifestyle factors,” says Dr. Carpenter.
“I believe this study is one that should spark future studies to obtain higher levels of evidence in an effort to decrease another stroke risk factor if it indeed exists.”