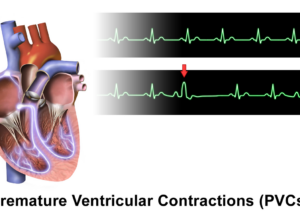
3 PVCs in a Row, but Structurally Normal Heart?

Can a run of three PVCs in someone with a structurally normal heart ever mean something concerning?
PVC stands for premature ventricular contraction, and some people experience or “feel” three in a row, as in thump … THUMP, thump … THUMP, thump … THUMP.
A run of three PVCs in a row leaves many people quite worried, even if their echocardiogram reveals a structurally normal heart.
“The more PVCs in a row, the more likely they are pathologic,” says cardiologist Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
“Three or more PVCs in a row are defined as non-sustained ventricular tachycardia, and an evaluation for underlying disease is mandatory when they occur,” explains Dr. Lepor.
What if the echocardiograph shows a structurally normal heart?
“If the heart is structurally normal you need to also evaluate for metabolic abnormalities such as electrolyte disorders (calcium, magnesium, potassium) and electrical abnormalities on ECG such as long QT syndrome.”
Don’t sit around in fear all day; make an appointment with a cardiologist and get some tests done.
Some recommended tests would be any of the following:
* EKG
* Echocardiogram
* Exercise stress test
* Cardiac MRI
* Blood tests (electrolytes, thyroid function)
* Electrophysiology study

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/8photo
Can Stress Cause an Extra Heartbeat?

This is about stress causing an extra heartbeat or the sensation of one, rather than the feeling of a skipped heartbeat.
“Studies have shown that stress can cause a sensation of a skipped or extra heartbeat that can be associated with either an extra heartbeat or no abnormality of heartbeat,” explains cardiologist Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
Dr. Lepor says that “this is related to the stress causing a release of adrenaline.”
Adrenaline is a hormone (chemical messenger) that’s released when we experience anxiety, trepidation or fear—and the fear need not be monumental—it can be simply that of opening an envelop that contains a bill that you know will be big.
Adrenaline is the “fight or flee” hormone that helps prepare the body for action.
Other hormones are also kicked into gear. A fight or flight produces anabolic hormones that neutralize the stress hormones, bringing the body back into balance.
If the fight or flight doesn’t come (i.e., you’re trapped at your workplace desk all day long in a stressful environment), the body will then be in a persistent state of fight or flight preparation…which is harmful to the body.
Dr. Lepor continues, “The sensation of an extra heartbeat is not always associated with an actual extra beat.
“The only way to distinguish is to wear a Holter monitor that records the heartbeat and symptoms you may have over a 24 hour period.”
This small device is worn on the body. After you’re done wearing it you turn it in to the medical clinic where its recording of your pulse will be printed out and interpreted.
If you seem to be experiencing an extra heartbeat when you’re under a lot of stress, ask your doctor about a Holter monitor.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Frank11
The Cause of a Heartbeat in Your Ear

You are not imagining hearing or feeling a heartbeat in your ear, as this is real and has a definite cause.
The phenomenon of having a heartbeat in your ear even has a name!
“At some times, especially when one lies on the side with an ear on the pillow, you can hear the heartbeat in your ear,” says cardiologist Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
“This is called pulsatile tinnitus. It occurs in patients who have conductive hearing loss that leads to increased sensitivity to internal head sounds such as blood flow to the ear, chewing.”
Dr. Lepor continues, “Patients with high blood pressure surges and blockages in the main arteries to the brain (carotid artery) can also have pulsatile tinnitus.
“If one senses a ‘swooshing sound’ in one’s ear, that can be related to an abnormality of the blood vessels in the brain called A-V malformation that can only be diagnosed with imaging studies such as CT, MR or angiography.”
If you’re experiencing a heartbeat in your ear, however, don’t jump to the conclusion that you necessarily have hearing loss, carotid artery disease or an A-V malformation.
Remember, the arteries are like pipes that run throughout a house, in that when water is gushing out of a particular pipe, you can hear this if you press your ear to a wall in another part of the house — pipes, or arteries, can conduct sound.
The arteries near your ear are very close to your heart, so it shouldn’t be surprising if you pick up a little heartbeat in certain positions in bed.
Nevertheless, it certainly won’t hurt to report this to a cardiologist and get an exam to rule out a less-than-benign cause — especially if you also hear it when not in bed or lying down.
In fact, many people have hearing loss and don’t realize it, since hearing loss develops insidiously and is painless.
The most common symptom of hearing loss is that of asking someone to repeat what they just said — the listener simply thinks the speaker didn’t talk clearly or loud enough.
If a heartbeat in your ear has you worried, discuss this with a cardiologist.
More Causes of a “Heartbeat in the Ear”
• Anemia
• Arterial stenosis
• Atherosclerosis
• Conductive hearing loss
• Ear abnormalities/Eustacian tube dysfunction
• Glomus benign tumor
• Hyperthyroidism
• Sigmoid or jugular sinus diverticulum
• Sinus wall abnormalities
• Spasms of the muscles within the ear
• Venous hum
If you have pulsatile tinnitus, you absolutely need to see your physician; it can mean something potentially life threatening.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/michaelheim
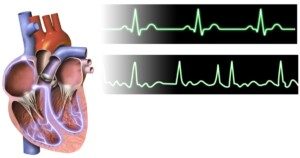
Can a 24 Hour Holter Monitor Miss Atrial Fibrillation?
Since atrial fibrillation isn’t guaranteed to occur in any given 24-hour period, isn’t it logical to conclude that a Holder monitor could miss it?
What exactly is atrial fibrillation?
Atrial fibrillation (AFib) is a heart rhythm disorder characterized by rapid and irregular electrical activity in the atria, the heart’s upper chambers.
This irregularity leads to an erratic heartbeat, which can cause symptoms like palpitations, fatigue and shortness of breath.
AFib increases the risk of stroke and heart failure if untreated.
If you were to view the number on a heart rate screen of a person with this heart arrhythmia, you would not see a steady number.
A normal heartbeat would show a steady number, give or take a few, such as a consistent range of 78 to 81.
If someone is in the midst of atrial fibrillation, you’d be seeing the numbers jumping all over the place quite quickly.
One moment the range might be high 70’s. Next moment it’s jumping around between 140 and 170.
Then suddenly it’s between 100 and 120. Then suddenly it’s 85, then 150. You get the picture.
A-fib. BruceBlaus
If a doctor or you yourself suspect atrial fibrillation, and the next step is to wear a Holter monitor, you may then think that this won’t necessarily be an effective way of tracking the heart rhythm disorder — since the atrial fibrillation may be quiet during the time you have on the Holter device.
“Atrial fibrillation can occur at varying frequency and is often not associated with symptoms,” says Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
“If it occurs less often than every 24 hours it can be missed on a Holter monitor,” he adds.
“Longer-term monitoring devices that can be monitoring for weeks to years can be used in those cases.”
So if the Holter device shows no abnormalities…this in no way means you don’t have A-fib.
Your doctor will tell you that you need to wear an event monitor that tracks heart rhythm for a longer period of time.
This device records your heart’s electrical activity continuously or at specific intervals to help diagnose irregularities or abnormal rhythms that may not be picked up by a Holter monitor.
Untreated atrial fibrillation is a major risk factor for an ischemic stroke.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
The Truth About GAS Causing Heart Palpitations

A cardiologist, not an online thread layperson, answers the question, “Can gas cause heart palpitations?”
Is there a true connection between farting and a flip-flopping heart?
“There is no clear cause and effect relationship between gas and palpitations. As common events, they can occur together,” says Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
So then, palpitations of the heart cannot possibly ever be caused by gas?
Dr. Lepor responds, “Only if one feels very embarrassed by the release of gas in public.”
The beating of the heart is driven by electrical signals. If you fart, there is no way that this will disrupt those electrical commands. Not directly, anyways.
Passing gas involves the digestive tract. Heart palpitations involve the cardiovascular system.
Though some bodily systems work closely together, such as the musculoskeletal and the nervous system, this is not the case with the digestive and the cardiovascular system.
So if you find that your heart skips a beat or jumps somewhat right after you pass gas … then consider the possibility that it’s embarrassment.
And try not to let one out when you’re around other people, especially inside a car or an elevator.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Master1305
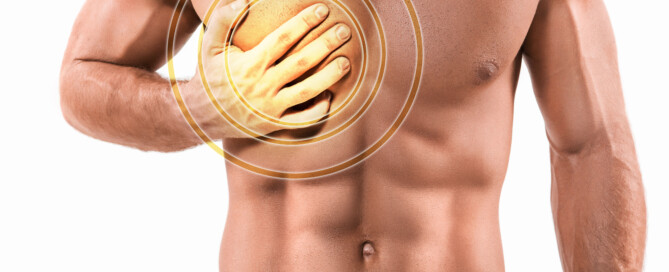
PVCs After Exercise: Forerunner of Heart Attack?
Have you been having PVCs right after you stop exercising, as in, you’ve been running on a treadmill or doing the burpees or pushups, and within seconds of ceasing the activity…you feel the premature ventricular contractions?
Does this mean you’re in trouble, as in, a future heart attack is awaiting?
“Post-exercise PVCs can be considered a risk factor for cardiac events if they are associated with underlying cardiac pathology,” says Norman E. Lepor, MD,cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
There’s a few things to consider here before you start panicking. Dr. Lepor mentions “cardiac pathology.”
If you just sprinted 14 mph for 30 seconds on the treadmill…chances are, you do not have cardiac pathology.
Nobody can just run like this. It requires training to get to this ability, even though it’s not exactly collegiate track team skill.
But a person with a pathologically compromised heart will not be able to sustain the training that’s required to reach this level.
Try it sometime: A young adult just starting an exercise program will be tossed off a treadmill or forced to step off if they attempt to run it, WITHOUT holding on, at 14 mph.
Another issue to consider, if you’ve been having PVCs post-exercise, is the anxiety factor.
You just rapidly squatted deep for 20 repetitions while holding a 40 pound medicine ball. You now feel the PVCs as you take a seat to catch your breath.
Chances are not high that there’s heart pathology involved, simply because this level of exercise—though not Olympic caliber—requires a trained body.
Many people off the street can’t even pick up a 40 pound ball, much less squat 20 times in a row with it.
Do you feel anxiety after finishing a set or ceasing an aerobic-based burst?
The anxiety may be from worrying about your exercise performance.
It may be from concern that an injury still hurts—did the set just make the injury worse?
And maybe you’re worried about PVCs in general and heart attacks, and after completing your intense exercise set, you started thinking about PVCs…and voila…you felt a few!
The adrenaline is going like mad, spurred by the exercise, and then spurred even more once you come to a rest and begin worrying about PVCs.
The conditions, then, are ripe for PVCs, since these can be triggered by adrenaline from anxiety over having a heart attack.
If you notice that PVCs regularly come right after exercise in the absence of anxiety, this increases the odds that there’s cardiac pathology.
Dr. Lepor says, “People with PVCs associated with activity should undergo a routine cardiac exam including a stress test and echocardiogram.”

Heart attack symptoms
If you fear a heart attack, don’t put off making the doctor appointment.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: MikeSaran
What Bleeding in Between Periods & Missed Periods Might Mean
Bleeding or spotting in between periods CAN mean cancer but also many other benign causes, and missed menstruation has a ton of causes.
Have you ever spotted in between periods? Seen blood stains on your underwear or on the tissue paper after you wiped yourself?
What’s the first thing that came to your mind?
Or, if this has not happened to you, what do you THINK would be the first thought that occurred to you? “Could I have cancer?”
Well, the truth is, bleeding in between doesn’t always mean cancer. On the other hand, it’s a very common symptom of uterine (endometrial) cancer.
It can be a sign of ovarian cancer, but only rarely.
Another cause, believe it or not, can be sitting on a hard bicycle seat and pedaling furiously — with no cycling exercise history, or after a long absence from cycling.
The jarring and pressure against a hard seat can cause mild spotting, but this does not come from the genital area; it’s likely from microscopic tears in the anal area.
This actually happened to me after pedaling furiously on a stationary bike—so hard, in fact, that when I was done, the bike had moved across the floor.
Another cause is doing rigorous jumping drills — again, with no jumping history, or after a long absence from jumping routines.
This has happened to me. But the spotting in these cases is either immediately after the exercise, or a little later on, and does not persist; it’s usually a one-time occurrence shortly after the activity.
If you haven’t done these activities and are bleeding (or spotting) in between periods, take this cue seriously, especially if you are postmenopausal.
It can mean cancer, though it can also have many other, less serious causes (which is actually usually the case).
Postmenopausal vaginal bleeding is a symptom of cancer in about 30 percent of cases.
About 90 percent of women with uterine cancer experience vaginal spotting or bleeding in between periods, or after menopause, according to the American Cancer Society.
Vaginal bleeding is often the first clue that something is wrong.
Other symptoms may not show until the disease is advanced.
Other symptoms of uterine cancer: prolonged periods; a pink, watery or white vaginal discharge (note: a milky-white discharge is also normal; this is known as “between-period discharge”).
It’s best to frequently monitor yourself so that you become familiar with what is normal and routine for your body, and what suddenly becomes different.
This could include pain during intercourse; a pelvic mass; pelvic pain; and unexplained weight loss (these usually occur in later disease stages).
Known Risk Factors for Uterine Cancer
• Diabetes
• Advanced age
• Longer menstrual span (i.e., time span from menstrual onset in adolescence to menopause)
• Never having been pregnant
• Obesity
• Higher lifetime-exposure to estrogen
• Pelvic radiation therapy
• Family history
• Breast/ovarian/colorectal cancer personal history.
Bleeding in Between Periods: Summary
The patient’s age factors into most probably causes, says Justin Chura, MD, a gynecological oncologist in Philadelphia, PA.
“For example, in a 20-year-old woman on birth control pills, bleeding between periods is very common, and the risk of cancer is extremely low.
“On the other hand, for a woman in her early 50s who still has menstrual periods and is now experiencing bleeding in between periods, further evaluation is needed including an ultrasound and possibly a biopsy.”
By the way, eating beets or juiced beets can cause urine to have a reddish tinge (from the beets’ red pigment), and this might pass for “bleeding in between periods.”
Missed period but not pregnant or menopausal?
Relax, it’s not a sign of cancer. Other causes of a missed period include:
– Severe dieting/substantial weight loss in short period of time
– Excessive, rigorous exercise, particularly related to endurance training
– Unusual amounts of stress
– Fast weight gain, or obesity
– Bulimia (vomiting food to lose weight)
– Birth control pills
– Depo-Provera injections
– Hormone imbalance
– Polycystic ovarian disease (hormone imbalance interferes with normal ovulation)
– Breast feeding
– Travel
– Illegal drug use
– No known cause – missed periods (in absence of pregnancy) are not that uncommon, and may actually mean nothing is up at all.
Nevertheless, it would be wise to see a gynecologist if you have missed two periods in a row, or two periods in 12 months.
 Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/siam.pukkato
Can Your Bad Cramps Be from Cervical Cancer?

Many disorders can cause bad cramps in the lower abdomen or pelvic area, but what are the odds that your recent-onset cramping is being caused by cervical cancer?
Yes, cervical cancer can cause bad cramping, but where does this disease rank as far as likelihood that it’s causing your discomfort as opposed to a benign cause?
Cervical cancer can cause pelvic or lower abdominal cramping.
“Cervical cancer can cause cramping in the pelvis,” says Justin Chura, MD, a gynecological oncologist in Philadelphia, PA.
“This can occur as the tumor expands on the cervix and pushes on the bladder and the bowel.”
Advanced Cervical Cancer
“Advanced cervical cancer can cause bleeding and increase the risk of infection, which can, in turn, cause cramping,” says Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, who’s board certified in ob/gyn and integrative medicine, is the author of “The Answer to Cancer.”
Cramping, however, is a common symptom and it is not specific to cervical cancer.
In fact, a sensation of cramping in the abdominal or pelvic region is one of the most common symptoms that doctors see patients about.
Causes are far-ranging and include strained muscles and irritable bowel syndrome.
“In other words, there are many more causes of cramping that are not cancer related,” says Dr. Chura.
“This can include cramping from fibroids, endometriosis, infections and painful menstrual cycles.”
Inflammatory bowel disease is another possible cause, though the pelvic cramping will likely be accompanied by aches elsewhere in the body due to the “enteropathic arthropathy” of inflammatory bowel disease.
Have a Pap smear if you’re worried about cervical cancer. This disease is SO easy to detect in its earliest stages.
The Pap smear can also detect precancerous changes in the cervix.
 Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/siam.pukkato
Can Chronic Cervicitis Lead to Cancer?
Cervicitis is inflammation of the cervix, but can this turn into cancer?
This is a question that many women would like to know, so I posed it to Justin Chura, MD, a gynecological oncologist in Philadelphia, PA.
“Chronic cervicitis does not lead to cervical cancer,” says Dr. Chura. “Cervicitis means inflammation. Inflammation can have multiple causes. This can include infection.
“The cause of cervical cancer is the human papilloma virus. Most of the time, chronic cervicitis is asymptomatic.
“Meaning, findings are seen on a Pap test, but the patient has no symptoms. When this is the case there is no recommended intervention.”
Perhaps the fear that cervicitis can lead to cancer or raise the risk of it originates from the fact that it can be discovered with a Pap smear — some patients wrongly connect dots and draw erroneous conclusions.
The risk of cervical cancer goes UP when a woman has multiple sex partners!
A sexually active woman should have a Pap smear annually, though this is also usually recommended for all women.
Frequency of the screening Pap smear should be discussed with one’s OBGYN.
 Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Does Cervical Dysplasia Always Turn into Cancer?

“Just because a woman is diagnosed with cervical dysplasia does not mean that she will develop cervical cancer,” says Justin Chura, MD, a gynecological oncologist in Philadelphia, PA.
A Pap smear will detect cervical dysplasia, which means atypical cell growth that’s non-malignant.
Dr. Chura explains, “For women with mild cervical dysplasia, no treatment is recommended, as this process resolves on its own most of the time.
“In addition, mild cervical dysplasia does not lead to cervical cancer. Severe cervical dysplasia, however, can lead to cervical cancer if not treated.
“Fortunately, treatments such as a cone biopsy are very effective in preventing this process from turning into cervical cancer.
“For some women with severe dysplasia, hysterectomy may also be an appropriate treatment option. The progression from severe dysplasia to cancer takes several years to occur.”
Luck of the Draw: Who Will and Won’t Develop Cervical Cancer
Dr. Chura explains, “The problem is that we do not know for which patient it will turn into cancer and for which patient it will not.
“One risk factor that a woman can control in potentially decreasing the risk of dysplasia progressing the cancer is exposure to tobacco.
“In other words, smoking should be avoided in women within all women, but especially in women with cervical dysplasia or cervical cancer.” Quit smoking!
 Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
Dr. Chura provides standard cancer care and robotic surgery for cancers of the cervix, ovary, uterus/endometrium and vulva. He is affiliated with multiple hospitals including Jefferson Einstein Philadelphia Hospital-Jefferson Health and City of Hope Cancer Center Atlanta, and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.