Top 5 Natural Treatments for Your Constipation

Actually, the No. 1 doctor-recommended treatment for constipation is so effective that it counts as ALL of the top five.
Constipation stinks (no pun intended). It hurts and in some cases can feel as though a brick is stuck halfway in and halfway out of your anus.
It may also require a trip to the ER so that a doctor or physician’s assistant can — with their fingers — try to pull out as much of the impacted fecal material as possible.
Usually an enema (inserted into the anus) is given to assist with the removal.
It takes about 15 minutes to begin working, and the result is a lot of liquid smelly diarrhea that seems to keep coming and coming.
But even if your constipation doesn’t get this bad, it’s still a pain to have.
You Don’t Have to Suffer from Constipation: Natural Treatment
“The top five natural treatments for constipation should ALL be powder fiber,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“Fiber is the only natural product that is not a laxative, because even naturally-occurring laxatives are laxatives and will eventually stop working when a person gets older.
“Laxatives also tend to draw fluid into your bowels from your body in an unnatural way.
“Fiber draws fluid into the bowel in a natural way and keeps water in the gastrointestinal tract that needs to be there.”
The water is what prevents stools from becoming too hard to comfortably push out, requiring straining.
Dr. Binderow also explains, “Another solution to constipation is to drink lots of water and fluids, so combining that with a natural powder fiber supplement should help regulate your system.
“The fiber will cause a bit of gas when you first start taking it, but that will stop within the first month or so.”
Finally, to help prevent constipation, don’t be sedentary.
Get lots of movement throughout the day. Don’t sit excessively.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Black Specks in Stools: Doctor Says Don’t Worry

“Usually a black speck in your stool is related to what you are eating – for example, coffee or pepper,” says Sander R. Binderow, MD.
Will bleeding or blood cause black specks in stools?
“A drop of blood in the stool will not present as a black speck – more so [it will] just cause an overall black stool or red depending on where in the intestines or colon the blood is absorbed,” explains Dr. Binderow, who’s with Atlanta Colon & Rectal Surgery.
If you’re worried about black specks in your BMs, you should realize that what you’re seeing may not even be black specks in the first place.
First of all, just how close are you inspecting your BMs?
What you’re seeing may be tiny pieces of a dark green food that got passed through, such as spinach.
When food particles do not fully break down in the digestive tract, they may pass through the intestines relatively intact, and their appearance can become noticeable in your stool.
This can particularly be true for foods with strong colors or those that are rich in pigments, such as blueberries, blackberries or certain types of vegetables – like spinach.
So remember: Undigested particles of food, when mixed with your poops, can appear as very dark or even black specks.
You should be able to prove this by taking some of the fecal matter, placing it on a white paper plate and then viewing it under a magnifying glass, in good lighting.
Between the magnification and the lighting, you should be able to see the true color of the “black specks,” e.g., very dark green, very dark purple.
Dr. Binderow adds, “Specks or spots in the stool do not need to be a cause for concern.”
Colon Cancer
And they certainly do not indicate the possibility of colon cancer, either.
Every patient should get a screening colonoscopy beginning at age 45, and even earlier if they’re at higher-than-average risk.
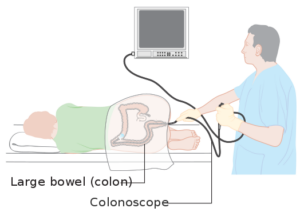
Colonoscopy. Source: Cancer Research UK
“If patients are reading too much into symptoms before colonoscopy, they could convince themselves they have any of a myriad of medical conditions.
“Rather than worry about symptoms and black specks or coloring of the stool, they should get a colonoscopy or non-invasive colorectal cancer screening test, like Cologuard, to diagnose and eliminate causes of discoloration in the stool.”

This home test, which is non-invasive, uses the latest advancements in DNA technology as it applies to bowel movement samples.
Altered DNA from abnormal cells in the sample can be detected, and this DNA may be associated with colon cancer.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
.
Top image credit: Shutterstock/goodluz
All Known Causes of Very Black Stools

Colon cancer isn’t the only cause of black stools.
“Stools can be dark green or even brown, and if it is dark, it’s okay,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“The color, consistency and smell of a stool are for the most part not as important when it comes to diagnosing a disease or colorectal cancer.
There are certain foods that we eat which choose the color of the stool.”
Dr. Binderow says that in general, the characteristics of BMs are caused by the environment, including food and beverage intake.
If your stools appear to be black, and especially if you don’t have concerning symptoms with this, like loss of appetite, unexplained weight loss, abdominal pain and undue fatigue, re-evaluate what you’ve been eating lately.
Yes, colon cancer can cause stools to be black, “black like tar,” says Dr. Binderow, “different from just a dark brown.”

Shutterstock/Ronald Plett
This is because if colon cancer is up high enough in the digestive tract, the blood from the bleeding gets digested before it exits the anus, resulting in that tar-black color — that then gets mixed with BMs.
Another cause of black stools is from iron, says Dr. Binderow.
“When people are anemic and take iron [supplements], the stool could be black.
“If someone shows up at their doctor’s office, and they have anemia, and the most common cause of anemia is a colon tumor, so they are screened for tumors immediately through colonoscopy.”
Spinach and beets may cause BMs to appear black, especially if viewed in dim light or you don’t have sharp vision.

Under good lighting and wearing vision correction if possible, inspect your poops closely.
Remove a sample from the water and take a good look.
You may then find that what initially appeared to be black is actually a very dark green or purple.
Other foods that can cause this include licorice, dark chocolate, blueberries, cranberries, grape juice, foods with red dye and iron-rich foods (meat, prunes, tofu, oysters, kidney beans, raisins, molasses).
In general, a junk food diet or diet based in highly processed foods results in darker BMs.
Other Causes of Black Bowel Movements
Acute gastritis, cancer (esophageal, stomach), colon polyp, Crohn’s disease, swollen blood vessels in the esophagus, and ulcer.
Dr. Binderow adds, “If a patient does not want a colonoscopy and they are over 50, at average risk of colorectal cancer, they could also take an at-home non-invasive colorectal screening test to test for precancerous and cancerous polyps.”
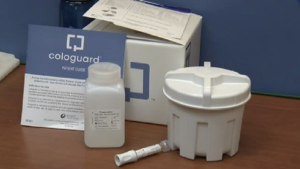
Cologuard is a non-invasive screening test for colon cancer using the latest advances in stool DNA technology — detecting altered DNA from abnormal cells in a stool sample which could be associated with cancer or precancer.
Update on Age to Start Colonoscopy Screenings
The age for getting one’s first screening colonoscopy was changed to 45 by the American Cancer Society in 2018.
This change was a response to an increasing incidence of colorectal cancer in women and men under age 50
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How Does Colon Cancer Cause Thin Ribbon Stools?

Stools that come out like toothpaste from a tube or ribbon-like or thin like pencils can indicate colon cancer.
“If you have an anal or low rectal cancer tumor, your stools might be smaller than normal since this causes the end of the anus or colon to create a toothpaste tube effect – smaller at the tip, so the stool is squeezed thinner than if there was nothing blocking the end of the colon or anus,” explains Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
“A smaller stool is typically caused by anal or low rectal cancer.
“However, it could most definitely be caused by your diet, diarrhea that could be caused by stress and other variables than a cancer.”
There are cases in which ribbon or thin stools are caused by a polyp (precancer) causing an obstruction.
But nevertheless, Dr. Binderow explains, “By the time you have a colon cancer causing symptoms in your stool, the cancer is in the later stages.
“The most important thing to do is to test regularly for colorectal cancer, when you and your doctor find it’s appropriate, which is usually 50 years old, or younger if you are at higher risk.”
The age for starting screening colonoscopies was changed to 45 by the American Cancer Society as of 2018 — because of the increasing incidence of colorectal cancer in adults under 50
Have you had your colon cancer screening?
Dr. Binderow says, “Colon cancer is the only disease, unlike mammography for breast cancer or X-rays for lung cancer, where you can find before it is in a cancerous stage.
“The cancer always starts out as colon polyps, which means if you find one in colorectal cancer screening and remove the polyp during that same procedure, you’ve prevented cancer rather than catching it when it has already progressed into the disease.
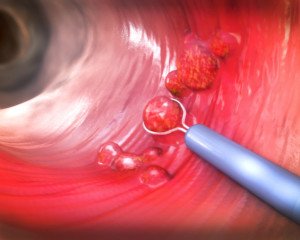
Removal of a colon polyp during a colonoscopy. Shutterstock/Christoph Burgstedt
“This is why it is so valuable to screen whether you screen with a colonoscopy or a non-invasive option like Cologuard, which can be done at home and only requires following up with a colonoscopy if you receive positive results.”
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Prescription Prilosec vs. OTC Prilosec
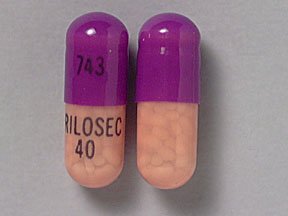
Many people with GERD want to know if there’s a difference between prescription Prilosec and the over-the-counter version.
“This is a relatively challenging question,” says Akram Alashari, MD, a trauma surgeon at Geisinger Medical Center in PA, and author of “THE POWER OF PEAK STATE.”
“I asked my department’s clinical pharmacist and I did some research to find the answer.
“Apparently, there doesn’t seem to be a difference in the drug itself.
However, there is a difference in the indication for administration.”
Dr. Alashari describes the following as approved uses by GERD sufferers for Prilosec as a prescription (there’s no difference in the chemical makeup of prescription Prilosec and the OTC version):
Can be used up to four weeks to treat heartburn and its associated symptoms.
Can be used four to eight weeks to treat endoscopically-diagnosed erosive esophagitis.
The drug has other indications not related to GERD.
The prescription version usually is of a higher dose per pill than the OTC Prilosec.

Dr. Alashari was formerly with Grand Strand Regional Medical Center in SC as an abdominal and critical care surgeon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
3 Ways GERD (Acid Reflux) Causes Shortness of Breath

A doctor explains the three ways that GERD (acid reflux) can cause shortness of breath.
“Shortness of breath,” when it comes to GERD or acid reflux, is more accurately referred to as labored or difficulty breathing, or a sensation that the airway has become constricted.
So it’s not the same “shortness of breath” that you feel after running up two flights of stairs or chasing after your dog.
“Gastroesophageal reflux followed by regurgitation and/or aspiration of gastric juice has been associated with several extra-esophageal complications including asthma,” says Akram Alashari, MD, a trauma surgeon at Geisinger Medical Center in PA, and author of “THE POWER OF PEAK STATE.”
He explains, “Two major mechanisms of reflux-induced asthma have been proposed: aspiration of gastric contents into the lung with consequent bronchospasm.
“Reflux-induced activation of a vago-vagal reflex arc from the esophagus to the lung causing bronchoconstriction.”
And of course, there’s LPR:
Dr. Alashari explains, “Otolaryngologic manifestations of GERD can result from the esophagopharyngeal reflux of gastric contents with subsequent contact injury of the pharyngeal and laryngeal mucosa.
“The term ‘laryngopharyngeal reflux’ has been used to describe this process.”
So those are the three mechanisms through which GERD can cause trouble breathing or the so-called shortness of breath.
Treatment
Dr. Alashari explains, “Drug therapy for laryngopharyngeal reflux typically involves acid suppression with proton pump inhibitors (PPIs). H2 blockers and antacids may provide additional benefits.
“Non-medical therapy includes behavior modification such as ingesting smaller meals; avoid eating within about three hours of sleeping and two hours of exercise; avoid distention of the stomach with excessive fluid during or soon before exercise.”
Finally, to impose more of a control on overnight acid reflux and help prevent nighttime breathing difficulties, you should try a wedge pillow that elevates the torso.

Elevating only the head with an extra pillow or two will not be effective.
Your torso (where the stomach and esophagus are) needs to be propped up at an angle so that gravity assists in keeping acid from refluxing.

Dr. Alashari was formerly with Grand Strand Regional Medical Center in SC as an abdominal and critical care surgeon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ANN PATCHANAN
Migraine Headache Prevention: Top Pills & Non-Oral Treatment

These top seven pills for prevention of migraine headaches are recommended by a neurologist who specializes in migraine pain treatment.
Anyone who suffers from migraine headaches knows that these can reach a pain level of 10 on a one to 10 pain scale.
The pain could be so searing that the patient goes to the emergency room, still in agony despite having an ice pack on their head.
The pain of a migraine can mimic a ruptured aneurysm. For those who’ve already had a clear MRI of their head and who have been diagnosed with migraine disorder, the knowledge that their problem is not being caused by an aneurysm or brain tumor is enormously reassuring.
Nevertheless, the pain can reach breathtaking levels and be disruptive to a person’s life.
Doctor’s Recommendation of Pain Drugs that Can Help with Migraine Prevention
Dr. Brian Loftus is a board certified neurologist in Bellaire, Texas, who specializes in migraine headaches and multiple sclerosis.
He says, “For prevention of migraines – my most frequent seven oral preventatives are zonisamide, duloxetine, candesartan, Topiramate, propranolol, amitriptyline, and Valproic acid.”
Ask your physician about these drugs. Try them as your doctor advises you. Maybe one of them will be the magic charm.
Follow dosing instructions by the book. Ask any questions about these medications.
What about non-oral prevention of migraines?
Dr. Loftus says, “Non-oral preventatives include pericranial nerve blocks, combined sphenopalatine ganglion/cranial nerve V blocks with Allevio, and intermittent IV magnesium.”
These are yet more options for the migraine headache sufferer. In addition, you may want to explore naturopathic options.
But be sure to inform your doctor of any alternative medical approaches, and vice versa.
Both the medical practitioner and the naturopathic practitioner should be aware of the other’s treatments so that they can be configured to complement each other.
Bear in mind that there is no one treatment that prevents migraine headaches 100 percent of the time for every patient. But all options need to be given a chance.
Dr. Loftus has a private practice in Bellaire, TX, and focuses on headaches, multiple sclerosis and hyperhidrosis (excessive sweating). He is also board certified in headache medicine.
has a private practice in Bellaire, TX, and focuses on headaches, multiple sclerosis and hyperhidrosis (excessive sweating). He is also board certified in headache medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photoroyalty
Sudden Onset Headache with Last Bench Press Rep: Causes?

A sudden severe headache with that last bench press rep can have one of several possible causes.
Can Rogaine Be Applied Like Shampoo on Entire Scalp?
Are you thinking of applying Rogaine (minoxidil) throughout your entire scalp to combat diffuse hair loss?
Not all hair loss is the same. Some people suffer from it in a diffuse or scalp-wide way, rather than a focal point like the notorious “bald spot” on the top/back of the head or the receding hairline and temple balding.
How effective would Rogaine (minoxidil) be if you were to apply the foam ALL OVER your head or drip the liquid from the medicine dropper all over your scalp (though this would be very messy)?
“I have seen patients who tell me they do apply it throughout their entire scalp, but have seen very limited positive results in doing so,” says Dr. Robert Dorin, DO, NYC-based hair care expert and restoration specialist.
“It appears that the people who have a true diffuse hair loss pattern, are typically not helped by the use of Rogaine,” continues Dr. Dorin.
“This type of pattern tends to be resistant to the benefits of Rogaine and appears to have a different etiology.
“There are numerous types of hair loss, and unfortunately, Rogaine does not work for all equally.”
Have you tried Rogaine (minoxidil) yet?
This isn’t to say that for 100 percent of the people who try it all over their scalp, that it would fail to stimulate regrowth.
It’s definitely worth a shot. There’s no question in the medical community that minoxidil indeed spurs new hair growth in deactivated follicles.
For some people it works. For others it fails. You will not know which group you fall under UNTIL you give minoxidil a fair shake.
You just might love the results! But there’s a few catches.
Using Rogaine — or Minoxidil — on the Entire Scalp
Again, they are one and the same, from a chemical formula standpoint. The first catch is the price. Minoxidil is the generic version and far cheaper than Rogaine.
But using it on your entire scalp means you’ll go through the bottles pretty quickly.
If you don’t mind this new monthly expense, then give it at least four months to work — as the instructions tell you to.
The second catch is the drippy mess while using the medicine dropper.
If you’re using the drug on your whole scalp, you need to be patient and careful, and embrace the concept of trial and error to get it just right.
Foam minoxidil is not recommended for the whole scalp. Most of it will end up on your hair, not in your follicles. Stay with the liquid formula.
Dr. Dorin of True & Dorin provides creative hair loss solutions, including advanced hair transplant techniques and the latest in regrowth technology, to ensure that his clients achieve their desired results.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why Can’t Rogaine (Minoxidil) Be Made a Shampoo?

A hair loss doctor explains why minoxidil can’t be made in shampoo form.
Rogaine (generic name minoxidil) comes in either a liquid form that’s dripped onto the scalp from a medicine dropper, or a foam version which is dabbed onto the area of hair loss.
This sounds wonderful for focal hair loss, but what about diffuse hair loss?
This means “head-wide” loss of hair volume due to an increasing number of dormant follicles.
What’s a person to do…apply the minoxidil liquid from the medicine dropper all over the scalp, covering every portion? Or massage in gobs of the foam?
Well, why not Rogaine in shampoo form?
What a Hair Loss Physician Says
“The reason why Rogaine is not made in a shampoo form is simply because it is not an effective way to deliver the minoxidil drug to the follicles,” says Dr. Robert Dorin, DO, NYC-based hair care expert and restoration specialist.
“If one stops and thinks about it, during shampooing, one applies the shampoo to the scalp and rubs, or lathers it up with some water in the hair and scalp for a period of maybe 2-3 minutes at most, then rinses the shampoo off down the drain and along with it the minoxidil.
“The minoxidil would only be in contact with the scalp for this time, partially diluted with water for a very short period of time (2-3 minutes at most), then rinsed off with the shampoo detergent.
“This would never give the minoxidil enough time to be absorbed into the scalp and reach the dermal layer (where the follicles live), allowing the drug to affect the follicles.”
Makes sense! So what about lightly working the foam throughout much of the scalp if you have diffuse hair loss?
If you have very short hair, especially like a crew cut, this would actually be easy to do.
You’d just have to stand there and patiently dab the Rogaine foam through (not rubbing it in, but just getting it in contact with the scalp).
However, if you have long hair (such as a woman with diffuse hair loss or “thinning”), this will be a problem, as much of the foam will end up on the hair rather than the scalp to penetrate into the follicles.
Women or men with long hair may want to stick to select wide parts that they can always easily find and run the medicine dropper along those, or apply the foam down those with their fingertips.
Maybe one day there will be a shampoo for triggering hair regrowth. Until then, you’ll need to stick to the Rogaine/minoxidil liquid or foam.