
Trouble breathing with chest pain after joint replacement surgery never has a benign cause, says Barbara Bergin, MD, an orthopedic surgeon.
NEVER assume that chest pain with difficulty breathing following joint replacement surgery is a sign of anxiety.
What can chest pain and feeling like you can’t get enough air actually mean?
“This would be a bad sign,” says Dr. Bergin, board certified orthopedic surgeon at and co-founder of Texas Orthopedics, Sports & Rehabilitation Associates.
“I can’t think of a benign process which would cause chest pain and trouble breathing after a total joint replacement, unless you coincidentally sustained an injury to your chest or ribs.
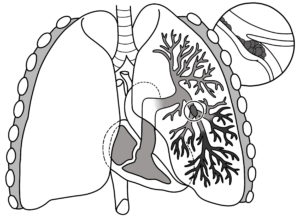
“Otherwise, you’re either experiencing a heart attack, or more likely…a pulmonary embolism, which is the result of a blood clot which has dislodged from the leg and entered the lungs.”
Father Had a Knee Revision Operation
I visited my father in his room three hours after his knee joint revision surgery.
On both feet were sequential compression devices that periodically inflate to squeeze against the patient’s feet to generate circulation in the legs to prevent blood clots.
He was also on the blood thinner Warfarin and was wearing knee high compression stockings.
Shortness of Breath and Chest Pain While Still in the Hospital
The hospital stay for a knee or hip replacement surgery is normally several days.
The patient himself, upon experiencing chest pain or diffiulty with breathing, may be able to press the nurse’s call button if alone.
The diagnosis of a pulmonary embolism, however, can only be made with a CT scan. There may be a few other tests as well.
Pulmonary Embolism
Only after this confirmation would the patient be givn a clot-busting drug via an I.V. — per doctor authorization.
Never would the patient receive such a drug without FIRST a diagnosis of a pulmonary embolus.
Naturally, I wondered what would happen if my father suddenly developed chest pain and shortness of breath, and on the way to the CT scanner, the pulmonary embolism got bigger and completely blocked his ability to breathe!
“A large blood clot to the lungs can kill you in short shrift,” says Dr. Bergin.
Why a Blood Clot Forms
“After surgery on the lower extremities, the blood coagulation process is in a heightened state,” says Dr. Bergin.
“This happens throughout the whole blood supply, in response to having a cut anywhere in the body.
“But in the leg, the circulation of venous blood gets sluggish because of the surgery and swelling.
“The movement of blood through the veins is assisted by movement of muscles.
“This helps pump venous blood out of the extremities, because veins have no ability to pump blood, like arteries do.
“What happens after surgery? We’re lying around in bed, not moving our leg, because it hurts [knee or hip replacement].
“So heightened coagulation + surgical swelling + less movement of the leg = increased potential to have a blood clot in the leg.
“This process usually takes a few days, but occasionally, it happens sooner. Some patients are more susceptible to developing blood clots, so it can happen within 24 hours.”
Trouble Breathing, Chest Pain Soon After Discharge
The patient continues to recover from joint replacement surgery at home. They then develop these two symptoms.
“This is an emergency, and under no circumstance should it be ignored,” says Dr. Bergin. “Call your surgeon, or better yet…call 9-1-1.”
Deadly Saddle
The type of pulmonary embolus that can kill in a minute is called “saddle,” because it blocks blood flow to both lungs at the same time — sealing off the entrance to any inhaled oxygen.
However, the saddle P.E. is not likely to strike a healthy person, even if they’re over 80.
It’s more likely with someone who has a pre-existing clotting disorder or very poor health.
The type of pulmonary embolus that usually develops in joint replacement patients are smaller clots that occupy only one lobe of the lungs (a pair of lungs has five lobes total).
A patient could have trouble breathing because a clot is in one lobe, but still be able to breathe with the four other lobes and have plenty of time for a CT scan and diagnosis.
Can shortness of breath + chest pain after a joint replacement have a less serious cause?
Dr. Bergin explains, “Occasionally chest pain and shortness of breath can be due to stomach acidity.
“But don’t assume that,” EVEN IF the patient has recently been diagnosed with a bad case of acid reflux.
“Chest pain and shortness of breath after surgery on the lower extremities means heart attack or pulmonary embolism until proven otherwise. You’re off to the ER in short order” if this occurs after the patient returns home.
As for my father, I was always on high alert, periodically asking him if he felt short of breath or had chest pain. He had no complications and fully recovered.

Dr. Bergin is a general orthopedist, surgically and conservatively treating all manner of bone and joint conditions. She enjoys educating patients so they can emerge stronger than they were before their orthopedic injury or surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.













