Can Burping Be the ONLY Symptom of a Serious Heart Problem ?

If you’re wondering why your new-onset burping might be caused by a heart problem, you’d be smart to see a cardiologist; it’s possible for angina to cause only one symptom: burping.
“Yes, gastrointestinal symptoms are often common in heart attack presentation,” says Dr. Lowell Steen, MD, Interventional Cardiologist at Loyola University Medical Center, Director of the Interventional Cardiology Fellowship Training Program, and Medical Advisor to 120/Life, a functional beverage with a blend of six natural ingredients that promote normal blood pressure.
“The heart has no direct pain fibers, so the pain is referred. That is why patients can have arm, jaw or chest discomfort.
“Burping, nausea and vomiting may be presenting symptoms of a heart attack.”
“Typical angina” is chest pain caused by clogged coronary arteries.
Sometimes this condition is accompanied by other symptoms: shortness of breath, dizziness and nausea.
But it’s entirely possible for typical angina to present with only symptoms that seem related to the digestive tract, such as burping.
The Sultan Qaboos University Medical Journal (Dec. 2007) reports the case of a man, 62, who’d apparently been healthy all his life.
However, for the two months prior to his presentation to a doctor he’d been suffering from unexplained burping. This was his only complaint.
One Symptom: Burping – Diagnosis?
He was diagnosed with angina pectoris, even though he did not report any chest pain, shortness of breath or other symptoms.
He had to undergo surgery to treat his severe heart disease. The SQUM Journal states:
“It is concluded that belching can be a presenting symptom of angina.”
And of course, angina is a heart problem – sometimes requiring coronary bypass surgery, depending on the extent of arterial blockage.
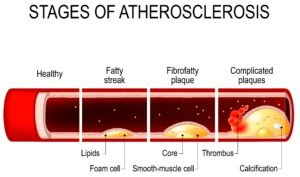
Shutterstock/Designua
“Belching or painful swallowing are suggestive of esophageal disease,” says the Journal, “although belching and indigestion may be seen with myocardial ischaemia.”
Myocardial ischaemia (or ischemia) is a fancy way of saying shortage of oxygen to the heart muscle.
How Rare Is Burping As an Only Symptom of a Heart Problem?
There is no quantitative data. “Belching as an isolated symptom of angina without chest pain, have not been reported before,” states the Journal, “and was not included as a common presenting symptom of angina pectoris in the standard textbooks of medicine and cardiology.”
Bear in mind that this study comes out of the nation of Oman, which has a significantly smaller population than the United States.
We can only imagine how many people in the U.S. or another heavily populated and industrialized nation have suffered from burping as their only symptom of heart disease – and were never properly diagnosed – and eventually died of a heart attack.
This is why new-onset, unexplained belching needs medical attention: See a cardiologist before you see a gastroenterologist.
A digestive issue such as acid reflux can wait.A heart problem can’t.
A Closer Look at the Man Whose Only Symptom of Dangerously Clogged Heart Arteries Was Burping
• Patient reported burping episodes after feeling gassy in his stomach for two months.
• The gas and belching occurred only during physical activity such as using a staircase and even walking, plus also emotional stress.
Interjection: That second bullet point makes a heart problem highly suspect in the case of burping as an only symptom!
PAY ATTENTION to events preceding worrisome symptoms – and document them!
• Needless to say, the patient reported no connection between his symptoms and eating, and they did not occur at rest, either.
• He was not on medications; never had surgery.
• Pulse, blood pressure and blood tests were normal.
• A resting ECG was normal.
• An echocardiogram stress test—during which he belched – showed angina pectoris.
Belching Caused by Blocked Heart Arteries
• An angiogram revealed 50 percent narrowing of two major coronary arteries.
• A third major artery and its branch had 98 percent blockage.
• Treatment was bypass surgery, statins and aspirin.
• The burping disappeared after this treatment.
“The only explanation for the cause of belching in this patient was angina pectoris,” notes the Journal.
The paper points out that the symptoms of belching and gas were related only to physical activity and emotional stress – a strong suggestion of a heart problem.
Though it’s not difficult to locate medical literature describing the symptom pairing of burping AND chest pain originating from a cardiac disease, the literature on burping as the ONLY symptom of heart disease is very scant.
Why would heart disease cause burping at all?
The paper’s author speculates involvement of the vagus nerve, which passes through the chest.
A marked vagal stimulation, that is associated with a shortage of oxygen to the heart, can cause gastric upset – leading to formation of gas – making one burp.
 Dr. Steen’s clinical expertise includes angioplasty, chest pain, coronary artery disease, heart attack, high blood pressure, valve disease, and vascular disease and intervention. 120life.com
Dr. Steen’s clinical expertise includes angioplasty, chest pain, coronary artery disease, heart attack, high blood pressure, valve disease, and vascular disease and intervention. 120life.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
Source: ncbi.nlm.nih.gov/pmc/articles/PMC3074882/
Can a Heart Problem Cause the Legs to Feel Cold?
If you’re wondering whether a heart problem can cause a cold sensation in the legs, your hunch is dead-on.
That cold feeling in your legs can be caused by congestive heart failure. (more…)
Why Frequent Urination Overnight Can Be Caused by Menopause

If you’re menopausal and find that you keep getting up overnight to use the bathroom, you may want to blame the menopause for this intrusion upon your sleep.
Yes, urinary function can be altered by menopause via the route of vaginal and urinary tract shrinkage – thanks to diminished production of estrogen.
It’s been commonly called urogenital or vaginal atrophy.
“Vaginal atrophy (now officially called genitourinary syndrome of menopause, or GSM) is a common contributing factor to overactive bladder,” says Michael Ingber, MD, board certified in urology, female pelvic medicine and reconstructive surgery, and founder of The Center for Specialized Women’s Health, division of Garden State Urology.
Furthermore, less estrogen means the bladder and urethra will become weaker which can lead to incontinence.
In addition to repeated overnight trips to the loo to relieve oneself, plus the daytime urge incontinence, menopause can also lead to the following problems:
• Stress-related incontinence—triggered by coughing, laughing or sudden movement.
• Increased daytime frequency
“Having the urgency to urinate and urinating frequently is a common problem women develop around and after menopause,” continues Dr. Ingber.
“Rarely, this can be due to how the kidneys function and produce urine. Also, dietary habits (e.g., excess caffeine, fluid intake) can play a role in urinary frequency and urgency.
“More commonly, however, this problem has to do with local problems with the bladder and vagina itself.”
Overactive Bladder and Menopause
Dr. Ingber says that 20% of the population has the so-called overactive bladder, in which the bladder – which is a muscle – spasms, signaling to the brain that it needs to be emptied.
“GSM occurs around menopause, when estrogen levels drop in the blood due to decreased production by the ovaries,” explains Dr. Ingber.
“When this occurs, the vulvar and vaginal mucosa (lining) get thinner, dryer, the pH increases (becomes more alkaline), and women are prone to dryness, discomfort with intercourse, urinary tract infections and overactive bladder.”
Is pre-existing “overactive bladder” necessary for increased peeing from “vaginal atrophy”?
“Overactive bladder is simply our term that describes women who urinate more frequently than what is considered normal,” says Dr. Ingber.
“Two-thirds of women are dry and just have to urinate frequently both day and night, and one-third of women are wet.
“This means they often have to wear a pad or change their underwear because they have an accident before reaching the toilet.
“We no longer think of them as separate conditions. They are interrelated and that is why whenever someone presents with a lack of vaginal estrogen, when they have urinary symptoms, we offer them treatment for the actual vaginal problem including vaginal hormone therapy or our novel MonaLisa Touch CO2 laser.
“This is also why we no longer use the term ‘vulvar and vaginal atrophy,’ but rather, ‘genitourinary syndrome of menopause.’”
Treatment for Frequent Overnight Urination from Menopause
“There are lots of treatments for this condition including exercise [Kegel], medical therapies and procedures that we do,” says Dr. Ingber.
“Because of this, vaginal hormone replacement can be an essential component of a woman’s pelvic health and quality of life.
“There are currently vaginal creams, tablets and even a ring which can be inserted. The goal of these therapies is really only to increase the vaginal health, not to increase blood levels of estrogens and affect the rest of the body.
“In general, these therapies are safe for most people, although, there may be a slight risk in women with a history of breast or endometrial cancer in taking these therapies.”
Fat loss and biofeedback can also help.
“There is now a SERM (non-hormonal oral therapy) called Osphena, which is a daily pill for women complaining of dryness during relations. This works very well.”
MonaLisa Touch – Just Five Minutes
“Lastly, there is a new non-hormonal option called the MonaLisa laser for atrophy,” says Dr. Ingber.
“This is an in-office therapy which takes five minutes, without pain, no anesthesia, which stimulates the vaginal tissue to produce collagen, thicken and restores the vagina to the premenopausal state.
“Several studies have shown benefit to the use of vaginal estrogen therapy for overactive bladder symptoms.
“There are a few studies which appear to show that the MonaLisa laser may also improve these symptoms.”

Dr. Ingber is board-certified in Urology and Female Pelvic Medicine & Reconstructive Surgery; is a Fellow of the International Society for the Study of Women’s Sexual Health. The Center for Specialized Women’s Health, division of Garden State Urology & Atlantic Medical Group.
specializedwomenshealth.com
(973) 537-5557
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, jcomp
What Kind of Brain Damage Can Anemia Cause?
If anemia is severe enough, it can damage the brain.
It’s easy to see why anemia could lead to brain damage. The brain depends upon oxygen for proper functioning.
Blood delivers oxygen to the brain, as it does to all organs.
When the brain doesn’t get enough oxygen, and this situation is not resolved in a timely manner, there then is a risk for permanent damage — though this wouldn’t be severe in degree.
“Little is known about the relationship between anemia and brain damage, but some limited studies suggest that anemia can mildly impair memory as well as the thinking abilities involved in everyday activities such as shopping, paying bills, etc.,” says says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
Dr. Tavel adds, “Even less is known whether correction of anemia will correct any impairment of brain function or damage, but in all likelihood, brain function should return to normal.”
Anemia’s Three Main Causes
• Loss of blood (e.g., internal bleeding, traumatic injury)
• Insufficient red blood cell production
• High rates of red blood cell destruction
A type of anemia called “pernicious” can damage the brain if not treated.
As Dr. Tavel says, the negative effect on the brain can affect concentration and memory. Other cognitive symptoms: confusion, depression.
The body needs vitamin B12 to manufacture red blood cells. Inadequate supply of B12 – often either via diet or due to a lack of a special protein that’s made in the stomach – will lead to pernicious anemia.
If pernicious anemia is severe or goes a long time without treatment, damage to the brain, as well as to other organs including the heart, will result.
As terrible as this sounds, the condition is actually simple to treat with B12 supplementation.
Prior to the development of supplements, the condition was deadly, hence the name “pernicious.”
Classic Signs of Anemia from Any Cause
• Fatigue that can’t be explained by benign causes such as lack of sleep, excessive physical activity or not eating enough.
• Feeling like you can’t get enough breath, as though you’ve been exercising – only you haven’t.
• Dizziness
• Headache
• Pale skin
• Chest pain
• Cold hands and feet
These symptoms can have many other causes, some more serious, some less serious.
In addition to the pernicious type, there are many other causes of anemia.

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Sources
nhlbi.nih.gov/health/health-topics/topics/anemia/causes
nhlbi.nih.gov/health/health-topics/topics/prnanmia/
nhlbi.nih.gov/health/health-topics/topics/anemia/signs brain damage
Doing the Deadlift, Squat and Lunge While Pregnant: Guidelines
![]()
The very exercises that are associated with power, muscle & competition are actually among the safest for a pregnant woman: squat, deadlift and lunge.
The back squat, deadlift and lunge (stationary or walking) are quite safe for the healthy pregnant woman.
However, some pregnant women who are strength training enthusiasts hesitate to do any of these compound moves.
Maybe this is because the back squat and deadlift are the very exercises that the strongest people in the world do for competition in powerlifting, strongman and CrossFit events.
But don’t let that trick you into thinking that the squat and deadlift, along with lunges, are not safe during your pregnancy.
It’s just that these three multi-joint movements are so versatile that they fit very nicely into any kind of strength training regimen.

Shutterstock/Paul Aiken
Another reason a pregnant woman might think the back squat, deadlift and lunges are not safe is because these exercises are done at very intense or mechanically heavy levels by serious fitness enthusiasts.
And though five sets of 5 RM deadlifts with only 90 seconds in between each set will leave a trainee feeling pummeled, remember … a deadlift routine can be adjusted to suit a woman who’s even nine months pregnant.
But there is one consideration you need to be aware of…
“In a normal healthy pregnancy, you likely can continue these exercises if you were doing them prior to your pregnancy,” says Danielle DonDiego, DO, a family physician and obesity specialist with SteadyMD, an online program where patients can call, text or video chat with their doctor anytime.
Dr. DonDiego is also a certified personal trainer and explains, “If these are a normal part of your routine, you can continue — as long as you haven’t been told otherwise by your personal physician.
“However, pregnancy is not a good time to start these types of exercises (or any other new and extreme training regimen). Continue what you were doing previously as long as your doctor says it’s okay.”
Why the Squat, Deadlift and Lunge Are Safe for Healthy Pregnant Women
The guidelines that are set forth by the American College of Obstetricians and Gynecologists encourage resistance training and do not prohibit the specific movements of the back squat (or any version), deadlift or lunge.

Shutterstock/Serghei Starus
But remember, it’s not wise to begin barbell squats and deadlifts for the first time while you’re expecting.
Already been doing these exercises?
The ACOG discourages anything that brings on symptoms or puts a pregnant woman at risk for falling or collisions.
By these guidelines, it would actually be much safer for a healthy pregnant woman to perform her usual sets of deadlifts or a squat variation than to participate in some kind of cardio activity – even light – in which she might stumble and fall — such as a hike or step class.

Shutterstock/Serghei Starus
Premature Labor
“There are only anecdotal reports that strenuous training may cause preterm labour,” states a report in the British Journal of Sports Medicine.
However, the training that’s referred to is aerobic, not strength.
“Nonetheless, until there is unequivocal evidence that strenuous exercise has no impact, a physically active woman with a history of, or who is at risk of, preterm labour should be advised to reduce her activity in the second and third trimesters,” continues the report.
If you’re at risk for preterm labor, definitely discuss strength training with your OBGYN, but again, the issue would involve intensity, not type of joint movement.
As long as there are no contraindications, a pregnant woman should embrace consistent, medium-intensity exercise for the same health benefits during pregnancy as prior to pregnancy.
When it comes to pregnancy and exercise, the big issues are intensity and risk of falls or collisions.
You can clearly see that three sets of 8-12 RM barbell squats are a lot safer than playing volleyball or participating in karate classes – the latter two which put a pregnant woman at risk for collisions or contact with other participants.
The paper in the British Journal of Sports Medicine points out that, just to play safe, it would be smart to avoid heavy resistance or any movements “that result in a large pressor effect during pregnancy.”
So just because you’ve been doing squats, deadlifts and heavy-weighted lunges long before you became expectant doesn’t mean that you should continue killing it during your pregnancy.
You can continue doing these exercises, but your heaviest squats and deadlifts are out, as these involve a large pressor effect.
A pressor effect refers to a rise in blood pressure. BP will rise during weightlifting, but the report refers to a “large” pressor effect.
You should discuss this with your doctor.
You should run your desired strength training program by your OBGYN.
Don’t just name specific exercises to your doctor, but ask about intensity and see what your doctor says.
Do not speak in terms of amount of weight lifted.
This is because, for example, a 135 pound deadlift, to your female physician who doesn’t strength train, might seem like an ultra-heavy lift – while it’s only your warmup!
Instead, speak in terms of protocols that make you strain and grit your teeth to get in the last few reps, that leave you heaving heavily at the end of the set.
Straining with heavy weights spikes blood pressure, but again, “heavy” is relative.
The 135 pound deadlift would spike the blood pressure of your non-trained doctor, but to a strong, experienced lifter it has less effect on her blood pressure because 135 is way below her working weight load.
Your OBGYN may not even know what a back squat and deadlift are.
Explain these and again, speak in terms of effort level (“I’m straining my guts out,” “I must grunt for the last few reps,” “When I’m done I’m only moderately out of breath,” etc.), rather than amount of weight lifted.
As for the walking lunge, the issue here may be balance for some women.
Pregnancy may throw off sense of balance. If you’ve never lunged before, there’s no reason to begin these during a pregnancy.

Shutterstock/Paul Aiken
A great alternative to lunges is the dumbbell squat — especially for those women who don’t feel comfortable with the barbell squat.
Dumbbells can be held at shoulder level, at the sides with straight arms or at chest level with bent arms.

Allie Edwards, a CPT specializing in prenatal and postpartum fitness, endorses the squat and other strength training exercises such as the kettlebell swing for expectant women.
Warning for Expectant Strength Trainers
Regardless of intensity level as well as type of weightlifting movement, the ACOG says to immediately cease activity if any of the following occur:
• Vaginal bleeding or leakage of amniotic fluid
• Difficulty catching breath – before the exercise starts
• Dizziness
• Headache
• Nausea
• Unexplained muscle weakness
• One calf with unexplained pain
• One calf that’s swollen, tender or unusually warm
The deadlift, squat and stationary lunge, from a mechanical standpoint, are very safe for pregnant women.
• Performed in one spot with both feet planted on the floor.
• Risk of losing balance is minimal.
• No impact to joints, no jarring motions.
 Dr. DonDiego focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
Dr. DonDiego focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
 Allie Edwards runs two blogs: The Perfect Pregnancy Plan and Vigor it Out. Edwards, a mother of three, is a certified personal trainer specializing in prenatal and postpartum fitness. She’s also certified in nutrition and lifestyle during pregnancy, and child nutrition and cooking.
Allie Edwards runs two blogs: The Perfect Pregnancy Plan and Vigor it Out. Edwards, a mother of three, is a certified personal trainer specializing in prenatal and postpartum fitness. She’s also certified in nutrition and lifestyle during pregnancy, and child nutrition and cooking.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/pixelheadphoto digitalskillet
Source: bjsm.bmj.com/content/37/1/6.
How to Minimize Pain During Core Needle Biopsy for Breast Cancer

There are multiple key factors that influence the amount of pain during a core needle biopsy when breast cancer is suspected. (more…)
Questions to Ask Your Doctor Before Having a LEEP

Facing a LEEP procedure can have some women quite unsettled, but if you arm yourself with the right questions to ask your doctor, you’ll feel more in control and less nervous. (more…)
How Long Does It Take for CIN 3 to Become Cancer?
It takes a lot longer than you think for CIN 3 to undergo a transformation to cancer if left untreated.
If you’ve been diagnosed with CIN 3, there is no reason to panic and fear for your life.
Of course, this high grade level of cervical dysplasia is nothing to sweep under the rug, either.
CIN stands for cervical intraepithelial neoplasm.
Time It Takes CIN 3 to Become Cervical Cancer
There are only estimates in how long it takes CIN 3 to eventually transform into an invasive cancer if left untreated.
A specific timeline is not known, says Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
“Generally speaking, it’s a slowly progressing process,” continues Dr. Riobe.
“Studies to determine this are not allowed due to ethics around allowing an invasive cancer to progress from a noninvasive condition.
“CIN 3 is treated as soon as detected, and conservative management is not appropriate, so it would be extremely difficult to find out the time of progression.”
The estimation ranges from 10 years (12 out of 100 women) to 30 years (50+ out of 100 women).
So if you’re diagnosed with CIN 3 and don’t have it treated, there’s a very small chance it will take about 10 years’ time to turn into cancer.
However, in no way does this mean to take such a diagnosis lightly. Don’t panic, but don’t turn your nose up at it, either.
“Given that cervical cancer was the most common cause of GYN cancer deaths prior to the development of the Pap smear, conservative management is not appropriate in the case of CIN 3,” says Dr. Riobe.
If you’re diagnosed with CIN 3, it’s best you discuss treatment options with your gynecologist.
Do not do nothing; it needs treatment. But definitely do not lose sleep and worry about dying, either. And if you smoke, QUIT.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: ncbi.nlm.nih.gov/pubmedhealth/PMH0072440/#i2109.frueherkennung-gm.developmentofdysplas
Can CIN 1 (Mild Cervical Dysplasia) Go Away on Its Own?
CIN 1 will go away on its own in most women diagnosed with this, but there is a small percentage of unlucky women whose CIN 1 will progress to a higher grade.
“Yes, CIN 1 may resolve spontaneously in 50 percent of cases in immunocompetent women,” says Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
Dr. Riobe continues, “Patients who are immunocompromised are less likely to have resolution.
“Cigarette smokers are also less likely to have resolution of CIN 1 without intervention due to the negative impact of cigarettes on immunity.”
Two studies show interesting percentages of resolution: One shows 75 percent — but it was a very small study — and a much larger study shows about 30 percent.
First Study: American Journal of Obstetrics and Gynecology (August 1999)
A study led by Randall K. Falls, MD, wanted to evaluate spontaneous disappearance of CIN 1 (low grade dysplasia) among patients of a private practice.

Shutterstock/Iryna Inshyna
• 100 patients with CIN 1 were offered either repeat Paps every three months for a year or actual treatment.
• 89 percent of the patients underwent the serial Paps.
• Of those 89, spontaneous resolution of CIN 1 occurred in 67, based on two consecutive Pap smears after the original (low grade) smear. Colposcopy confirmed resolution.
• At the one year mark, 17 women, whose smears did not show that their original CIN 1 had gone away, were treated for “persistent atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesions” via a loop electrosurgical conization.
Of those 17 patients…
• One had CIN 2.
• Four had progression before one year.
Study Conclusion
Because CIN 1 has a high rate of going away on its own, the paper states that serial Pap smears is “safe” in a “reliable patient population.”
What About a Larger Population Study?
The May/June 2008 issue of Anticancer Research has a very interesting report. The study authors wanted to assess the natural history of low grade dysplasia.
The patients had been referred for colposcopy from January 1996 – July 2005: 1,001 women with CIN 1.
• After six months, 330 patients’ CIN 1 had disappeared.
• 305 patients still had the low grade dysplasia.
• 45 had a progressed pathology.
At 12 Months…
• Of the 330 whose CIN 1 had gone away, 200 remained negative; 42 had a recurrence of their low grade dysplasia; and nine actually progressed to a higher grade.
• Let’s back up: For nine women whose CIN 1 was gone at the six month mark, the dysplasia was back after 12 months – but worse.
• Of the 305 women who, after six months still had CIN 1, 131 were negative at the 12 month mark; 121 still had CIN 1; and 10 had gone to a higher grade.
Study Conclusion
The conclusion of Nisha Bansal, MD’s study is that there’s “a low rate of progression for CIN 1, suggesting it may be reasonable to prolong the screening interval in women with CIN 1.”

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
Sources:
sciencedirect.com/science/article/pii/S000293789970548X
ar.iiarjournals.org/content/28/3B/1763.short
Can Breast Cancer Cause a Bruise-Like Area on the Skin?
An especially aggressive form of breast cancer can cause the appearance of bruising on the breasts.
So how do you tell the difference between the bruise-like area of this kind of cancer and that of a benign bruise from skin trauma?
“This sign tends to happen in a less common and aggressive forms of cancer called inflammatory breast cancer, and the skin change is caused by the tumor cells blocking proper lymphatic drainage in the skin,” explains Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine.
Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
“It can also make the skin appear like an orange peel and this is called “peau d’orange,’” says Dr. Riobe.
A bruise from skin trauma (e.g., bumping into something, getting bumped into, impact from a ball, child’s playful hand, or adult hand in a karate class) follows a predictable course.
The skin that covers the breasts is no different than the skin that, say, covers your legs.
A bruise on your breast from an external source will progress and appear the same as bruises on your legs, butt or arm.
Bruising from External Trauma
- 0-2 days: pinkish or “red”
- 2-5 days: blue and/or purple
- 5-7 days: green
- 7-10 days: yellow

Normal bruise. Shutterstock/Stephane Bidouze
It can take about two weeks for a typical bruise to vanish, though big “ugly” ones from more forceful trauma will take longer – but they’ll still follow a predictable course.
Inflammatory breast cancer affects one percent of all BC cases in the U.S. yearly. This means about 2,300 new cases/year, making it a rare disease.
Bruise of Inflammatory Breast Cancer vs. Benign Bruise
Inflammatory breast cancer can visibly progress over a matter of days, even hours.
It’s not likely that a bruise on your breast that’s progressing according to the color guide above is a sign of IBC.
The bruise as the only symptom – over a period of time – is a reassuring sign, but keep an eye on it to see if it does – or doesn’t – follow the color progression of a harmless bruise.
If it’s still there after two weeks and doesn’t seem to be following the color progression, AND if it’s gotten bigger for no apparent reason, see a doctor.
Other Symptoms of Inflammatory Breast Cancer
• Redness covering a large surface area of the breast; may come and go.
• Swelling, which may involve only part of the breast.
• Unusual warmth, aching or tenderness.
• Appearance of hives, welts or bug bites.
• Unusual inversion or flattening of the nipple.
• Any other frightening (usually sudden onset) appearance of the skin, including a surface that resembles an orange peel.
Trust your gut if you begin feeling uneasy at what you’re seeing. It’s reassuring if you recall a recent collision of something with your breast.
Keep a close eye on any new bruise for suspicious changes.
Inflammatory breast cancer is sometimes misdiagnosed as eczema!
Get a second opinion if this is your diagnosis and your gut is doubtful.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Olympus Digital Camera
Discomfort Behind Breast when Swallowing: Cancer May Be Cause