Do Children Get Pancreatic Cancer?

If children can get pancreatic cancer, just how many actually develop this disease? And what should parents look out for?
“I have not seen this in my career,” says Robert Saul, MD, a board certified pediatrician for 40+ years and Professor of Pediatrics at Prisma Health Children’s Hospital and the University of South Carolina School of Medicine.
Dr. Saul adds, “But yes, children can get pancreatic cancer.”
In fact, even infants can be diagnosed with pancreatic cancer – a disease that can strike at any age.
However, “can” does not mean that parents should worry that their child might have pancreatic cancer.
Certainly, if one’s child is experiencing new and unexplained symptoms, they should be seen by a pediatrician.
Let the pediatrician take it from there, and do not worry about a disease that has an incidence of 0.46 cases per one million people under age 30.
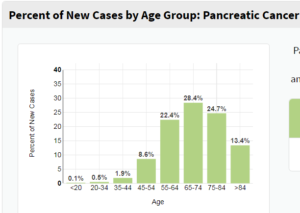
The median age of diagnosis is 70, but one tenth of a percent of cases occur in people under the age of 20. Again, this includes babies.
See the chart below from the National Cancer Institute Surveillance, Epidemiology and End Results Program for number of diagnosed cases per age bracket.
The Journal of Pediatric Surgery has covered the phenomenon of pancreatic cancer in children.
In one paper, one particular medical institution had six cases of pediatric pancreatic neoplasms between 1971 and 1991.
So it’s exceedingly rare, but not impossible, for this age group to get this very difficult to treat disease.
The six patients were between three weeks old and 16 years.
There are different kinds of pancreatic cancer. In the case of these young patients, there were one insulin-secreting tumor, one pancreatoblastoma and three solid cystic tumors.
The paper reports that surgery was the only treatment, and that the young patients were all alive on an average of 7.8 years later.
Another paper of the same journal but different issue reports on 58 patients having either an exocrine type of tumor, endocrine type or sarcoma.
The pancreatoblastoma was more commonly seen in kids under 10 years.
About half the 58 patients had metastatic disease, and 44 percent of these entailed the endocrine type.
Don’t Ignore Symptoms
If your child starts having abdominal pain, nausea or fatigue, you certainly do not want to start fearing that he or she might have pancreatic cancer.
It really is just so unlikely.
But DO take your child to their pediatrician to find out what’s behind these or any other new symptoms.
 Dr. Saul is the coauthor of “Thinking Developmentally: Nurturing Wellness in Childhood to Promote Lifelong Health,” and author of “Conscious Parenting: Using the Parental Awareness Threshold.” His website is mychildrenschildren.com.
Dr. Saul is the coauthor of “Thinking Developmentally: Nurturing Wellness in Childhood to Promote Lifelong Health,” and author of “Conscious Parenting: Using the Parental Awareness Threshold.” His website is mychildrenschildren.com.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sources
sciencedirect.com/science/article/pii/002234689290284E
jpedsurg.org/article/S0022-3468(08)00894-4/abstract
seer.cancer.gov/statfacts/html/pancreas.html
Are Heart Palpitations Normal with Fibromyalgia?
Your fibromyalgia MAY be the cause of your heart palpitations, but not in the way you might be thinking.
Just because fibromyalgia has been known to cause the perception of heart palpitations doesn’t mean that you can’t possibly have a cardiac arrhythmia or some other disorder that’s causing the fluttering or “skipped” heartbeat.
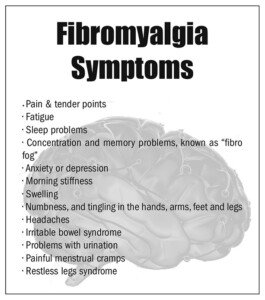
The hallmark features of fibromyalgia are chronic body-wide pain and tenderness. There may also be fatigue and dizziness.
But in fibromyalgia, there is also a dysfunction of the autonomic nervous system (ANS). And the ANS regulates heartbeat.
Many sufferers of fibromyalgia will report that their heart races or pounds after they rise from a seated position.
If all the pulse does is go up, this technically isn’t a palpitation, but rather, merely a sped-up heart rate (tachycardia). Though to the patient, it may be described as “palpitations.”
The tilt table test is very useful in evaluating ANS dysfunction in those with fibromyalgia who report frequent heart palpitations.
Commonly, patients will report tachycardia during tilt table testing. Because it’s triggered by postural changes, it’s called orthostatic tachycardia syndrome.
It means that the pulse has risen more than 30 beats per minute after more than three minutes standing upright.
This doesn’t mean that the heartbeat has literally skipped or fluttered. It’s a steady rate, though elevated.
If you perceive a skipped, fluttering or irregular heartbeat from time to time, and just happen to have fibromyalgia, here is something to consider:
“Fibromyalgia presents with varied symptoms, and yes, some patients with fibromyalgia report palpitations, possibly due in part to increased awareness of pain, and associated anxiety in some patients,” says Glenn Meininger, MD, Director of Cardiac Electrophysiology Services for the Baltimore region of the MedStar Heart & Vascular Institute.
If you have fibromyalgia, it would still be a smart move to have a cardiologist examine you.
“Palpitations can be benign or less worrisome when they are associated in isolation with anxiety, fatigue, alcohol or caffeine consumption, says Melissa Franckowiak, MD, an anesthesiologist in Lockport, NY.
“They can and do occur as part of fibromyalgia, especially since anxiety and fatigue occur more frequently in fibromyalgia patients than in the general population.
“The most important thing to note is how palpitations change in their symptomatology. Has there been an increase in their occurrence or are they becoming associated with chest pain?
“If there has been a noted increase in frequency, duration of how long they tend to last, or if there has been associated chest pain or shortness of breath with them, especially with exertion, they should be reevaluated.”
And keep in mind that other conditions can cause a jumpy heart such as overactive thyroid, persistent anxiety and high caffeine intake.

Dr. Meininger is board certified in cardiac electrophysiology, cardiovascular disease and internal medicine and is widely regarded as an expert in the use of multiple modalities to treat cardiac arrhythmias.
 Dr. Franckowiak is the inventor of two patented medical devices and the CEO of Pneumaglide, providing airway solutions to the surgical services and emergency medical services communities. A fiction writer under the name of Melissa Crickard, she is the author of “The Labrador Response” and “Another Five Patients,” available on Amazon.
Dr. Franckowiak is the inventor of two patented medical devices and the CEO of Pneumaglide, providing airway solutions to the surgical services and emergency medical services communities. A fiction writer under the name of Melissa Crickard, she is the author of “The Labrador Response” and “Another Five Patients,” available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/designer491
Source
springer.com/article/10.1007/s11926-008-0076-8, Current Rheumatology Reports (Dec. 2008)
Can TMJ Disorder Interfere with Nasal Breathing?

Do you have TMJ disorder and now have begun having trouble breathing through your nose?
Temporomandibular joint disorder causes many more symptoms than just jaw clicking and jaw pain. (more…)
Can Wisdom Teeth Removal Cause Nosebleeds?

You just had your wisdom teeth removed. You’re now having bloody noses. Is there a connection?
“Some oozing after wisdom teeth (upper wisdom teeth) removal is to be expected for a few minutes to an hour or two, as the blood from the extraction site could flow through the sinus to the nose,” explains Brijesh Chandwani, DMD, BDS, Diplomate, American Board of Orofacial Pain, with Connecticut & NY TMJ. (more…)
What Makes Tongue Sore Underneath after Dental Work?

Have you ever noticed how sore your tongue was in the hours after receiving dental work?
Does this mean the dentist went to hard on you?
Can it mean that maybe something’s seriously wrong with the area beneath your tongue?
Sore Tongue Underneath After Dental Work
“The structure of the tongue consists of sensitive mucosa due to its highly sensitive function such as taste, speech and digestion,” says Brijesh Chandwani, DMD, BDS, Diplomate, American Board of Orofacial Pain, with Connecticut & NY TMJ.
“It can get irritated with mechanical trauma (such as biting the tongue or roughness in certain foods) or very hot drinks,” continues Dr. Chandwani.
One such food that can cause irritation to the tongue are triangular shaped tortilla chips.
Whether these chips are whole or in fragments, they come with many pointy edges that, when chewed enthusiastically, can cause soreness to the tongue.
If you by chance receive dental work a day or two after eating a lot of pointed-edged tortilla chips or similar food, you’re bound to feel some soreness about the tongue.
Dr. Chandwani continues, “It can also get irritated from friction between tongue and dental work (filling, denture, crown or bridge).
“The dental work may or may not be sharp; friction can make the tongue sore.
“As the tongue is rich in nerve supply (it can even perceive an extremely tiny foreign body such as a piece of hair), it gets aware of the slightest change in its surroundings right away — which sometimes leads to a behavior of repeated physical friction to the new dental work.
“Sometimes the dental work may have to be smoothed/contoured; most times the tongue tends to adapt to the change.”
Give the soreness several days to settle down. Avoid foods that can aggravate any structure inside the mouth (sharp-edged foods, chips, hard candy, shelled candy, raw carrots and celery, even crisp lettuce). Also avoid hot beverages.
And don’t keep feeling your tongue to “test it out.”

Dr. Chandwani has 15+ years of experience focusing on TMJ disorders and sleep disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sheff
Why Don’t Beta Blockers Alone Allow Sports in Long QT Syndrome?
People with long QT syndrome are typically told to avoid playing sports.
And beta-blocker drugs to lower the risk of suffering a sudden cardiac arrest is the standard of treatment. (more…)
Cervical Carcinoma in Situ vs. CIN 3: Is There a Difference?

The last thing a woman with abnormal cervical cells needs is confusion over what exactly she has: carcinoma in situ or CIN 3?
Is there a difference between CIN 3 and an actual malignancy?
“Yes. CIN 3 means the cells are looking abnormal under the microscope and without treatment may develop into cancer,” says Heather Bartos, MD, a board certified OBGYN, and chief of Obstetrics & Gynecology at Texas Health Presbyterian Hospital in Denton, TX.
“Cervical carcinoma in situ means that the cells are cancerous, and that they have not moved out of the location from where they originated.”
Carcinoma in Situ (stage 0)
The word “carcinoma” means cancer. So anything that has carcinoma in its name is malignant.
In situ means local or very confined, or in its original place.
So literally, carcinoma in situ is a cancer that’s still in its original place — and is at its most curable form.
What about CIN 3?
These are precancerous cells. They are not (yet) malignant, but as Dr. Bartos points out, can become malignant.
It’s considered the most severe form of CIN before cancer develops.
CIN 3 also involves a larger portion of the cervical lining being affected by the abnormal cells.
What is the “CIN” in CIN?
• It stands for cervical intraepithelial neoplasia.
• CIN may also be referred to as dysplasia, which means cellular overgrowth.
• CIN 3 or III is a high-grade dysplasia — higher than the more moderate grade of II, which is more progressed than the mild form of I.
 Dr. Bartos served as an assistant clinical professor of OBGYN at the Uniformed Services University of Health Sciences for several years and was a physician in the U.S. Navy for eight years.
Dr. Bartos served as an assistant clinical professor of OBGYN at the Uniformed Services University of Health Sciences for several years and was a physician in the U.S. Navy for eight years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Cause of Jaw Muscle Twitching Can Be Teeth Cleaning

A twitching jaw muscle can have several causes and one of them is cleaning the teeth. (more…)
Can TMJ Disorder Cause Eye Socket Pain?

Eye socket pain can bring to mind a brain tumor or aneurysm, but temporomandibular joint disorder (“TMJ”) is also a possible cause for pain that seems to be originating from within the eye.
“Pain from TMJ disorders can be experienced in different part/s of the face and neck, and it is not uncommon for patients to experience isolated pain in regions of the eye or ears and no pain in the TM joint region (despite it being TMJ disorders),” says Brijesh Chandwani, DMD, BDS, Diplomate, American Board of Orofacial Pain, with Connecticut & NY TMJ.
“There are a few different mechanisms behind pain being experienced in the region of the eyes,” continues Dr. Chandwani.
“Inflammation in the TMJ region often causes pain in the face of the affected side of the jaw joint including the eye.
“In cases of non-inflammatory disorders of the TMJ (muscle spasm, muscle disorders), pain can be referred from the affected muscle to the eye socket.
“Thirdly, patients often suffer from TMJ disorders and different headache disorders concurrently, and eye socket pain could be the main symptom from the headache disorder.
“Pain in the region of the eye socket could also be referred from the neck muscles.
“Lastly, pain in the eye socket could be due to something scary like a brain tumor also.”
What you should do is see your regular doctor for an initial evaluation, though seeing a neurologist before any other kind of doctor can also set your mind at ease.
Your primary care physician may refer you to an ophthalmologist and/or neurologist, but is not likely to suspect TMJ disorder if your only symptom is eye socket pain and even other head discomfort with it.
If an MRI or CT scan of the head and neck shows no abnormalities (e.g., a pinched nerve in the neck can also cause pain that seems to be emanating from the eye socket), you’ll want to get an exam by your dentist.
Like Dr. Chandwani pointed out, TMJ disorder doesn’t always present with the more publicized problems of this common ailment such as a clicking jaw, inability to open the mouth all the way and discomfort chewing food.
“If you are suffering from eye socket pain, primary physician should be contacted right away,” says Dr. Chandwani.

Dr. Chandwani has 15+ years of experience focusing on TMJ disorders and sleep disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Can a 17 Year Old Get Breast Cancer? Yes.
It’s fair to be point-blank: A girl of 17 years CAN get breast cancer. It has happened.
But there’s something that teen girls need to be very aware of when it comes to breast cancer. (more…)