How Low Must Ejection Fraction Be for Congestive Heart Failure?
Find out what the cut-off point is for when ejection fraction could be low enough to mean congestive heart failure.
People with congestive heart failure have a low ejection fraction, but does a low ejection fraction always mean congestive heart failure? How low is too low?
“The cut-off point where we would start to worry about why the patient’s heart function is being affected is usually below 50%,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
The ejection fraction simply refers to how much blood the heart pumps with each beat.
The percentage means what percent of the blood, that’s in the heart’s chambers, gets pumped out.
A cardiologist may explain this to a patient in terms of how much of a “squeeze” that the heart has with each beat.
EF is determined for the left ventricle and also for the right: two different figures.
“A normal EF is usually 55-60% or 60-65%, and an EF from 50-55% is generally considered low normal,” says Dr. Sayeed.
“We wouldn’t necessarily call it CHF (congestive heart failure) if the EF was below 50% unless they were having signs and symptoms of CHF like shortness of breath, unable to sleep flat, waking up at night with shortness of breath, or leg swelling, etc., but would call it a depressed EF,” continues Dr. Sayeed.
This can be a little tricky, though, if the patient is of advanced age and never exercises.
They may complain of shortness of breath after pushing a shopping cart full of groceries across a parking lot, loading the car’s trunk, then pushing the cart back.
Chances are, an 80-year-old is going to be short of breath after this.
Does this mean they automatically have congestive heart failure if their ejection fraction is under 50 percent, even as low as 35 percent?
The cardiologist needs to find out if there are other suspicious symptoms and what can explain those symptoms.
Did they have relatively recent coronary bypass surgery and recover fully from it, which might rule out heart disease causing symptoms?
Is an echocardiogram normal? Is a chest X-ray normal?
If yes to all these (and no other symptoms), the patient is most likely short of breath from exertion combined with old age and lack of aerobic exercise.
Athletes exist who have a low ejection fraction.
“An athlete could have a low EF if he had a known cardiomyopathy of some sort, but was able to train himself back to a high endurance level,” says Dr. Sayeed.
“This would be fairly uncommon, as most individuals with a low EF would not be able to be very athletic due to symptoms, unless they were very well-compensated and could deal with the low EF.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/designer491
Overcome Your Fear of Twitching Muscles Once and for All!
Overcome Your Fear of Twitching Muscles Once and for All!
Here is the sequence of events:
1) You notice a muscle twitching and it won’t stop. It may be under your leg while you’re sitting; on the arch of your foot; a whole toe; a whole finger; below your lower lip; in the chest, torso, upper arm, shoulder…it’s just twitching away.
2) In this day and age of the Internet, you do a search on something like, “Why does my muscle keep twitching?”
3) On the first page of search results are links to ALS sites; you learn that muscle twitching is a well-documented symptom of this merciless, incurable disease.
4) Your “fasciculations” now intensify, becoming more frequent and spreading throughout the body.
So if you first began noticing the twitching in your left lower leg, it’s now spreading up the leg, then to the other leg, and it just seems that your entire body’s muscles are acting up.
5) You now spend hours and hours on the Internet, and every time you find some reassuring information, the next link contradicts the good news that you just read and you’re back at ground zero: fear that you have only two to five years to live.
Scared out of Your Wits About Your Twitching Muscles
“I would say that there is a wealth of knowledge available about neurologic diseases including ways to identify and treat them,” begins Mitzi J. Williams, MD, clinical neurologist with Morehouse School of Medicine and clinical advisor for the Multiple Sclerosis Foundation.
“Because there is so much information available, it can cause one to think that conditions occur more commonly than they do.
“For instance, there are an estimated one million people in the U.S. living with MS — out of an overall population of 325 million people.
“ALS is an even rarer condition and some estimate that there may be 20,000 people living with ALS in the U.S. at any given time.
“Though they have gained recognition through various campaigns to raise awareness and funds for research, they are not at all common diseases.
“Reading and informing yourself about conditions related to your symptoms such as muscle twitching is important, but it is also important to pair that knowledge with medical expertise for diagnosis.
“If you have been seen by a medical professional and have muscle twitching without weakness or other signs of neurologic impairment, it is not likely either of these diseases.”
Below are links to articles that will give you a lot of very helpful information.
I know what it’s like; I’ve been there, and I have made sure that my articles will leave you feeling much more empowered with knowledge—and most likely, with the reassurance you’ve been so desperately seeking.
Where are you twitching?
……………………………………………………………………………………………..
Muscle Twitching F.A.Q.
The areas where a twitching muscle is most likely to be visible include the eyelid, an entire finger or toe, the quadriceps area and the chest region. Why you see some fascics and is this worrisome?
Sometimes a muscle twitch looks more like something under the skin making it jump. Here is what that means.
Another name for harmless muscle twitching is benign fasciculations. If you’re suffering from a lot of this, the cause may be anxiety.
As you inspect the front of your legs for any signs of atrophy (which may be a symptom of a neurological disease), you may spot a dent or groove that you swear was never there before. There is a benign explanation,
Do you exercise a lot or hard? Lengthy aerobics sessions, or vigorous cardio activity and even strength training, can cause muscles to twitch afterwards. A doctor explains why in this article.

Dr. Williams is author of “MS Made Simple: The Essential Guide to Understanding Your Multiple Sclerosis Diagnosis,” available on Amazon. She is a member of the American Academy of Neurology.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
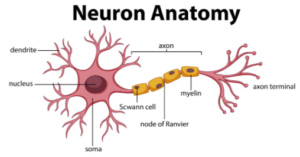
Image of neuron: vecteezy.com
ALS Tongue Twitching, Weakness, EMG Test
Why can’t ALS patients feel their tongue twitching?
Did you know that if you can feel your tongue twitching, this is not a symptom of ALS?
That’s because people with this neurological disease cannot, ever, feel their tongue twitching. Learn more about this.
What ALS tongue twitching really looks like
When you realize what this actually looks like, you’ll probably be overcome with a ton of relief, because, though the tongue in general is “icky” to look at, the twitching tongue of someone with ALS is in a league of its own. Read more…
How to tell the difference between perceived weakness and ALS weakness.
I once read of a man who couldn’t help wonder if he had ALS, even though he was bench pressing 500 pounds.
Though the weakness has to begin from some point, there actually are big differences between benign weakness that one might experience from stress, fatigue or overactive imagination, and pathological weakness. Learn more.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/pathdoc
Why Muscles Seem to Twitch More When at Rest

Find out why your muscles begin twitching while at rest, but stop when you move.
One day I sat at my computer and began noticing that my leg muscles were twitching all over.
Not much sooner, I had completed a two hour power hike and trail run, during which I perceived no twitching.
If I moved my knees in and out, or repeatedly went up and down on the balls of my feet, the twitching ceased. Or did it?
I’ve had twitching (fasciculations), but never while I was moving that muscle group. Or so it seemed.
“Benign twitches are more prominent when the muscle is at rest for two major reasons,” begins Anthony P. Geraci, MD, associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
“First, if we are at rest—sitting or lying down—we are more likely to notice a twitch.
“Second, even when we think we are perfectly still, our nerves and muscles are very busy keeping us still.
“We have a feedback loop between the muscles and spine that keeps our posture steady, etc.
“Our agonist and antagonist muscles are always in a state of balance.
“For example, when we move our biceps, the triceps receives signals from the spine to inhibit it from contracting and fighting against the bicep.
“This phenomenon occurs constantly and the inhibitory signals keep the muscle membranes stable.”
So if you’re at your computer in a seemingly immobile state, your muscle fibers aren’t exactly inert.
There’s still activity going on.
Think of them as being on standby for more prominent movement such as shifting position in your chair.
And of course, it makes a lot of sense that you wouldn’t feel twitching while you’re walking, cleaning the house or exercising.
The fact that muscles “seem” to twitch only while at rest in NO way points to a possible disease process.
There is nothing intrinsic about rest that suggests a pathology.
So go ahead, get in your favorite chair and relax!
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sudden Onset Transient Double Vision: Get to ER

Just because your sudden-onset double vision disappeared after a few minutes doesn’t mean that the cause can’t kill you.
There are many causes of double vision (diplopia), but sudden-onset, transient double vision is a different animal and almost always points to an underlying, very serious problem.
For example, this is a possible symptom of a mini stroke (TIA: transient ischemic attack).
And though sudden-onset transient double vision may have a not-so-serious cause, such as something wrong with the eye rather than the brain, this doesn’t mean you should blow this off and pretend nothing happened just because everything returned to normal after a few minutes.
Get to the Emergency Room
A physician will administer the appropriate tests to see what may have caused this troubling symptom. NEVER think, “Oh, I’ll be fine; it’s gone now.”
Thinking like this could COST YOU. A transient ischemic attack is a warning sign that a massive stroke could be lurking just around the bend.
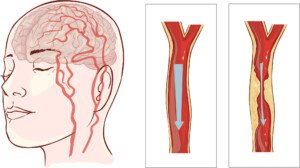
Blood flow in the brain is cut off in an ischemic stroke. Shutterstock/corbac40
Other possible causes of sudden-onset transient double vision are an actual stroke, diabetes and trauma to the head.
The ER doctor will start by taking a detailed medical history and performing a physical exam.
A neurological exam is usually next, as double vision can be linked to neurological issues – such as a TIA.
This involves checking your eye movements, reflexes and muscle strength.
Vision tests are also conducted to understand the nature of the double vision.
These tests might include tracking your eye movements and measuring how well your eyes focus and align.
Blood tests can help identify issues such as diabetes, thyroid problems or infections that could be affecting your vision.
If the initial tests suggest a more serious problem, imaging studies like a CT scan or MRI of the brain might be performed to check for tumors, bleeding or other abnormalities.
“If the symptom is truly double vision and the other causes you list are ruled out, then in otherwise healthy people a consideration would be myasthenia gravis,” says Anthony P. Geraci, MD, associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
“There is a simple blood test to check for this and one should see a neurologist to investigate this possibility.
“Myasthenia gravis is a condition which causes muscle weakness transiently. It can often be limited to muscles of the eyes.”
I’ll say it again: If your symptom lasted only a few minutes and you felt “fine” after that point, as though nothing happened, do not be tricked by this.
- A mini stroke, by definition, is transient.
- The next blood clot could be a full-blown stroke and permanently cripple you, if not kill you.
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Erica Danger
Numbness in Tip of Middle Finger: Cause & Solution
If the tip of your middle finger has suddenly become numb, here is some reassuring news.
It’s hard to ignore numbness in the tip of your middle finger.
However, the extreme locality of this should be a tip-off (no pun intended) that it’s benign and not a sign of MS or some other neurological disease.
I was inspired to write this article after I developed numbness in the tip of my middle finger.
It didn’t take long for me to connect the dots, though at first, I was stumped.
The day prior, I had placed a lot of pressure on it while doing bench dips at the gym with a lot of weight on my lap.
Below is what this exercise looks like.

Note the man’s left hand. Imagine the pressure against his middle finger as he pushes up.
When pushing up during this exercise against heavy resistance, one cannot help but press the middle fingertip really hard against the underside of the bench.
It’s nearly impossible not to do this. So how, then, might this cause numbness?
“There are two nerve branches that run along either side of our fingers,” says Anthony P. Geraci, MD, associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
“Numbness can occur with prolonged pressing or pressure against these small nerves, due to transient damage to the nerve.
“The medical term for it is ‘meralgia digitalgia.’”
In a neurological disease, numbness would not be in such a tiny, pinpointed area in the absence of other symptoms.
If you have numbness in your middle fingertip, think very carefully what you’ve done earlier that day or the day before.
I did, and at first, it didn’t come to me what I might have done to put pressure on it. Then I remembered the dips.
The fact that numbness is in only one finger and not the same finger in the other hand, in no way points to a disease!
It’s quite common to exert force unequally when exercising under a heavy load.
What happens in meralgia digitalgia is that the pressure (in my case, pressure against the underside of the bench) compresses the nerve that supplies sensation to the skin surface of the fingertip.
In my case it took two or three days for the nerve to decompress and full sensation to return.
There is no need for treatment other than patience.
It’s worthwhile to note that carpal tunnel syndrome can also cause numbness in the middle fingertip (my mother experienced this in both hands).
However, there will be other symptoms with carpal tunnel syndrome.
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Seasontime
Can Cause of Numb Lips Be Serious Like ALS?

As innocent as a numb lip may sound, some causes can be quite serious–can one be ALS?
There are a number of causes for numbness in a lip, says Anthony P. Geraci, MD, associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
Dr. Geraci further explains, “Have to be careful here, as some of the causes can be signs of serious problems.
“I have to be sure to inform your readers that if they have these symptoms they should see a neurologist or their medical doctor.”
Before you panic, though, review your recent history to see if there could be a benign explanation.
Were you just out in the freezing cold?
Did you accidentally bite your lip recently?
Did you have dental work earlier and the Novocain has not completely worn off?
Sometimes the lip gets very numb from this anesthetic and it can last quite a while after the procedure.
Dr. Geraci continues, “One of the more common and benign causes is due to hyperventilation.
“During heavy breathing while exercising or during anxiety, carbon dioxide becomes decreased in the blood and this cause metabolic changes in the blood that are sensed by the nerve endings–lips, finger tips and toes.”
Serious Causes of Lip Numbness
One can be a TIA: transient ischemic attack. This is a “mini stroke” or blood clot that causes temporary symptoms.
If you suspect a TIA, get to the ER immediately, as a TIA is a harbinger of a full-blown stroke (30 percent of people who have a TIA have a stroke within one year).
However, if numbness in your lip is caused by a TIA, you’ll have other symptoms with it (one or more of the following: slurred speech, facial numbness or paralysis, confusion, visual disturbance, one side of body suddenly weak, numb, heavy or paralyzed).
Another possible cause is multiple sclerosis.
If you have a numb lip from MS, you probably have some other symptoms as well (e.g. muscle spasms, balance problems, fatigue, slurred speech and vision problems).
ALS does not cause lip numbness.
Some Other Causes of Lip Numbness
- leprosy
- seafood poisoning
- trigeminal neuralgia (facial nerve irritation; cause is sometimes unknown, but may be from the nerve coming in contact with a blood vessel, MS, aging, and rarely, a tumor; trigeminal neuralgia is also accompanied by facial pain)
- shingles
- arterial spasms (Reynaud’s disease)
- low blood sugar
- mineral deficiencies
- cosmetic/soap allergies and food allergies.
That’s a LOT of potential causes for numbness in the lip. However, if all you have is a numb lip, and NO other symptoms, chances are not likely that you have anything serious.
This statement, however, is not absolute, and if your lip numbness persists, see a doctor.
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
What Causes INTERMITTENT Muscle Twitching?

This article is about the causes of intermittent muscle twitching (fasciculations), not spasms.
Intermittent muscle twitching (fasciculations) is not the same phenomenon as spasms.
If you’re wondering what can be causing intermittent twitching of your muscles, here is what Dr. Anthony P. Geraci, a neurologist, says:
“This is a short answer: Benign muscle twitches are due to unstable muscle fiber membranes, usually due to injury (as when we work out). The twitching is simply a random phenomenon.”
Dr. Geraci is associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
Thus, the intermittency, in and of itself, is no cause for concern.
And don’t let the term “injury” scare you.
Every time you exercise, you injure muscle fiber membranes.
They then repair themselves, and this is one way that exercise makes you stronger.
This injury is especially caused from intense weightlifting.
Benign fasciculations come in all sorts of flavors, shapes and colors, in that they can be occasional, intermittent for a few days or weeks, intermittent for many months, ongoing for a few days, and even ongoing for much longer periods of time.
Benign fascics can also occur in response to specific activities such as hiking, using the revolving staircase, chin-ups or bench pressing.
Thus, their occurrence is contingent on how often you do these triggering activities.
Other benign causes of common muscle twitching are fatigue, emotional stress or anxiety, and mineral deficiencies.
If you have fasciculations and no noticeable weakness or other concerning symptoms like slurred speech or falling seemingly for no reason — chances are pretty high that you do not have a neurological disease (i.e., despite the fascics, you can still knock off pushups, run up and down stairs, be on your feet all day at work without a hitch, etc.).
Note, however, that “benign fasciculation syndrome” typically comes with some cramping and/or exercise intolerance, though it is not progressive or capable of causing damage to your neuromuscular system.
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
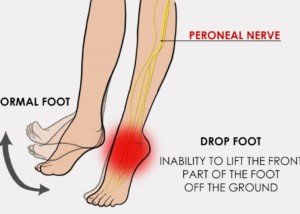
Strength Tests for Foot Drop, Quads, Calves, Fingers

Strength Tests for Foot Drop, Quads, Calves, Fingers
As a former personal trainer, I have designed some brilliant strength tests that should give any healthy person loads of reassurance that they are healthy.
Of course, always consult with a neurologist for a medical evaluation if you’re experiencing troubling symptoms.
But in the meantime, try out these strength tests if your “hot areas” are the foot, quads, calves and/or fingers.
Strength tests can be a fabulous way of giving you the very reassurance that you so desperately need to feel that you’re healthy — that everything’s going to be just fine!
Strength Tests for the Following
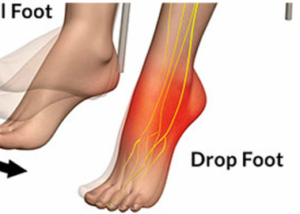
Think you have foot drop? Foot drop is literally that: a dropped foot — due to the inability of the muscles to hold it up.
This is evident when walking. The affected foot will feel as though it’s dragging or limp, or not as perky as it used to be.

An ankle-foot orthotic (AFO) for true foot drop. Source: Foot drop Pagemaker787 CreativeCommons
Many conditions, including ALS, cause foot drop. However, there are strength tests that, if you can pull them off, will be mighty reassuring that your motor neurons are just fine. Check them out: Foot Drop
Some people with health anxiety have taken to focusing on their quad muscles or entire upper leg.
There are strength tests that target the quadriceps muscles, and if these muscles are weak due to a motor neuron disease, you will not be able to conduct these drills without knowing that something is very wrong. So check them out. Quads
Another hot area of focus among those with health anxiety is the lower leg or calves. I have some dandy strength tests for those.
Fingers and/or the entire hand are also a common area of focus.
It is so easy to see if your fingers are truly suffering from clinical weakness by conducting some straightforward strength tests. Here they are. Fingers
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Why Don’t Websites Say ALS Tongue Twitching Can’t Be Felt?

Those who fear ALS would benefit by knowing that bulbar-onset tongue twitching cannot be felt by the patient.
Bulbar-onset ALS tongue twitching cannot be felt by the patient, but are there web sites that make note of this?
How does one discover or come to the conclusion that their tongue is twitching?
Sometimes they just happen to see what appears to be a twitch when maybe applying lipstick or flossing their teeth.
Being that few people have a habit of looking at their tongue in the absence of any perceived worrisome or annoying symptoms, perhaps we should conclude that most people who report tongue twitching initially began feeling something that they concluded were fasciculations.
When a person hunts enough on the Internet for information pertaining to tongue twitching, they will come across a lot of instances in which “tongue twitching” and bulbar-onset ALS are in the same sentence.
Mayo Clinic even lists twitching of the tongue as a symptom of ALS.
Why don’t any of these sites point out that bulbar-onset fasculations CANNOT BE FELT?
I posed this question to Anthony P. Geraci, MD, associate professor of neurology at Donald & Barbara Zucker School of Medicine in New York.
Dr. Geraci says, “I am not surprised that medical sites never point this out: It is a huge complaint I have with the medical profession; they always write about disease and symptoms from THEIR point of view and not the patient’s experience.”
 Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
Dr. Geraci is also the director of neuromuscular medicine at Northwell Health in New York.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.