Sudden Brief Extreme Dizziness in Younger Adults: Causes, Solutions

A doctor discusses possible causes of sudden, extreme and brief dizziness in younger people. And solutions.
There are MANY causes of sudden, brief episodes of severe dizziness in people who do not have any conditions that can cause this — that is, conditions that are strongly associated with elderly age.
“Most common ones include abnormal heart rhythms, neck, muscle spasms, ear infections, drops in blood sugar and mini-strokes,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
A mini-stroke is also known as a transient ischemic attack. Though elderly age is a big risk factor, middle-aged people and even younger adults can experience a TIA, though in younger adults, this is rare.
A TIA can cause many symptoms, and though a sudden and brief episode of severe dizziness is one of them, it’s not one of the more common symptoms of a mini-stroke.
In fact, if you’re middle aged and especially younger, and you’ve been experiencing sudden-onset dizziness with no other symptoms, this is unlikely to be a TIA, but a checkup with a neurologist would be a smart idea.
Middle Ear Problem As Cause of Sudden-Onset Severe Dizziness
Dr. Teitelbaum says, “A key discriminating factor? Do they have vertigo where it feels like they or the room are actually spinning around in a circle?
“If yes, this points to a middle ear problem. Also, do they pass out without warning? This suggests an abnormal heart rhythm.”
Side effects from medications (especially narcotics), and pregnancy, can cause a bout of sudden intense dizziness.
There are different kinds of “dizziness.” One such type is called orthostatic hypotension.
Do you get your symptom only right after you suddenly stand after having been seated for a while?
If so, rise slowly from your seat and when you’re halfway up, pause for 15 seconds, then resume rising to an erect position slowly.
This will prevent a sudden drop in blood pressure, which can cause acute dizziness and even blacking out in some individuals.
BPPV
Benign paroxysmal positional vertigo (BPPV) is a common inner ear disorder that triggers sudden, short (or long) episodes of dizziness or a spinning sensation.
It can certainly occur in young adults and people of all ages.
It occurs when tiny calcium crystals, called otoconia, become dislodged from their usual position in the utricle of the inner ear and move into the semicircular canals of the inner ear.
These canals help detect head motion. When the crystals shift with certain head movements, they send false signals to the brain, conflicting with normal balance input.
This mismatch can cause abrupt vertigo lasting briefly in some cases, often brought on by rolling or sitting up in bed, looking up or sideways, or bending over.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
Are You Rude Due to Your Hearing Loss?

If you have hearing loss, here’s why people get irritated when you ask them to repeat or why they say “Never mind, it’s not important.”
Many people with hearing loss, impairment, who are hard of hearing, etc., report that many individuals get irritated or become rude when asked to repeat something or speak louder.
I’ve seen this situation come up in advice columns: A hearing impaired individual writes in to complain that, so often, people become irate and impatient when that individual asks them to talk slower, louder or to repeat what they just said.
One such woman with hearing loss said it was hurtful when people would respond, “Never mind, it’s not important,” when she asked them to repeat their statement or question.
To all such men and women with hearing loss who have experienced rudeness or exasperation from people, I have a question for you:
HOW do you ask people to speak louder, slower or repeat things?
Take a good look in the mirror and honestly answer this very fair question.
I know people with hearing loss. I can’t begin to tell you how many times I’ve witnessed one of them, a woman I’ll call “Linda,” respond rudely to a speaker when she couldn’t understand them!
She’ll typically deliver a curt “What?!” with an anguished face when she can’t understand what was just spoken to her.
This makes the speaker think that Linda blames THEM for why she didn’t hear them clearly!
Think about it: You’re talking to someone (and, in this hypothetical scenario, you can hear perfectly). That person reacts with an exasperated “What?!” and looks miffed.
How would this make you feel? Would you want to kindly, patiently repeat yourself?
Or would you be totally put off and decide to end the interaction with a “Never mind, it’s not important”?
People do not want to feel as though the hard of hearing listener blames them for why they can’t understand their speech.
Speakers who are made to feel that the listener blames them for “mumbling” or talking unclearly will find this very offensive and rude.
Granted, some people DO mumble and talk unclearly, but let’s face it: Most people do not have this problem.
I know I don’t. In fact, I’ve been told I sometimes talk too loud. As a person who communicates (writing) for a living, I place a high premium on the importance of clear speech. I don’t drink or take drugs; my speech is very clear.
One time I had a phone job. I called someone and began speaking. The cranky man interrupted with a blunt, angry “Speak up! I can’t hear you!”
Well, I didn’t speak up; I HUNG up. I’m sure he thought I was rude!
Had he interrupted with a kindly “Excuse me, but can you repeat that and talk a bit slower and more careful? I’m having trouble hearing you,” I would have kindly obliged.
I know a relative with hearing loss who wears hearing aids, but he often gets irate with me if he doesn’t understand me. He accuses me of “running my words together.”
If you have difficulty with hearing, have you ever accused the speaker of “mumbling” or talking too fast?
This is VERY insulting and provides NO incentive for the speaker to be kind and patient with you.
If you think only children mumble, realize that kids’ voices have higher frequencies, and that’s why you have more difficulty deciphering kids’ speech.
Linda thinks nowadays, everyone on the phone who leaves messages “can’t talk clearly.”
The man with hearing aids I mentioned believes that “today’s movies have poor sound quality,” that the actors don’t speak loud enough and mumble.
He also thinks that “young people don’t know how to leave clear phone messages.”
You’re pretty much guaranteed a kind, thoughtful, patient response from the speaker to repeat or talk slower if you do your part:
Be gracious when asking someone to repeat their question or statement, without implying that they can’t talk clearly.
Don’t be curt just because the speaker is a teenager or child, either. And remember, children emit higher frequencies.

Shutterstock/locrifa
I’ve witnessed Linda outright tell people on the phone that they need to speak more clearly; her tone of voice and choice of words clearly tell the talker that she blames THEM.
Often, when a person finally suggests that the listener might have hearing loss or that they should get their ears checked, they typically insist, “Nothing’s wrong with my hearing.”
If you think these suggestions are rude, why is there a double standard when it comes to visual impairment?
If someone’s squinting to read a sign, and their buddy says, “Hey man, when’s the last time you had an eye exam?” few people would consider this rude.
If you saw someone struggling to read fine print, you’d be apt to say, “Maybe you should see an optometrist,” without ever considering this might be rude.
You’d especially suggest an eye exam if you witnessed a friend or family member often bumping into edges of furniture.
So why is it rude to recommend someone get their hearing checked? Why is it rude to tell someone, “I believe you have hearing loss,” but not, “I think you have nearsightedness”?
If you’re hard of hearing and are fed up with being treated with impatience, being dismissed or being reacted to in a rude way when you ask the talker to adjust their speech, I urge you to re-evaluate how you respond to people when you don’t understand what they’re saying.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, katemangostar
Tiny Red Spots in Toilet after BM or Urine: Unlikely Origin
Have you noticed tiny red dots against the toilet bowl after a bowel movement or urine output and wondered what’s wrong?
Imagine turning towards the toilet to look inside after having a bowel movement or releasing some urine, and on the inner portion of the toilet bowl you see a few red dots, spots or specks.
This will make you think you just released some blood. And that may very well be the case — until you use a tissue to wipe at the red spots to get a closer look—and realize that they won’t come off the porcelain.
This is what happened to me. At the gym I stood to wipe myself after urinating, and noticed two dark red tiny spots against the part of the toilet that’s under the water. They looked like little droplets of blood.
Toilet paper in hand, I wiped at one so that I could examine it on the paper. It didn’t budge; it didn’t even smear.
Blood that just come out of me would have easily transferred to the tissue paper.
I flushed the toilet. The tiny red spot, and the other one, remained in place, not budging or breaking up. I flushed the toilet again and they remained fixed on the porcelain.
Conclusion
They were there before I entered the stall and had nothing to do with my body.
Specks of blood coming out of your anus, urethra or vagina will not firmly plant themselves against porcelain like tiny specks of paint will.
They’ll come right off with tissue paper and smear on it.
So next time you use a toilet, make sure it’s free of paper and get a good look at the porcelain to see if there are any pre-existing red specks or anything else that might fool you into thinking it’s your blood or other worrisome discharge.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
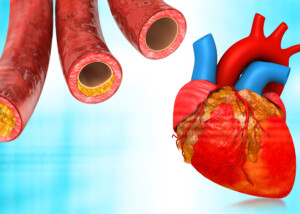
Zero Calcium Score in Asymptomatic vs. Symptomatic Patients
A zero calcium score is NOT an accurate predictor of cardiac events in patients with symptoms, but for those without symptoms, it’s over 95 percent.
A group of people with symptoms like chest pain and shortness of breath upon exertion undergo coronary calcium scoring and just happen to all get a result of zero, while a second group (equal number of people) with NO symptoms also undergoes the test, with a result of zero.
Does the calcium score of zero mean the same for both groups? NO.
“No medical test is perfect,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“Every medical test is based on probabilities. Bayesian Theory, which takes into account pretest probability of disease in the interpretation of the results, must be applied.
“How likely is the patient to have the disease you are looking for – must be considered in interpreting any test result.”
It’s possible for a person with a moderate to high probability of heart disease to have a calcium score of zero, even though these patients usually (which doesn’t mean always) have high calcium scores.
Likewise, those with low pretest probability of heart disease will “likely,” says Dr. Reynolds, have a low calcium score—but not all will.
Comparing Asymptomatic Patients’ Zero Calcium Score with that of Symptomatic Patients
Dr. Reynolds points out a 2006 American Heart Association study of patients without symptoms who had a zero calcium score.
The zero calcium score “was associated with a very low risk for plaque (negative predictive valve 95-99%) and low cardiac event rate for the next five years (0.1 per 100 person-years),” she explains.
“However, in a 2008 study in Circulation in which symptomatic patients were studied, a zero calcium score was not nearly as predictive of good outcomes.”
This doesn’t mean that every single person with chest pain and/or shortness of breath, who has a zero calcium score, falls into the category of the collective result of the 2008 Circulation study.
One explanation is that in a group of “symptomatic” people, some will surely have non-cardiac origin of their symptoms.
“Bottom line – calcium scores are NOT definitive enough to use as diagnostic tool – which is why the professional medical associations do not recommend them as routine screening tests – which is why the insurance companies won’t cover the expense,” says Dr. Reynolds.
“If a patient is low-risk and asymptomatic, there is no conundrum – just relax and stick to a healthy lifestyle and diet. There is no need for a calcium score or a CT angiogram!”
Summary of Comparison of Asymptomatic and Symptomatic People with Zero Calcium Score
“In patients with no or minimal risk factors and no symptoms, a CAC of zero has a great negative predictive value of disease.
“In patients with multiple cardiac risk factors and/or symptoms to suggest coronary disease, a CAC is an INAPPROPRIATE TEST, as the negative predictive value is not helpful.”
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
sscpywrt26
Trouble Breathing During or After Exercise, No Chest Pain
Find out a most unlikely cause of difficulty breathing IN during or after exercise in the absence of chest pain in an otherwise healthy person.
Suppose you just had your heart checked and everything’s normal, but you have sudden-onset difficulty breathing IN during or right after exercise (or any other time of the day, for that matter), and there’s no chest pain.
What might this be?
You may want to pay a visit to an otolaryngologist (ear, nose and throat doctor), because a condition called laryngopharyngeal reflux can obstruct breathing, says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Sudden or gradual voice changes, choking symptoms, coughing and shortness of breath are usually symptoms of laryngopharyngeal reflux or LPR,” says Dr. Silvers.
This condition can be misdiagnosed as exercise-induced asthma, even though, as Dr. Silvers explains, difficulty inhaling is not a symptom of asthma. In asthma, the breathing difficulty pertains to exhaling.
This condition can be misdiagnosed as exercise-induced asthma, even though, as Dr. Silvers explains, difficulty inhaling is not a symptom of asthma. In asthma, the breathing difficulty pertains to exhaling.
“LPR happens when acid reflux gets up to the level of the larynx,” she continues.
“The result of this acid is swelling at the back of the vocal cords. This swelling keeps the vocal cords from coming together properly and leads to hoarseness.
“The swelling creates a structural blockage and can make is hard to take a deep breath.”
When LPR comes on, you may have only one of its symptoms, such as difficulty breathing in, which can be quite alarming if this occurs right as you’re catching your breath after wind sprints across a gymnasium.
If trouble breathing strikes while catching your breath after a burst of exercise, you won’t be very motivated to speak to check if your voice is hoarse; you’ll be too busy struggling to inhale.
By the time the episode (which may be very brief) is over, your voice may sound normal.
“The swelling can tickle the vocal cords and cause a dry cough,” continues Dr. Silvers.
“And this swelling can give you the sensation of a lump in the throat and occasionally difficulty with swallowing.”
Diagnosis of Laryngopharyngeal Reflux
“All of these mentioned symptoms do not have to be present to make a diagnosis of LPR.
“A physical exam by an otolaryngologist can confirm this diagnosis with an examination of the larynx.
“This is a common problem with people of all ages. Even young healthy people can develop LPR during stressful periods, eating a poor diet, even during exercise. The symptoms of LPR can be constant or come and go.”
If you experience trouble breathing during or after exercise, especially if there’s chest pain, consult with a physician to rule out a more dangerous cause.
LPR is benign (though if left untreated, it can lead to esophageal cancer).
Keep in mind that trouble breathing from a heart problem isn’t always accompanied by chest pain.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Realstock
Sudden Difficulty Breathing Right After Cardio Exercise

Sudden difficulty taking breaths immediately after a cardio stint isn’t always exercise-induced asthma.
Symptoms of vocal cord dysfunction and exercise-induced asthma are nearly identical.
Symptoms between these two are so alike, in fact, that many athletes or workout enthusiasts are misdiagnosed with exercise-induced asthma, when in fact, they’ve been having bouts of vocal cord disorder.
However, this doesn’t mean you can’t, by coincidence, have BOTH conditions—which makes proper diagnosis even more tricky.
The misdiagnosis leads to inappropriate, and therefore ineffective, treatment, say researchers from Ohio State University Wexner Medical Center.
Vocal cord dysfunction goes by several different names, including paradoxical vocal cord fold motion disorder (PVFMD).
Asthma inhalers are useless for this condition, which is managed by several approaches such as Botox injections, biofeedback and vocal cord retraining therapy.
Vocal cord disorder can occur during or right after exercise, but can be triggered also by emotional stress.
It can be caused by environmental irritants that one gulps in during the heavy breathing of exercise.
The vocal cords constrict and obstruct the air flow to the lungs, making inhalation labored.
Another symptom of vocal cord dysfunction, besides difficulty breathing in, is coughing—not necessarily a hacking type of cough.
It can be a sudden cough, like something is suddenly deep in the throat. The cough may immediately precipitate the trouble breathing.
Thirty percent of the Wexner study group reported coughing during exercise.
However, vocal cord dysfunction that produces coughing doesn’t always produce the trouble inhaling.
Diagnosis of vocal cord dysfunction, post-exercise, can be made with a flexible fiberoptic laryngoscope.
Vocal cord disorder and exercise-induced asthma both can cause a whistling or “respiratory sound” upon inhaling, and diagnosis cannot be made based on what the “wheezing” of one condition sounds like compared to the other.
“PVFMD symptoms can often mimic asthma,” says Anna Marcinow, MD, study co-author.
She adds that up to “40 percent of people with asthma also have PVFMD — so it’s typical for an athlete to get the asthma diagnosed correctly, but not the vocal cord dysfunction.”
Though frightening, vocal cord dysfunction will not typically cause a person to pass out or suffocate.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/ nd3000
Source: sciencedaily.com/releases/2013/04/130412192400.htm
Can a Class 2 Heart Murmur Go Away on Its Own?

Have you been diagnosed with a class II heart murmur and are scared?
In June 2011 a cardiologist told me I had a class II heart murmur on inspiration (inhaling).
It was not something he brushed aside and he wanted to find out what was causing it.
The reason I was seeing a cardiologist in the first place was for a routine heart disease screening, and to also discuss results of my calcium score test (zero).
The stethoscope picked up the class II heart murmur.
A heart murmur is simply a distinct sound that the doctor hears via stethoscope.
Many are benign, but some can signal a condition. My subsequent echocardiogram was normal.
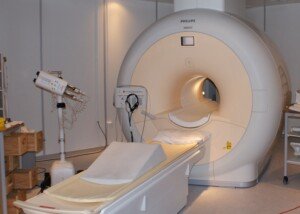
I then had a magnetic resonance angiogram because my doctor’s colleague suggested the possibility of a congenital pulmonary stenosis.
If it turned out that indeed I had this, then it would have to be “watched,” and I’d have to have periodic imaging to follow it.
I had no symptoms, but my doctor said that as one gets older, their pulmonary stenosis — if they have it — “becomes more relevant.”
The MRA took about an hour. When the MRA result came back normal, the doctor attributed the class II heart murmur to “robust cardiac flow” from my workouts.
Two years later I saw him for another routine checkup (just because you’re symptom-free and are at low risk for coronary artery disease, doesn’t mean you shouldn’t get routine checkups).
The class II heart murmur was GONE. In fact, the doctor said, “You now have the quietest heart murmur in the world.”
He didn’t know why the heart murmur went away. I had not stopped exercising in the preceding two years.
He did not rule out that “white coat syndrome” during the first visit may have caused it.
That’s when a person’s pulse changes due to the anxiety of being examined by a doctor.
Nervous about an MR angiogram?
Relax, there’s nothing to be afraid of.
An MR angiogram of the heart is like taking a detailed picture of your heart’s plumbing to check for any issues like blockages or irregularities.
It also looks at function. This amazing procedure can also detect other issues that are unrelated to the reason you’re undergoing it.
This MR angiogram is something to marvel at, not be nervous about.
Nevertheless, you will be given a squishy ball to hold in one hand that, when squeezed, signals to the technician that you want to exit the MRI machine — should you become claustrophobic.
In the procedure, you will lie down and keep as still as possible while the machine takes the images, which helps doctors see how well your heart and blood vessels are working.
Remember, there is no radiation exposure with an MRI procedure.
On a few occasions you’ll be asked to hold your breath for a brief period.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/lenetstan
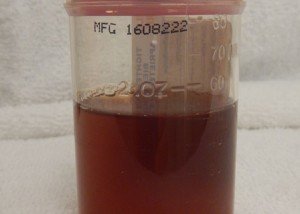
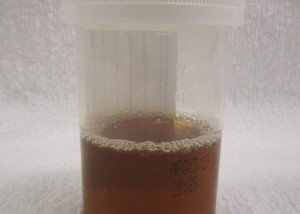
Orange Urine vs. Dark Yellow: Telling the Difference

A proven way to tell the difference between orange urine, yellow-orange and dark yellow.
If you’ve read somewhere that orange urine can be a sign of disease and are wondering if what you’re seeing as orange is actually a dark yellow color, here are tips to better identify the actual color.
You’ll need a clear plastic cup (8-10 ounce) with about a 3.5 inch diameter.
This way, a woman can securely place the rim against her urethral/vaginal area to catch the stream of urine without it splattering anywhere.
While holding the cup firmly in place, relieve yourself. A man, of course, should use this same type of cup to empty his excrement.
Make sure you’ve allowed a good amount of urine to build before excreting it.
This is because only a few ounces of urine may appear darker, or even lighter, than it actually is.
The cup should be at least half full whenever you check the color of your urine; ideally, two-thirds to three-fourths.
Set cup on counter and clean yourself so that you’re not distracted by that aspect. Now, inspect the cup’s contents; here’s how:
Hold it up and look at it. If the urine is an obvious shade of yellow, then it is. You’re done with the test.
However, sometimes it’s hard to tell if what you’re viewing is orange urine, yellowish-orange, light orange, golden-dark yellow or dark yellow.
If you set the cup on the counter — at least if the counter is white, like mine — it will distort the color by making it a darker yellow.
Or, if the actual color of the urine is medium/dark to dark yellow, then the distortion will make it appear yellowish-orange or even deep orange, respectively. Do not be alarmed by this “refraction effect.”
This distortion is very evident with an aerial view of the cup when it’s on the counter.
Do NOT view the color when the cup is on a surface; you must hold it by your fingertips above the rim. Hold it up against a white wall or white door.
Orange vs. Dark Yellow Urine
Document the colors you see. In my case, I noted the following colors:
– Pale-clear
-Pale yellow
-Light yellow
-Medium yellow
-Dark yellow
-Yellow-orange
-Orange-yellow
-Light orange
-Orange

Shutterstock/gritsalak karalak
These colors were noted when I was holding the cup in the air and against a white wall. At the beginning of this experiment, I didn’t like seeing orange urine.
Perhaps you’ve read that a “dark” or “deep” yellow urine indicates dehydration.
However, dehydration, indeed, can cause urine to appear orange. So how can you tell if orange urine is benign or caused by a disease?
I’m not going to tell you that the following technique eliminates the possibility of disease.
What I WILL tell you is that it can reveal a PATTERN — a predictable pattern of varying degrees of color on the pale-clear to orange continuum of urine.
And sometimes, predictable patterns can be very reassuring.
Checking for Patterns
The technique is to track your water intake and exercise times.
If you just sweated up on the treadmill, your urine output after that may be orange from the water loss (dehydration).
A woman who’s having hot flashes especially, while doing cardio, may have orange urine due to the loss of water through perspiration.
After awakening in the morning, you’ll note that urine tends to be dark yellow or maybe even some degree of orange, due to an overnight dehydration process.
If you guzzle a lot of water and soon after urinate, the output likely will NOT reflect the rehydration.
It may take two hours after guzzling water for it to lighten the urine.
So don’t panic if, 90 minutes after drinking two giant glasses of water in 10 minutes, your urine is still orange.
Wait a short while for your bladder to become full again, and chances are, it will be yellow or pale.

For me, 20 ounces of water did the trick every single time.
What seemed like the output for that 20 ounces (not long after drinking it) was actually an output that was already building up in my bladder, from previous dehydration.
I’d simply wait for my next need to relieve myself, and sure enough, the urine was flaxen, a nice pale yellow.
Dark yellow urine is also likely to occur right before bedtime, unless you’ve been drinking up the water all evening.
Note how much water you’ve been drinking, and when you relieve yourself.
For me, one hatch mark indicated one cup of water. If I urinated right after that, I put the color down right below the hatch mark(s).
If I urinated, say, at least an hour later, I skipped a space and put down the color.
So when I reviewed the record, I knew that the skipped space meant that the urination wasn’t immediately after the water intake, but sometime after.
I quickly saw a pattern develop, and was soon able to easily predict the color of my urine.
Juicing fruits and vegetables may not do a good job of rehydrating you — or, at least —will not lighten urine much. Neither will milk.
I found that only WATER does this. Not once did I continue to yield orange urine despite drinking a lot of water. This is always very reassuring.
And by the way, the more dehydrated you are, the stronger your urine’s odor will be due to its concentration.
The concentration is what makes it a dark yellow, or orange.
Is your urine sometimes the color of the sunset below even though you’ve had plenty of water?
Do you occasionally see ssalmon-colored stains on the toilet paper after you wipe?

Here is a likely explanation if a deep amber color is scaring you.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Igor Nikushin
Source: mayoclinic.com/health/urine-color/DS01026/DSECTION=causes
Drinking a Lot of Water but Barely Peeing: Causes, Solutions
Can Angina Come and Go Every Second, Blinking On and Off ?

Do you get chest pain or what feels like angina that comes and goes, literally hurting one second then going away the next, like intervals?
“By definition, angina occurs when the oxygen supply to the myocardium is not adequate to meet the demand,” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“Theoretically, this can occur for a second or so, or it can last hours until ischemia (myocardial strain from oxygen deprivation) becomes infarction (myocardial cell death from prolonged oxygen deprivation),” continues Dr. Reynolds.
“Some patients are very attuned to their symptoms and can differentiate angina from non-cardiac aches. Symptoms will vary. Anything is possible.”
Non-cardiac conditions can cause a chest pain or ache that smarts or comes and goes like a light blinking on and off.
Two such conditions are esophageal spasms and muscle spasms. It’s not well-understood what triggers esophageal spasms, but muscle spasms are usually caused by fatigued muscles from a workout.
These non-cardiac and benign conditions can cause a smarting on-and-off chest pain that’s alarming, and each wave of chest pain may last only a second or so.
Another potential source of a “smarting” type of pain that seems near or in the chest is a gas bubble or fecal matter moving through the GI tract.
Transient irritation of nerves can also cause an intermittent pain in or near the chest.
“Angina usually occurs under emotional or physical stress when the heart is beating faster and harder and needs more oxygenated blood into the coronary arteries, but which cannot be provided by the partially blocked arteries,” explains Dr. Reynolds.
“Angina theoretically can also occur when there is a minor plaque rupture and blood flow is transiently disrupted.”
If you’ve been having chest pain that blinks on and off, lasting only seconds or even one second at a time, especially if you fear angina, get a complete cardiac exam by a cardiologist.
Before you see the doctor, however, it would be wise to document if anything triggers these episodes of smarting chest pain, e.g., do they tend to occur the day after heavy bench pressing?
Does it occur only upon inhalation? This suggests a musculoskeletal cause or possible inflammation of the sac around the lungs. Does the chest pain occur only upon exhalation? This suggests a musculoskeletal cause.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Freepik.com
Angina During Rest but Never from Physical Exertion Possible
There’s a type of angina that can occur at rest but not during exertion.
Maybe you know that “unstable angina” can occur at rest, even during sleep and awaken the patient.
But this type of angina (caused by plaque buildup in the coronary arteries) will also strike when the patient exercises or induces physical exertion such as carrying a heavy box to the car or running up a flight of stairs.
But can angina occur only during rest and not during physical activity?
“There is a syndrome called Prinzmetal’s angina (also called variant angina or vasospasm),” says Monica Reynolds, MD, a cardiologist with ColumbiaDoctors Medical Group in White Plains, NY.
“It is not very common and often hard to document (requires a cardiac cath using provocative agent to induce spasm),” continues Dr. Reynolds.
“It is caused by vasospasm (contraction and narrowing) of the coronary arteries rather than atherosclerosis (plaque buildup). It occurs more in younger women.”
This doesn’t mean older women, or men, are immune to this condition.
“The treatment is slightly different than classic angina – nitrates and calcium channel blockers are usually used (as opposed to beta blockers),” says Dr. Reynolds.
Prinzmetal’s angina increases the risk of heart attack and sudden death, so don’t assume that just because there may not be much plaque buildup, doesn’t mean this condition is necessarily benign.
More About Prinzmetal’s Angina
The coronary artery may be as clear as a whistle, but the spasm reduces its diameter to that comparable to what severe coronary artery disease does.
However, this “variant” angina can also affect someone who already has diseased vessels.
Prinzmetal’s cannot be diagnosed with a treadmill stress test.
The most sensitive test is an IV administration of ergonovine at specific intervals. If a spasm results, this will show on a concurrent EKG.
When a coronary artery narrows either due to plaque buildup or a vasospasm, the body doesn’t know the difference — in that angina will result, even during rest.
 Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
Since 1992 Dr. Reynolds has practiced clinical cardiology at ColumbiaDoctors Medical Group, one of the largest multi-specialty practices in New York State.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.