Why You Suddenly Can’t Breathe for a Few Seconds

Do you have spells of “I can’t breathe!” that last maybe five or seven seconds?
Instead of allowing this to scare the pants off of you, see a doctor to get to the bottom of this frightening symptom.
My mother was having sporadic incidents in which she’d report, “I can’t breathe.”
Of course, she was able to breathe but said it was difficult.
She was not panting, winded or out of breath as one might be after running up a few flights of stairs.
The trouble breathing would last, as my mother said, “seconds,” and had no apparent trigger, frequently occurring when she was seated, or standing passively. Exertion did not bring it on.
If all your tests “come back normal,” it’s likely that the reason you have very brief episodes of difficulty breathing is anxiety related or a panic attack, even though right before the brief episode of breathing trouble, you weren’t thinking of anything worrisome.
Breathing Problems from a Panic Attack
“Panic attacks can cause a change in one’s ability to breathe,” says Walter Gaman, MD, FABFM, board certified in family medicine and the author of several award-winning books including “Age to Perfection: How to Thrive to 100, Happy, Healthy, and Wise.”
“Holding breath or gulping for air can be a sign of other conditions, but when all other medical tests are within normal limits, a panic attack should be considered,” continues Dr. Gaman.
“Stress and anxiety are real and panic is caused by an over-stimulation of the fight or flight response within the body.”
My mother has congestive heart failure and an ejection fraction of 25 percent, but her cardiac nurse was more interested in the idea that fluid buildup (from the CHF) was causing the episodes of I can’t breathe.
“An older patient who has a known heart failure may experience an inability to breathe,” says Dr. Gaman.
“If the chest X-ray is normal, showing no fluid or enlargement of the heart, the shortness of breath could be caused by an SVT, supraventricular tachycardia.
“This is when the heart speeds up due to a problem with the electrical signals within the heart.”
My mother’s chest X ray was normal.
There was no weight gain and no edema.
Her other cardiac tests were normal: EKG, echocardiogram (though it did show weak left ventricle—the reason for the 25 EF), blood pressure, pulse, pulse-ox, chemical stress test.
Several years ago she had coronary bypass surgery.
If episodes of SVT had been occurring only while she was at home, making her suddenly “unable to breathe” for a few seconds, these transient events would not have been picked up at the ER.
She saw a pulmonologist who ruled out COPD. The pulmonologist did not believe that the very brief episodes of difficulty breathing were caused by a lung disease or even a heart problem.
When lung disease does cause problems breathing, the episode would not just suddenly come and go and last so briefly without any exertion or pattern; it would be more of a persisting situation.
Furthermore, my mother has no other symptoms that the doctor asked about, such as dizziness, fever, lightheadedness, tingling, numbness, nausea, visual problems or rashes.
The only symptom is the periodic sensation of “I can’t breathe.”
The pulmonologist said it’s probably either anxiety related or a vocal cord dysfunction.
And remember, a panic attack can occur in the absence of precipitating worrisome thoughts.
The “program” for panic attack often runs in the background—like a computer program running in the background—not readily apparent, but there.
“Anyone [young or older] experiencing a sudden lack of breath should seek medical attention,” says Dr. Gaman.
If you’re having episodes where you have trouble breathing, and it’s not related to exertion and seems to come on for no reason at all, and are brief (lasting only seconds), get your heart and lungs checked, but it’s probably panic attacks.
Get the more serious causes of trouble breathing ruled out first.

Dr. Gaman is with Executive Medicine of Texas and is with the Staying Young Radio Show 2.0 podcast.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ShotPrime Studio
Hydralazine (Apresoline): Is 300 Mg Daily an Overdose?
Here’s the scoop on accidentally taking 300 mg a day of hydralazine (Apresoline) instead of the prescribed 30 mg a day.
My mother’s cardiac nurse made a mistake which resulted in the pharmacist preparing her prescription for hydralazine (Apresoline) at 10 times the amount ordered by the cardiologist for high blood pressure.
About a month and a half after my mother began taking hydralazine, my father (who takes charge of all the medications) noticed a mistake:
The bottle said that each pill was 100 mg, but the dosing instructions on the bottle said to take one “10 mg” tablet three times a day.
Was this just a typographical error on the bottle, or were the tablets, that my mother had been taking at this recommendation for about a week, really 100 mg?
Well, when my father went back to the pharmacy to investigate, he compared the newly prepared, 10 mg pills to the ones in the 100 mg bottle, and they were smaller.
Initially she’d been taking just one 10 mg tablet a day. It was then increased to twice a day. Then the instructions came in for three times a day.
My father then noticed the 100 mg on the new bottle, but at first didn’t think much of it—until a week later when he just happened to notice the dosing instruction for “10 mg” three times a day.
So instead of 30 mg a day of Apresoline, my mother had been taking 300 mg a day.
My father said he was on “pins and needles” and refused to dispense to my mother any more of the pills, to clear the perceived overdose out of her system.
He called the cardiologist’s office—this was Friday. The cardiologist was out for the day.
I learned about this on Saturday and did some online research about hydralazine overdose.
I could not find how many mg of this Apresoline drug constituted an overdose, but was relieved to learn that 300 mg a day is actually a common prescription—after it gradually gets raised to this amount.
In fact, one site said 400 mg a day was sometimes prescribed, and one site even had it up to 800 mg.
Furthermore, the half life of hydralazine or Apresoline is three to seven hours, sometimes eight, meaning that half the amount of the drug is already cleared from the system in this time frame.
However, symptoms of an overdose can be the following: faintness, passing out, muscle aches, ankle swelling, chest pain, rapid heart rate.
My mother had none of these. But then again, 300 mg a day is a standard prescription amount.
However, a patient is never jumped from 30 mg a day to 300 mg a day overnight, either.
On Monday morning my parents received the phone call they were waiting for, and the cardiologist’s office told her there was no problem with the 300 mg accidental dosing, and that ironically, the doctor will probably want to go up to 300 mg a day over time anyways.
Hydralazine is a vasodilator—it opens up blood vessels so that more blood could flow through the body.
Lesson learned: Always make sure that you KNOW the dose that the doctor has prescribed, or that the doctor has changed (increased or decreased).
Make sure that this number MATCHES what’s on the prescription bottle.
Read the prescription bottle very carefully, even if you need a magnifying glass.
Have the pharmacist recite to you what the prescription is for. This is your right as the consumer!
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/daizuoxin
Sources:
drugs.com/dosage/hydralazine.html
rxlist.com/apresoline-drug.htm
drugs.com/sfx/hydralazine-side-effects.html
webmd.com/drugs/drug-8662-hydralazine+oral.aspx
Pain in Ball of Foot when Cycling: Causes, Solutions

A doctor explains that there are several possible causes to a pain in the ball of the foot when cycling.
This can occur while riding outdoors or while using a stationary bike.
There are several possible causes of pain in the ball of your foot when pedaling a bike.
“Pain in the ball of the foot, especially when cycling, can be due to several issues,” says Nere Onosode, DPM, of OrthoCARE, which specializes in all elements of orthopedic medicine including foot, ankle, knee, hip and shoulder care.
Footwear
“The simplest solution is usually the most missed. Addressing the type and size of shoes used to ambulate and/or ride is important.
“Full length arch supports with forefoot padding can help alleviate pain at the ball of the foot.”
Make sure that your footwear is designed for cycling, or at least, exercise.
Don’t assume that an indoor “exercycle” doesn’t count as enough exercise to warrant proper footwear.
In other words, avoid wearing sandals or flip-flops while pedaling (people have been known to do this).
As for arch supports, these are sold online and at drug stores; no prescription required.
There are many varieties, and you may need to try several different versions before finding the right ones.
Musculoskeletal Causes
Dr. Onosode explains, “From a musculoskeletal standpoint, it could be a bone issue from crowding of the metatarsals that make up the ball of the foot, or entrapment of nerves that run in between those.”
You may even have a hairline fracture of a metatarsal bone, which an X-ray would likely show.
A hairline fracture of a metatarsal bone is a small, often subtle crack in one of the long bones in the foot, which can occur due to repetitive stress or trauma.
This type of fracture is typically characterized by a thin, non-displaced crack that may not always be visible on standard X-rays but at least can be detected with advanced imaging techniques if symptoms persist.
Dr. Onosode adds, “Also, inflammation of the bursa can cause pain. If the pain is related to inflammation, a simple OTC anti-inflammatory pills can help resolve that.”
Bursitis occurs when one of the small fluid-filled sacs that cushion bones and tendons becomes irritated or inflamed.
This condition commonly affects the bursa located at the base of the toes or under the heel.
The inflammation can result from repetitive stress, improper footwear, or direct trauma.
Treatment can also include ice. In some cases, physical therapy or injections may be recommended to reduce inflammation and alleviate discomfort.
In summary, pain in the ball of your foot should not happen while cycling.
If it doesn’t go away despite icing, self-massage and taking a break from the exercise, see a doctor.
 Nere Onosode, DPM, is a Doctor of Podiatric Medicine and board qualified by the American Board of Foot and Ankle Surgery.
Nere Onosode, DPM, is a Doctor of Podiatric Medicine and board qualified by the American Board of Foot and Ankle Surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
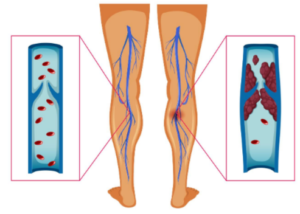
DVT Prevention after Joint Replacement: Portable Compression

DVT (blood clot) prevention after joint replacement surgery can be done with a portable compression device that straps onto the legs.
The standard of care following joint replacement surgery is to send the patient home with a prescription to take a powerful blood thinner drug to prevent the development of a DVT: deep vein thrombosis.
Sometimes the surgeon will instruct the patient to take only aspirin.
Whether the patient takes a prescription blood thinner (Coumadin) or aspirin depends on the surgeon’s viewpoint on these two drugs as well as the patient’s medical history and other unique factors.
However, there is a third way to help prevent post-op blood clots following joint replacement surgery.
Portable (Mobile) Compression Device
The Shiley Center for Orthopaedic Research and Education at Scripps Clinic has conducted research and the report is in a 2015 issue of Journal of Bone and Joint Surgery.
The conclusion of the study is that a portable, strap-on compression device is just as effective as blood thinners in the prevention of a DVT.
The patient can easily walk around with the device on (walking would be limited by the joint replacement surgery itself, however, as the patient heals from the operation).
The device can be used by patients at their home for 10 days, or even longer, following joint replacement surgery—in place of a blood thinner, to stave off a blood clot formation.
Patients should inquire about this device to their surgeons prior to the operation.
Blood Thinners vs. Compression Device
“The risk of bleeding with blood thinners has to be weighed against its benefit in preventing blood clots,” says Dr. Paramjit “Romi” Chopra, MD, founder of the Midwest Institute for Minimally Invasive Therapies (MIMIT), an interventional radiology and endovascular therapy practice.
“Long-term use of blood thinners is not recommended if patients are mobile and at lower risk of DVT once they resume their usual level of activity.
“Lower extremity compression devices, including portable sequential compression devices and even compression stockings, can reduce the risk of DVT.
“They may be a better option in patients at higher risk for bleeding, such has patients with history of GI bleeding.”
Dr. Chopra combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
combines his Eastern roots and 30+ years’ Western experience to unify the best of both worlds at MIMIT to treat venous disease, peripheral artery disease and musculoskeletal disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2014/02/140214152050.htm
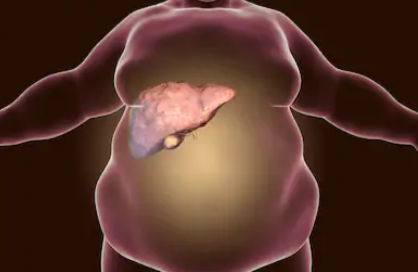
Percentage of Liver Disease Patients with Bad Body Odor
Find out the percentage of people with liver disease who have bad body odor.
What percentage of patients with liver disease have the bad odor?
What’s really odd is that when I do a search on “causes of change in body odor” or “causes of foul body odor,” liver disease is on the list.
But when I do extensive searches on “symptoms of liver disease,” not one of these sites, including esteemed sites like Mayoclinic.com, lists body odor as a symptom.
So just what is that percentage?
“It’s a small percentage, less than 10%, maybe even less than five percent,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“A patient will only have that distinctive odor when they’re in liver failure, and most patients with liver disease do not progress that far.”
Why is the percentage so small?
Dr. Fine says, “We can speculate that this is because the only liver disease patients who experience this symptom are the ones in liver failure and that is a small percentage of patients.”

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/SvetaZi
Can Non-Alcoholic Fatty Liver Disease Cause Bad Body Odor?
Can a bad body stink be caused by non-alcoholic fatty liver disease (NAFLD)?
Ever wonder if non-alcoholic fatty liver disease cause foul body odor? If so, how?
“Yes. If the patient is in liver failure, they’ll develop the odor regardless of whether or not alcohol is involved,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“However, alcohol is the most common cause of liver disease in this country.
“Obesity and high triglycerides are also common causes.”
Non-alcoholic fatty liver disease can cause foul body odor as follows:
A damaged liver doesn’t detoxify chemicals as efficiently as it should.
Compounds like ammonia, sulfur byproducts and ketones can build up in the blood and get released through breath, sweat and urine.
This can create a musty, sour or “rotten” odor that can be detected by someone near that person.
It even has a name: fetor hepaticus.
Hormonal changes, insulin resistance and altered gut bacteria in NAFLD can make this odor even stronger.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Kateryna Kon
Benign Causes of Elevated ALT and AST
Find out if an elevated ALT or AST can ever have a benign cause.
Just what does “elevated” mean in reference to the liver enzymes of ALT and AST?
The elevation can be mild, moderate or significant.
You may be wondering if the cause of a very mild elevation could ever be benign.
Benign Causes of Elevated ALT
“The only benign reason would be if that patient’s normal range is beyond the average, but that is very rare,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“For the most part, there are no benign elevations of ALT — there’s always a reason. Some medications can affect ALT levels, so can alcohol consumption and over-working your muscles.”
If you’re scheduled for a blood test for liver enzymes, do not lift weights for two to four days prior to the test, if you want to ensure that muscle fiber damage won’t influence the results.
However, a report in the British Journal of Clinical Pharmacology notes that in a study, the ALT and AST remained elevated seven days out from an intense weightlifting session in healthy men who were not weightlifters.
Benign Causes of Elevated AST
If the person’s normal range for AST is above average, says Dr. Fine, this can explain an “elevation,” but that’s rare.
“For the most part, AST elevations aren’t benign. There’s usually an underlying pathology like muscle inflammation or alcohol consumption.”
And keep in mind the study in the BJCP noted above.
“If your AST or ALT levels are elevated, see a qualified physician as soon as possible.”

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monkey Business Images
Source: ncbi.nlm.nih.gov/pmc/articles/PMC2291230/
Do AST and ALT Values Show Liver Cancer? What About Hep?

The value of the ALT and AST liver enzymes will vary depending on the type of liver sickness including cancer.
In general (numbers vary from one lab to the next), a blood test value of over 50 for the ALT is considered elevated, not within the normal range. For AST, the cut-off point is 40 (anything above is elevated).
Again, realize that these cut-off points will vary with different testing labs.
What are the AST and ALT values that are associated with fatty liver disease, the common hepatitis viruses, liver cancer and other liver disease?
“AST and ALT levels vary greatly depending on the liver disease and the individual patient,” says Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“In fatty liver disease for example, the AST and ALT values are usually twice the normal range or higher.
“They can be as high as 10 times normal. They can also be up to 10 times the normal range in common hepatitis cases like in hepatitis A, B and C.”
What about cancer?
“With liver cancer, the AST and ALT levels could be mild to normal because those cells are burnt out, so there is no AST or ALT leak,” says Dr. Fine.
Autoimmune Disease
“In autoimmune liver disease, which is more common among women, the AST and ALT levels can be three to six times normal.”
How to protect yourself against liver disease
– Avoid drinking alcohol, or drink only occasionally at the most.
– Exercise regularly, and this includes strength training.
– Avoid processed foods as much as possible.
– Avoid unhealthy ingredients like trans fats and preservatives.
– Lose weight if you’re overweight. If you’re not overweight, don’t gain excess weight.
– Limit foods with added sugars. This includes the so-called nutrition or meal bars.

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Chinnapong
Can “Bad” Cholesterol Be Raised by Non-Fatty Liver Disease?
Non-alcoholic fatty liver disease means something is very wrong with your body.
Can this condition, which is often brought on by poor diet, actually raise your LDL (bad) cholesterol?
“Yes. LDL receptors are located primarily in the liver and their number is regulated by the cholesterol content in the liver cells,” explains Jeffrey Fine, MD, chief of gastroenterology at the Medical Surgical Clinic of Irving.
“When a person’s diet is high in saturated fat and cholesterol, the cholesterol content generally rises. This causes the LDL receptors to fall and plasma LDL levels to rise.”
It’s important to note that the biggest perpetrator in raising cholesterol levels in the body is refined carbohydrates.
The influx of added sugars and white-flour-based foods really does a number on body chemistry and health.
- Avoid white flour as much as possible.
- Limit saturated fats, and avoid trans fats (partially hydrogenated oils).
Non-alcoholic fatty liver disease is often caused by poor diet. High LDL cholesterol is a risk factor for heart attack.
Symptoms of Non-Alcoholic Fatty Liver Disease
Also known as NAFLD, this condition encompasses numerous liver diseases that affect those who drink only a little or no liquor at all.
Too much fat gets stored in the liver cells and can lead to non-alcoholic steatohepatitis, which can permanently damage the liver.
In fact, the damage is similar to what can occur with a heavy drinker, and can lead to failure of this organ.
Usually there are no symptoms, but they may be fatigue and pain in the upper right abdomen.
But the steatohepatitis can cause fluid retention in the stomach, causing it to swell.
Other symptoms of non-alcoholic steatohepatitis: visibly enlarged blood vessels under the skin’s surface, red palms, enlarged breasts in men, and jaundice (yellowing of the skin and eyes).

Dr. Fine has been in practice for over 30 years and specializes in digestive health, integrative medicine and food sensitivities.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Kateryna Kon
Liver Disease Answers: Body Odor, Urine Color, ALT, AST
Below are links to articles about liver disease that answer questions that perhaps you’ve been struggling to find answers for with extensive online searches–which either turned up nothing or vague, overly-broad information.
So I asked a medical doctor to give me the straight answers and wrote the following articles — which include his statements.
Body Odor
Perhaps you’ve heard or read somewhere that liver disease can cause a distinct body odor.
No, not the typical “BO” that one might detect on someone who just had a gym workout, who wears dirty clothes or who doesn’t shower often enough.

Shutterstock/ESB Professional
Can body odor be a single symptom of liver pathology?
How many people with liver problems have bad body odor
Labs
What about those blood tests for liver function?
Ever wonder about those and how telling they might be?

Shutterstock/Olena Yakobchuk
ALT and AST: Looking at the Values
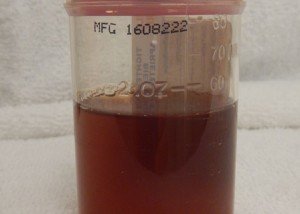
Urine Output
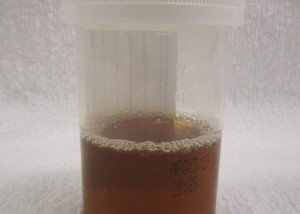
Liver disease can change urine color due to a buildup of bilirubin, a yellow pigment produced during the breakdown of red blood cells.
When the liver is damaged, it cannot process bilirubin properly, causing it to spill into the bloodstream and be excreted in the urine.
This often results in dark brown, amber or tea-colored urine.

James Heilman, MD/CreativeCommons
How common is liver disease?
As of 2025, liver disease remains a serious and growing health concern in America.
An estimated five million adults — about 2% of the U.S. population — have some form of liver disease.
Nonalcoholic fatty liver disease (NAFLD) continues to rise, driven by increasing rates of obesity, diabetes and metabolic syndrome.
In fact, type 2 diabetes and metabolic syndrome are strongly associated with obesity.
Other common forms include alcoholic liver disease, hepatitis B and C, and cirrhosis.