Acid Reflux Chest Pain vs. How Angina Feels

Here is a comparison acid reflux symptoms to those of angina chest pain.
It’s no secret that a person with chest pain from angina can be misdiagnosed as having acid reflux or some other digestive issue.
This happened to my mother who, two days after the misdiagnosis, underwent quintuple bypass surgery after the correct diagnosis was made.
“Chest pain from reflux may be similar to angina pain, so if there’s any chance of cardiac disease, the patient should first consult a cardiologist (or internist) to rule out cardiac disease before embarking on any GI workup, especially if the patient is middle aged or older and hasn’t already had a cardiac evaluation,” says Jonathan Zinberg, MD, chief of gastroenterology at South Nassau Communities Hospital, Oceanside, NY.
“However, reflux pain is typically burning, though may be sharp, often after eating, especially after reclining or overnight. It usually lasts for a prolonged time (20 minutes to a few hours), but improves after an antacid or acid reducing agent.”
Angina Chest Pain
Dr. Zinberg continues, “Angina is typically a heavy sensation, but may be sharp or even burning, usually after activity, but could be after eating, usually is not at rest or reclining or in the middle of the night, but rarely could be so.”
My mother was one of those rare cases. She was awakened at 5 a.m. by chest pain (angina).
“It may be brief and improve with rest,” says Dr. Zinberg.
“If prolonged and not improved with an antacid, seek medical attention.”
Unstable Angina
Angina can occur while at rest, and this type is called unstable angina. “Unstable angina is dangerous and scary,” says Dr. Zinberg.
“It usually occurs in someone who already has a history of coronary disease and angina, and with worsening it may occur even at rest.”
Duration of Chest Pain
“In a setting where there is a reason to be concerned about cardiac disease, if the pain lasts longer than 15 or 20 minutes, medical attention should be sought.
“Known angina patients usually have nitroglycerine to take for acute angina symptoms.
“Otherwise, it’s worth taking an antacid or H2 receptor antagonist (like ranitidine or famotidine) to see if the heartburn will disappear. If it doesn’t, speak to a doctor.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/airdone
Left Side Stomach Pain Worsens After Eating: Causes

Pain in the left side of your stomach after you eat can have serious causes including cancer but also benign causes.
Definitely see a doctor about this.
“This is a nonspecific symptom, has many causes, and will depend on the location and character of the patient and the pattern of exacerbation and relief,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
IBS as a cause of pain in the left abdominal area following a meal.
“This often is seen in patients with irritable bowel syndrome, where one gets left sided cramps, associated with altered bowel function.”
Can causes also be serious?
Dr. Blume continues, “There are numerous causes of this, however, some of which are serious and some are not, including diverticulitis, malignancies, inflammatory diseases involving the bowel, as well as upper gastrointestinal problems.
“Looking up a symptom out of context is often not particularly helpful. Taking a detailed history concerning this symptom is the best way to help determine what the pain is from.
“A physician may or may not order an imaging study, depending on what he or she feels is likely the problem, based on assessing that particular person clinically.
“One normally does not automatically order an imaging study, such as CT or MRI on the basis of a complaint alone.
“One first has to decide what one thinks the problem is, and then decide what test is needed to confirm that impression.”
If you’ve been troubled by left sided abdominal pain after eating, chances are pretty high that your doctor will order an imaging study of that area of your body, such as a CT scan, MRI or ultrasound.
You’ll also probably get a blood test ordered.
Remember, there can be quite a few possible causes of this symptom.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Inspiration GP
Appetite Loss Causes OTHER than Ovarian Cancer
You don’t overeat, you don’t have ovarian cancer, so why have you lost your appetite?
Have you been feeling full “all the time” even though you haven’t been eating more, and even though your doctor said you don’t have ovarian cancer?
Feeling full all the time is a nonspecific symptom, says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
He explains, “One needs to distinguish whether this is a problem with gastrointestinal structure (i.e., obstructive or inflammatory problems) or gastrointestinal function (this may include metabolic problems, medications, as well as functional gastrointestinal disorders).
“Diagnosing this would likely involve a combination of taking a medical history as well as some diagnostic testing.”
For women who have noticed a persistent full feeling, one of your first stops, if not your very first stop, should be with a gynecologist.
Ask the doctor to see if your ovaries are doing well.
Keep in mind that the absence of ovarian cancer does not mean that some other cancer can’t be causing you to feel disproportionately full relative to the amount of food you eat.
Cancers that can subdue the desire to eat include stomach, colon, pancreatic and lung.
Additional Causes of a Suppressed Appetite
– Addison’s disease
– Anxiety
– Celiac disease
– Chronic heart failure
– Crohn’s disease
– Dementia
– Depression
– Diabetes (though this also often causes intense hunger)
– GERD
– Kidney disease
– Liver disease
– Pancreatitis
– Rheumatoid arthritis
– Side effects of cancer treatment
– Stress
– Tapeworm
– Ulcer
– Ulcerative colitis
This list of causes of appetite loss is not complete.
If you’ve been experiencing a loss of appetite lately, then the more symptoms that occur with this, the more concerning your situation is.
For example, a suppressed appetite that’s also accompanied by vomiting, unexplained fatigue and/or abdominal pain should be immediately checked out by your doctor — regardless of your age — or gender.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/VGstockstudio
Non-Cardiac Causes of Dizziness when Eating

If it’s not your heart, what can be causing dizziness while you eat?
Eating should be an enjoyable experience, not something you dread because it causes you to feel dizzy.
Non-cardiac causes of dizziness while eating are many.
“One needs to remember that just because you are having gastrointestinal symptoms, does not necessarily mean that this is from a gastrointestinal problem,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
He continues, “This is a nonspecific symptom and can be related to metabolic or neurologic issues.”
Getting dizzy when eating can have a number of causes.
Dr. Blume explains, “One can see this from problems involving abnormal gastrointestinal function, such as when one’s autonomic nervous system (the part of your nervous system that works without you thinking about it) — specifically the parasympathetic nervous system — function is abnormal, where one can get dizzy after eating.
“However, one often gets other symptoms along with this, such as feeling clammy, flushed, nauseated or having erratic bowel function.”
If dizziness during eating keeps happening to you, make an appointment with your physician.
This is not normal and needs to be evaluated. There is no known food that makes a person feel dizzy or causes vertigo while it’s being eaten.
Occasional dizziness when eating is probably not caused by eating or anything related to the GI tract.
Rather, it’s likely a coincidence in that whatever the cause of the symptom is, just happens to act up while you are eating.
Keep a record of these events so that you can potentially identify a pattern, or at least, present to your doctor.
Documentation can help you determine if the dizziness does or does not occur at other times unrelated to food intake.
You can make a note if there are other symptoms that may suggest a cardiac problem such as chest pain, feeling faint and/or feeling short of breath.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
What to Tell Cardiologist if You’ve Been Passing Out

A cardiologist explains the details you should give your cardiologist if you’ve been blacking out.
Have you been blacking out and are planning on seeing a cardiologist?
Don’t just tell the doctor, “I’ve been having blackouts; what’s wrong?” Certainly, your doctor will ask questions to get more information, but you should also be prepared to give specific information.
You should tell the doctor “the exact symptoms before and after the blackout,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Dr. Sayeed continues, “Whether they could feel it coming or if it was just like a flip of a switch — awake one minute, found on the ground with facial and head injury the next without warning.
“They should tell their cardiologist if they felt any abnormal heartbeat, palpitations, chest pain, lightheadedness, dizziness before it happened, or if they feel changes in certain positions make them feel like passing out.
“They should tell their doctor if it occurred after urinating, a big bowel movement, meal, extreme activity or taking medication.
“They need to tell the doctor if they are diabetic and taking diabetic drugs or exercising. Whether they feel completely normal or awakening from the blackout and feel funny.”
Though blackouts can have non-cardiac causes, it’s important to rule out any possible heart problem.
Dr. Sayeed says cardiac causes can be a “slow heart rate; pauses in the heart beat; fast and irregular heart beat; severe obstruction of a heart valve; and carotid sinus hypersensitivity causing fainting with changes in position.”
Of course, the sooner you see a cardiologist after a blackout, the less you’ll have to tell your doctor, but some people DO put off seeing a doctor, or, they see a doctor but fail to give as much information as they are capable of.
So every time you have a blackout, it’s vital to document all the details that you experienced just prior to it, after it, and even within 15 minutes of it, to see if a pattern emerges.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com jcomp
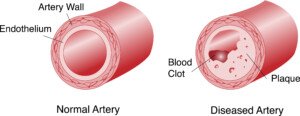
CT Angiogram for Chest Pain: Cost, Availability & Safety

If studies show the accuracy of CT angiogram for detecting heart disease, why isn’t this tool used more often in chest pain ER cases?
Research have shown the efficacy of the CT angiogram in detecting heart disease in patients presenting to the ER with chest pain, so it makes absolutely no sense to me, the layperson, why this tool isn’t used in a standard way across the board in emergency room settings.
“Coronary computed tomographic angiography (CCTA) has been shown to have a high negative predictive value for the detection of coronary disease,” says Donna P. Denier, MD, of The Cardiology Center with the Appalachian Regional Healthcare System in NC.
“That is, it is very useful in ruling out the presence of coronary disease, even more than ruling it in,” continues Dr. Denier.
“The issues of its usefulness are cost, availability and safety. The majority of patients who present to an emergency department with chest pain can be categorized quickly into one of three groups based on a careful history, physical exam, evaluation of risk factors and review of EKG and troponin results.”
Troponin is an enzyme that leaks from the heart when there is cardiac muscle damage (heart attack).
Thus, as you may now be realizing, a troponin test detects a very recent or current heart attack, not blocked coronary arteries.
My mother’s troponin results were normal after I took her to the ER when she complained of shortness of breath and had vomited.
Three days later (after a second ER visit) she underwent quintuple bypass surgery!
Dr. Denier continues, “High risk patients are admitted and usually undergo cardiac catheterization (such as my mother) which makes a rapid conclusive diagnosis and allows for treatment at the same time.
“Low risk patients (e.g., athlete, under age 50, nonsmoker, healthy body weight/blood sugar/blood pressure) can be sent home and followed as outpatients for further testing.
“For low risk ambulatory patients, a stress test is the best test to rule out coronary disease because it gives functional information as well—how how far a patient can walk without developing symptoms.”
What about the moderate risk patient in the ER with chest pain? “It is the moderate risk patient who requires a test to safely rule out the presence of significant coronary disease,” says Dr. Denier.
“CT angio is clinically useful in this group. As this test is performed while the heart is beating, quality imaging is dependent upon slowing the heart rate enough to image between cycles.
“This limits some patients due to rapid or irregular heartbeats that cannot always be controlled with medication. Some patients cannot tolerate the medication that is used to slow the heart.
“Radiation exposure is another concern and although this has been reduced by newer technology, all centers do not have the latest equipment.
“Cost is definitely a limiting factor, and the test is not universally covered by insurance companies, as it is still considered a screening test.
“As technology evolves, cardiac CT will continue to be one of the techniques considered for the rapid and accurate evaluation of patients with chest pain.”

Dr. Denier has been practicing medicine for over 20 years and is board certified by the American Board of Internal Medicine – Cardiovascular Disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Tests from a Cardiologist to Evaluate Why You’re Fainting

A cardiologist talks about blackouts and what tests you should get to find out if the problem is heart related.
Have you been having blackouts and “all the tests” are normal? Perhaps you haven’t had the right tests.
First of all, the doctor you should initially see is a cardiologist, since blackouts can be caused by serious heart problems that need immediate attention.
So just what are the tests you should insist upon for blackouts?
“One could consider an echocardiogram to make sure there are no problems with the heart valves,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Dr. Sayeed continues, “A holter monitor could check for abnormalities in the heartbeat. A stress test could look for abnormal heartbeat with exercise. A tilt table test could evaluate for blackout with different positions.”
Some people black out soon after rising from a prolonged seated position. Their blood pressure plummets and the brain is starved of oxygen, causing the blackout.
The tilt table test measures blood pressure when the patient is in various positions.
Can a seemingly healthy person, with no previous concerning symptoms, suddenly one day drop from a blackout?
“Yes, this can certainly happen, as the electrical system in the heart can suddenly decompensate, especially in an older person, and this is why they frequently come in with bruised or injured faces or head injury.”
On the other hand, a person can begin experiencing suspicious symptoms, short of an actual blackout, that progress over time, one day culminating in a full fledged loss of consciousness.
Dr. Sayeed, explains that “there can be a transition period, especially if they are just having brief episodes of abnormal heartbeat and if this progresses over time to worsen the heartbeat. The symptoms can get worse and eventually lead to syncope.
“This is usually less common and usually a more drastic sudden blackout is how patients usually present.
“But certainly a gradual onset over time can occur especially if the person can tolerate the symptoms quite well.”
If you have even ONE blackout, do not delay getting tests, because this symptom is never normal.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
Shortness of Breath from Heart Problem vs. Narcotic Drugs

Is there a way to distinguish between breathing difficulty from angina and from narcotic painkiller side effects?
Narcotic painkillers can cause trouble breathing as a side effect, yet angina as well can result in this scary symptom; is there a way to tell one type of labored breathing from the other?
“Narcotic side effects would make them drowsy or unconscious, and breathing would become dangerously slow or even stop, and the person may not even realize it,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“Angina is usually reproducible with the breathing difficulty happening each time they do a certain amount of activity, walking, etc., and once it is severe would even occur at rest, and the person would be very uncomfortable and definitely would realize it.”
So if you’re on narcotic painkillers, and you feel fine all along, and suddenly develop difficulty breathing, chances are very high that this is NOT a side effect from the narcotic drugs.
It’s not necessarily angina, either, but you can pretty much rule out narcotic side effects if this is your only symptom, and especially if it came on during mild exertion that’s too light to justify the shortness of breath.
My mother had been on narcotic painkillers, and on and off complained of “labored breathing.”
We all thought it was from the narcotics because the inserts listed this symptom as a possible side effect (along with a huge host of other potential side effects).
It’s much more likely that all along this symptom had been caused by severe coronary artery blockage, because eventually she was diagnosed with very severely blocked arteries (after being diagnosed with unstable angina), and had to undergo coronary bypass surgery.
If you’re worried about your heart health, see a cardiologist and also have your coronary calcium score taken.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/PrinceOfLove
Why a Stress Test Can Miss Severe Artery Blockage
Find out how often and why cardiologists miss severe heart disease when examining a patient.
It’s possible for a cardiologist to miss severe heart disease when giving a patient a heart exam, and actually go as far as telling the patient, “You’re the last person I’d ever expect to have a heart attack.”
This happened to my mother. Ten months later she had emergency quintuple bypass surgery.
“This can happen if the stress test is normal but the patient has severe triple vessel coronary disease,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“Some nuclear stress tests can be normal in the setting of triple vessel disease due to a phenomenon called balance ischemia where the blood flow discrepancy cancels each other out and the test appears normal.”
In other words, relative blood flow is detected, rather than absolute blood flow.
Thus, if only one or two of the three major vessels is/are severely blocked, this will cause a disparity in blood flow that will be easily detected.
How common is balance ischemia as a camouflage in a stress test?
Dr. Sayeed says, “This probably happens in a relatively small percentage of people, 5% or less. A cardiologist with a high suspicion of disease based on symptoms and exam and history would not trust the falsely normal stress test and probably perform a coronary angiogram.”
But what if the patient reports no symptoms?
My mother did not have symptoms 10 months before three doctors said that a massive heart attack was imminent.
She saw a cardiologist because an EKG, taken in the ER as part of a complete workup to find out why she was sleeping so much, revealed a “left bundle block.” The ER doctor told her to follow up with a cardiologist.
The cardiologist did not order a stress test or any other imaging procedure.
She gathered subjective information from my mother, then examined her with a stethoscope, noted the pulse and blood pressure, and declared her heart healthy.
If the patient has no symptoms, has normal blood pressure, normal pulse, is not diabetic, does not smoke or drink, is not obese and reports no family history of heart disease, what SHOULD the cardiologist do?
When the cardiologist asks the patient, “Do you exercise?” and the patient says, “Well, I maintain a large house that has a staircase, and I’m up and down those stairs a hundred times a day,” the cardiologist should see a blaring red flag.
When people say things like this, assume they are sedentary!
A staircase in the house does not mean the resident has a built-in cardiovascular exercise program!
My mother had three blaring risk factors for severe heart disease that the cardiologist should NOT have missed:
1) elderly age
2) lack of structured aerobic exercise
3) excess fat in the midsection (though she was not obese).
The cardiologist should have probed further with the exercise — for example:
“Do you do any brisk walking for at least 30 minutes most days of the week — and whatever walking you do while shopping does not count.”
And, “Do you take any fitness classes? Do you use any cardio machines like a bike, treadmill or elliptical? Do you jog?”
Sedentary people have a way of convincing themselves they get “plenty of exercise” by believing that housework and shopping count as sustained, rhythmic cardiovascular exercise!

Freepik.com
Though probing the exercise habits often will not turn up useful information when so many people believe that walking 3 mph on a treadmill while holding on counts as meaningful cardiovascular exercise, the probing can definitely yield insight to the cardiologist screening for severe heart disease.
The cardiologist asked my mother about her diet.
My mother replied, “I eat a balanced diet. I hardly eat fast-food. I watch my portions. I don’t eat much sweets.” The cardiologist did NOT probe further.
The problem isn’t so much the type of food; it’s the BRAND.
Popular, commercial brands of processed goods (potato mixes, pasta mixes, seasoning packets, salad dressings, bread crumbs, frozen dinners, frozen side dishes, processed frozen meats) are full of trans fats, which damage coronary arteries!
My mother’s diet was rich in heavily processed foods: trans fats! Trans fats are also “hidden” in foods whose packaging says “Zero trans fats!”
As for no family history of heart disease, my mother confidently declared this, even though at the time, her son had been diagnosed with heart disease years before, and she had siblings whose health histories she was not aware of (one eventually had a heart attack!).
Do you now see how easy it is for a cardiologist to miss severe coronary heart disease?
Shutterstock/OSweetNature
If you’re worried about your heart, be sure you know the FACTS to what seem to be simple questions that the cardiologist will ask about your lifestyle and family history.
And get your coronary calcium score taken; discuss this with your cardiologist, as this can be extremely telling of the presence of severe coronary heart disease.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Zero Calcium Score: How Soon Can a Bad Diet Raise It?

If your calcium score is zero and you go bust with your diet, how long before the score rises?
Your calcium score is zero because you’ve been having a healthful diet and exercising, and maybe there’s some good genetics and/or youth tossed into the equation.
But let’s suppose that lately you’ve been gorging on sugary foods with trans fats, and eating very little of the vegetables and fruits you used to eat a lot of.
Maybe you’ve been stressed. Stress can lead to junk food consumption as a form of emotional relief or comfort.
The body’s stress response triggers cravings for high-fat, high-sugar foods, which can temporarily boost mood.
How long do you have to keep up this bad diet before it raises that calcium score of zero?
“Usually a calcium score or stress test gives an average person about a three to five year warranty in that if it is normal, the risk will probably be low for that period of time,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“If someone is abusing their diet, it is possible that plaque could build up in three to five years’ time to the point where it could be detected on calcium score,” adds Dr. Sayeed.
“This is about how often stress tests, but not necessarily calcium scores, are repeated to monitor for new flow-limiting plaques.”
If your calcium score is zero, indicating no significant calcified plaque in your coronary arteries, it’s important not to use this as an excuse to abandon healthy eating habits.

The closer a food is to its natural state, the healthier it is for the human body, especially the heart.
Consuming a menu high in processed foods and added sugars can still pose risks to the person with a zero calcium score, because sugars contribute to coronary artery plaque buildup over time.
While a zero calcium score is a positive sign, maintaining a plant based diet rich in whole foods and low in processed sugars is the magic bullet for long-term heart health and preventing future cardiovascular issues.
You should read ingredient lists of your favorite foods.
You’ll be surprised over the amount of “hidden” sugars. Any ingredient that ends in “ose” is a sugar.
Trans fats can appear under various names on ingredient lists. Common names include:
1. Partially Hydrogenated Oils: The primary source of industrial trans fats.
2. Hydrogenated Oils: May also contain trans fats, though less than partially hydrogenated oils.
3. Vegetable Shortening: Often contains trans fats unless specified as trans fat-free.
4. Margarin: Some margarine products contain trans fats, though many have been reformulated.
5. Fully Hydrogenated Oils: These are typically low in trans fats but can still be present in some products.
Also avoid anything with “interesterified” fat in it.
Always check labels carefully and choose products that list “no trans fats” or “0 grams of trans fats” to avoid these harmful fats.
Calcium score is very predictive of the presence of coronary heart disease.
Calcium score is calculated using a CT scanner without contrast dye.
The test takes about 15 minutes and shows only the amount of calcified or hard plaque.
It does not show the soft or unstable plaque deposits.



 Jonathan Zinberg, MD
Jonathan Zinberg, MD