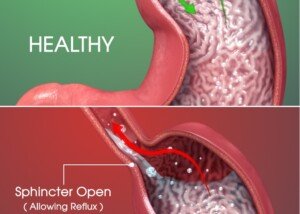
Can GERD Cause Heart Problems?

GERD can cause chest pain but do you fear it can lead to heart problems?
GERD causing heart problems is a common concern among the many sufferers of acid reflux disease, which is a prevalent condition.
Gastroesophageal reflux disease can cause burning, aching and strange feelings in the chest as well as the upper abdomen.
Can GERD negatively affect the heart?
“GERD cannot cause heart disease, but esophageal symptoms can be confused with cardiac symptoms,” explains Larry Good, MD, who’s been a practicing gastroenterologist for 40+ years. He has a private practice located in Lynbrook, NY and is affiliated with Concierge Choice Physicians, a leading provider of personalized care in the U.S.
In addition to chest pain, burning and aches, GERD can also cause issues with the throat such as coughing, a hoarse voice and a feeling of a lump in the throat.
When acid reflux makes its way to the throat, causing symptoms, the condition is known as LPR: laryngopharyngeal reflux disease.
Heart Chest Pain vs. GERD Chest Pain
Dr. Good continues, “Typical cardiac chest pain from angina pectoris is described as an oppressive heavy chest pressure (on elephant sitting in the chest) with difficulty breathing.”
Though you are now assured that GERD does not cause problems with the heart, you are not quite out of the woods.
Acid reflux disease, over time, depending on severity and frequency, can lead to pathological changes in the esophagus, bringing on a condition known as Barrett’s esophagus: abnormal cells.
This in turn increases the risk of esophageal cancer by leading to cellular changes.
Another important point to consider is this:
Just because GERD does not cause any problems with the heart, does not mean that you do not have coronary heart disease!
You may very well still have clogged arteries! Consider getting a complete exam by a cardiologist.
 Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sudden Severe Stomach Pain, Diarrhea: Causes

Sudden severe stomach pain and diarrhea can be quite scary.
“Acute severe abdominal pain and diarrhea implies severe intestinal inflammation,” says Larry Good, MD, a practicing gastroenterologist for 40+ years. He has a private practice based in Lynbrook, NY and is affiliated with Concierge Choice Physicians, a leading provider of personalized care in the U.S.
“It is important to understand the difference between the stomach (one organ) and the abdomen,” continues Dr. Good.
Of course, when a person feels intense pain in this area, the term “stomach” and “abdominal” become interchangeable to that person, because the way they see it, “stomach” refers to the section of their body between their bellybutton and sternum.
“Severe abdominal pain with urgency to defecate [diarrhea] is usually caused by an intestinal infection (viral, bacterial, food poisoning) or by a chronic inflammatory disorder like ulcerative colitis or Crohn’s disease.”
Sudden Severe Stomach Pain: Benign Form of Colitis
Another inflammatory disorder that can cause these symptoms is microscopic colitis. Like ulcerative colitis and Crohn’s, this is an inflammatory bowel disease, but it’s far more benign.
You can have it and not even know it, depending on the frequency of the diarrhea and how “normal” it looks.
One of the key features of microscopic colitis is that the diarrhea may be nocturnal.
I have MC (the very intermittent kind), and one time in the middle of the night, I was awakened by a lower abdominal cramp and the urge to have a bowel movement.
Once I sat on the toilet, I was overcome with severe lower abdominal pain—not the typical “pain” you feel when you have a lot of hard BMs to void. It was so intense I felt nauseous.
And then the diarrhea came (not a lot), and poof, the pain was gone! This was a one-time flare, unrelated to previous food intake.
“Chronic abdominal pain, urgency and diarrhea including fecal incontinence is frequently caused by diarrhea-predominant irritable bowel syndrome,” says Dr. Good.
 Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sebra
Burping from Stress: The Why? and Solutions

Burping can be caused by stressful situations or anxiety, and we all know how embarrassing this can be.
Those around you are likely to think that your burping is because you either ate a lot of gassy foods, or…you’re just, well, uncouth.
So why does stress or anxiety cause burping anyways?
“Stress can cause esophageal spasm and that can cause air to be trapped in the esophagus and cause ‘stress burping.’ Swallowing air can also be a nervous habit,” says Larry Good, MD, a practicing gastroenterologist for 40+ years. He has a private practice based in Lynbrook, NY and is affiliated with Concierge Choice Physicians, a leading provider of personalized care in the U.S.
The esophagus is your so-called food pipe. It is a muscle, though not the type of muscle (skeletal) that you use to bench press a barbell. Any kind of muscle can go into a spasm.
Though an esophageal spasm can cause chest pain–sometimes intense–there are times when an esophageal spasm cannot be felt.
However, despite that, they may produce a burp due to that trapped air that Dr. Good points out.
So what can you do about this embarrassing problem?

Shutterstock/Nik Stock
It is pretty tough to just knock out all the stress in your life.
But what you can focus on doing is altering the way you respond to anxiety-provoking situations.
If you are in an intense business meeting, where people will hear you burping, take some deep breaths and stay calm.
If you are undergoing stress or anxiety, make sure you are not in the habit of swallowing air, including when you gulp beverages. Few people like to hear others burping.
 Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
Dr. Good has additional expertise in the diagnosis/treatment of IBS and inflammatory bowel disease, and is extremely proactive in genetic testing, individualization of pharmacologic treatment, and risk mitigation in cancer screening/prevention. Concierge Choice Physicians
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/pikselstock
600 Pound Life Enablers: What Happened in Their Childhood?

Something happened in the enabler’s childhood that makes them keep bringing food to the super morbidly obese (“My 600 Pound Life”) who can’t move much.
Many of the “600 Pound Life” subjects are actually closer to 700 pounds.
What on earth could have happened in the enabler’s childhood that drives them to keep bringing life-threatening amounts of junk food to their loved-one who can barely get out of bed—and sometimes can’t?
- How can the enabler trade their OWN life for the continuous “caregiving,” which includes gruesome tasks such as cleaning up infections beneath enormous rolls of fatty tumors?
- How are the enablers able to stomach the sights and odors that come with their role?
- This isn’t about love and devotion. Something else is going on here.
“Codependency” is the dynamic between the enabler and the 600+ pound, bedridden or severely immobilized loved-one.
The Enabler’s Childhood
“The characteristics of codependency invariably originate in childhood,” begins Linda Centeno, PhD, clinical psychologist, and assistant director of the Koch Center in NJ that specializes in eating disorder treatment.
“Many codependent individuals [the enablers] have had to endure difficult family dynamics in their families of origin and have had to develop ways of coping to survive,” continues Centeno.
“Children who come from chaotic families often feel worried and scared. They feel that things are unsafe and often try to make themselves feel better by focusing on controlling others’ behavior in an attempt to ‘keep the peace.’
“When children grow up this way, they learn not to think of themselves and what they may need, but how to appease and take care of others.”
If you’re a regular viewer of “My 600 Pound Life,” you’ve probably seen the episode where the husband routinely trekked a considerable distance by foot to the grocery store to shop for his immobilized wife, lugging back large quantities of food across a big field of grass.
You’ve seen Dillon, young adult son of Pauline, leading a life completely absent of friendships and hobbies, because all of his time was focused on enabling his mother.
Though offspring of the super morbidly obese grew up in their enabling role, what about people who became enablers only after they reached adulthood?
As Dr. Centeno explains, the child in a chaotic family environment never learns to focus on himself or herself.
You’ll note that in “My 600 Pound Life,” the enabler is rarely, if ever, a professional with some outside hobby like golf, hiking, karate or volunteer activities.
The learned dynamic “makes it difficult for the person to know who they are as a person separate from the one they are trying to help,” says Dr. Centeno.
“It is safer psychologically to stay attached and needed than to individuate and become a separate person in their own right.” Penny’s husband Edgar comes to mind.
“The result is that they become enmeshed, do not feel a separate sense of autonomy, and know no way to be without the person they are trying to take care of. In fact, the idea of standing alone can feel tantamount to death.”
This is why the enabler, though knowing that a heart attack can be one meal away, continues feeding their loved-one dangerous amounts of unhealthy food.
Enablers Can’t Say “No!” out of Love
How many times, on “My 600 Pound Life,” have you heard the enabler say they can’t say “No!” to all the food demands because of their “love” for that person?
You’ve heard, “How can I say ‘No’ to my daughter,” and, “How do I say ‘No’ to the man I love?”
Explains Dr. Centeno, “In the case of a relationship with a morbidly obese individual, many caregivers do not even realize that they are codependent. These dynamics are unconscious.
“The person feels that this is the way they have to be, and can even take a certain amount of pride (and security) in feeling that they are doing a good job; that they are devoted, loving and responsible.
“It is the source of the positive feelings they have about themselves and it is nearly impossible to imagine themselves separate from the dynamics of the relationship.
“If the person is focused on the caregiving aspects of their loved-one’s extensive needs, then there are no autonomous decisions to be made, no time to look at their own conflictual feelings, such as anger, resentment or emptiness.
“The caregiver feels so needed and indispensable and their own self-worth is so wrapped up in having to take care of the other, that it actually saves the caregiver from the daunting task of having to find their own purpose as a separate individual.”
This sounds so much like Pauline’s son, Dillon, but also many of the people who became enablers after they reached adulthood.
“Many caregivers worry that without the other, they would have no purpose.”
Dr. Centeno adds, “Unconsciously, a caregiver may worry that the partner may leave him or her and then the caregiver would be forced to be separate and autonomous (and alone).
“The person who is in love with the morbidly obese individual is hungry to be loved and needed by them.
“However, the morbidly obese person is addicted to food and has replaced the love for their partner with love for food.
“Essentially, this dynamic leaves the caregiver with many unmet needs. But the feeling of being needed by their partner is often more powerful than the fear of being alone.”
Not everyone will turn out to be an enabler to a 600 pound individual—regardless of how chaotic their childhood is — simply because not everyone’s brain is innately hardwired the same way.
In short, enabling is NOT something that can happen to anybody.
 Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Long Femurs, Short Shins, Short Torso: Squat HELL

Learn everything imaginable about long femurs, short shins and long torsos and the BACK SQUAT.
I’m a former certified personal trainer for a health club chain.
When you look at me you won’t see a woman with a short torso relative to her overall height.
Instead, I have short shin bones relative to my femur length. And this definitely causes mechanical problems when performing the squat.
I’m also convinced it interferes with my deadlift, in that if my knee joints were two inches higher, I’d probably be able to put at least 80 more pounds on my deadlift.
Below are articles that EXPLAIN EVERYTHING. You will never, ever again fail to understand why the long femur to short torso, or short shin to femur, presents a problem with performing the back squat.
And you’ll be able to extrapolate from that information sharper insight into why you have difficulty with other compound movements, including those in the tasks of daily living.
ARTICLES ON FEMUR, SHIN & TORSO LENGTH
Often, the people who claim that long femurs relative to torso is no excuse for a poor back squat or for struggling with correct form — actually have good body proportions for this exercise. They’re not exactly in a position to criticize.
Did you know that short people can have “long” femurs? Femur length needs to be put into context. It’s not an absolute.
Being short doesn’t automatically give you good anthropometrics for the squat.
And conversely, tall individuals can have short femurs. Again, it’s about context, not absolutes.
It’s wrong to say “Tall people have difficulty squatting.”
With poor anthropometrics, as they apply to the back squat, comes issues that impact how much weight can be moved.
Everyone talks about the squat when it comes to long thighs.
But what about in the activities of daily life? How much does the femur issue affect activities that involve squatting?
Stop comparing squatting in adults to that in kids. This is a very unfair comparison. Sure, it’s fun to compare it in the context of envy.
But in the context of, “My four-year-old has perfect squat form; why don’t I?” you’re being very unfair to yourself. And unrealistic.
There’s not nearly as much discussion about shin length as there is for femur.
But it’s not always about femur length when it comes to a barbell squat. The relative length of one’s shins can heavily factor into the equation.
Have you ever tried squatting to parallel or even a bit past this point while wearing high heels?
Well, if you’re a man, you probably haven’t, but if you’re a woman and have a pair of chunky heel shoes, go put them on and see what happens with your back, and how it all feels, when you squat down to parallel.
It’s so much easier! Even an extra one-inch elevation makes it easier. Here’s why:
Are you sick and tired of hearing people claim, “If you can rise from a chair then you can squat”? I sure am. This is a very inept frame of reference.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vladimir Sukhachev
Have you Looked at Your Poops Lately?

How often do you examine your poops? You may be amused at this question, or maybe you’re thinking, “Ewwww.”
But so many things about bowel movements can tell a LOT about a person’s health, about what might be going on–ranging from benign (though annoying) conditions to cancer.
“Most of us understandably think about how often we have a bowel movement and why our stool changes in appearance and consistency,” says G. Shelton McMullan, MD, board certified gastroenterologist with Capital Digestive Care in MD.
“It is very normal for our defecation frequency to fluctuate and also for the size/shape and appearance of our stool to vary, without any seeming pattern,” continues Dr. McMullan.
Floating Poop
“Often when our stool is loose, it will break up easily in the toilet or sometimes float at the top of the bowl; this is not specifically a cause for concern,” says Dr. McMullan.
Slimy Stools
“When the stool in addition appears to be ‘slimy’ and/or associated with what looks like oily deposits, this can potentially be representative of a condition called exocrine pancreatic insufficiency (EPI), involving dysfunction of the pancreas in digesting fats and protein,” explains Dr. McMullan.
“Anyone with concern should mention this to his or her healthcare provider for possible further investigation; a simple submission of stool with testing of something called fecal elastase allows for the diagnosis of EPI.”
How often do you check your bowel movements’ color?
There’s no need to obsess over this, but definitely from time to time you should take note of your poop color.
Dr. McMullan explains, “In terms of the color of one’s stool, my attention is heightened when I hear about pitch-black stool with a sticky consistency, as this could represent a bleeding source within the gastrointestinal tract.
“This type of bloody stool is termed melena and has the appearance of what one would expect lava from a volcano to look like.
“Maroon or bright-red bloody stool obviously is abnormal, so this should always be reported.
“In addition, if one’s stool remains light or clay colored [greyish], this raises suspicion for a possible blockage of the main drainage duct of the gallbladder, liver and pancreas.
“Outside of these mentioned colors, color of one’s stool is in general not concerning.” This means that fluctuations in any shade of brown (light, chocolate-brown, deep brown, brownish tan, etc.) is normal. Varying tinges of green with the brown is also normal.
Still Overly Poop Worried?
Check out the very helpful articles below to see what different gastroenterologists have to say about bowel movements. .
It’s time to start getting familiar with your BMs. What your poops look like can be very telling of your health.
 Dr. McMullan has published numerous medical abstracts and presented posters related to the management and treatment of inflammatory bowel disease and other gastroenterological conditions.
Dr. McMullan has published numerous medical abstracts and presented posters related to the management and treatment of inflammatory bowel disease and other gastroenterological conditions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/dizain
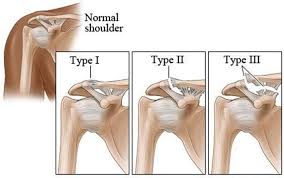
Why You Have Pain Long After Grade 2 AC Separation
Why is it that a year, even two years after a grade 2 AC separation, an athlete can still have pain and struggle through weightlifting sets?
“If the patient is still symptomatic it may either have not been a grade 2 injury or it may need a reconstruction,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“I would advise seeing an orthopedic surgeon.”
Does this mean that a grade 3 AC separation was misdiagnosed as a 2?
Dr. Oheb says, “Not necessarily. You can have a grade 2 injury which is persistently symptomatic. I cannot give you a simple answer to this question.
“Some things require a thorough evaluation of the patient and the X-rays to determine the root cause of a patient’s pain. There is no range of motion test that strongly points to a grade 3.”
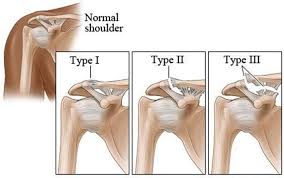
What Is a Grade 2 AC Separation?
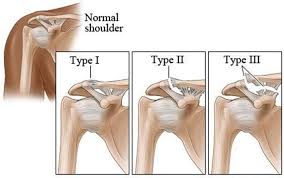
A grade 2 acromioclavicular (AC) separation is when the AC joint is partially dislocated, and the acromioclavicular ligament is completely torn.
This ligament connects the acromion, a part of the shoulder blade, to the clavicle (collarbone).
The complete tear of this ligament causes the clavicle to move partially out of alignment with the acromion, resulting in visible displacement and pain.
Despite the complete tear of the AC ligament, the coracoclavicular ligaments, which connect the clavicle to the coracoid process of the scapula, remain intact.
These ligaments stabilize the AC joint and help prevent the clavicle from shifting excessively.
Their intact condition provides some stability to the joint, even though the AC ligament is damaged.
In some cases, if the symptoms do not improve or if the injury severely impacts shoulder function, surgical intervention may be needed to repair the torn ligament and re-establish joint stability.
Symptoms
- The pain ranges from medium to severe.
- Swelling may be present.
- Movement of the arm induces pain.
- There may be a small bump where the clavicle bone ends, at the top of the shoulder.
- Pushing the clavicle with a hand may move it. Do not experiment with this. It’s not necessary for you to evaluate the injury this way. Only a doctor should do this.
- There may be pain when touching the area.
With proper diagnosis and treatment, a patient should not experience pain during strength training, weightlifting or other physical activities long after treatment and rehab end.
If you have recently injured your shoulder, and it’s so painful that lifting your arm straight out in front of you (frontal raise) is impossible due to pain — see a doctor as soon as you can.
If your injury does not involve the AC joint, it may be a clavicle fracture.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Andrey_Popov
Why Isn’t Surgery Recommended for Grade 2 AC Separation?
Since the ligaments are torn in a grade 2 AC separation, why isn’t surgery the treatment of choice?
One day I was doing stool stepping exercise in my living room.
Suddenly, it were as though an unseen force yanked me off the stool while I had one foot on it and threw me to the floor.
It was over in a split second; too quickly for my athletic body to react. I landed on my shoulder and it hurt like hell.
I diagnosed myself with a possible AC separation, either a grade 1 or 2.
Separation of the acromioclavicular joint is usually caused by falling on one’s shoulder — which can happen after falling from a height or being tossed from a bicycle or skateboard.
A more serious injury (higher grade) may occur from a vehicular accident.
In a grade 2 AC separation, ligaments are torn from the bone.
A ligament is a type of connective tissue that connects bones to other bones at joints, providing stability and support.
Ligaments are composed primarily of dense, fibrous collagen fibers, which give them strength and flexibility.
Now in the case of an ankle injury in which ligaments are actually severed, surgery is the standard treatment. Same with the ligaments in the knee.
So I wondered why, in the case of a grade 2 AC injury, surgery isn’t performed.
“It is not recommended because it has not been shown to significantly improve the average person’s long-term function,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“However, with a high demand patient who continues to have symptoms after a course of conservative treatment, surgery would then be an option.”
In my case, the injury turned out to be a hairline fracture of the clavicle.
This type of fracture is typically caused by trauma or impact, such as a fall or direct blow to the shoulder.
The symptoms were identical to that of a grade 1 or 2 AC joint trauma save for a visible deformity.
Treatment for a hairline clavicle fracture often focuses on pain management and immobilization of the shoulder, commonly with a sling or brace.
My injury healed beautifully with patience plus a homemade sling.
Standard Treatment for a Grade 2 AC Joint Injury
- Rest from activity
- Use of a sling
- Cold packs
- Painkillers
- Physical therapy
The above protocol works superbly; surgery is not required unless the injury is really severe.
Prevention of an AC joint separation is not related to physical fitness.
It’s related to activity. Be extra careful when you’re involved in activity that has the potential to cause a fall.
This includes hiking downhill and walking down an outdoor staircase that’s coated with a thin, often not very visible, layer of ice.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Is Any Exercise Restricted for Grade 2 AC Separation Recovery?

If you have a full recovery from a grade 2 AC separation, is there any exercise that you should never try to do ever again, being that the ligament is no longer attaching two bones, and instead is in a state of perpetual tear?
I was inspired to write this article after reading in a forum about a young man’s concern about deadlifting with a grade 2 AC separation.
He was afraid that “there was nothing holding it together,” referring to the joint, when he was picking up a heavy barbell off the floor.
He was afraid that something would just break off in his shoulder joint.
Take a look at the diagram below showing the grades of an AC joint injury.
Any deadlifting or other weightlifting enthusiast will certainly wonder if, after the injury heals (no longer painful, swollen or bruised; no restriction of motion), any strength training exercises are permanently off-limits.
“There are a number of ligaments that support the acromioclavicular joint,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Including the joint capsule as well as the coracoclavicular ligaments,” adds Dr. Oheb.
“In this case there is a likely tear of the AC ligament, but the CC ligaments are still intact and likely sprained. [A sprain is an injured ligament that is not actually severed or torn.] Once they heal there should be no restrictions.”

Freepik.com. pressfoto
This means that if you were deadlifting 400 pounds before your grade 2 AC separation, you can expect to eventually be deadlifting 400 pounds again.
As well as any of the following for max effort:
- Bench press
- Overhead press
- Bar dip
- Bent-over barbell row
- Rock climbing
- Chopping wood
This may take time with a grade 2 AC joint injury. Do not get ahead of yourself.
And while performing the deadlift, be sure to place the bar back onto the floor with control — rather than banging it to the floor, since having control is better for the shoulder and back structures.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/wavebreakmedia
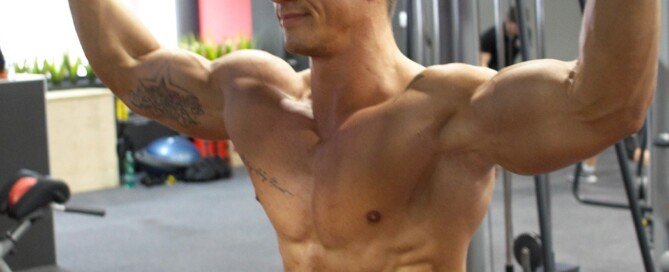
How to Get Back into Bodybuilding with Grade 2 AC Separation

If you suffer a grade 2 AC separation and are a bodybuilding enthusiast, you can expect to eventually resume your workout regimen once your injury heals.
However, you must be patient. You must not rush back into the bench presses, dumbbell presses, overhead barbell presses, dips, etc.
“In general, ligament tears and sprains can take up to 12 weeks to heal,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
Dr. Oheb adds, “I would recommend gradual progressive weight bearing after that.”
This means using a very light barbell for bench pressing, and small dumbbells for chest and shoulder pressing.
How Much Weight Are We Talking Here?
Just how much weight you should lift, once you are cleared to do this (after completing physical therapy exercises) will be determined by your previous level of strength.
Have you ever sprained an ankle? This is a ligament injury.
If you’ve ever experienced this, you know how long a bad sprain can take to heal before you’re running up and down hills again or sprinting across a parking lot in the rain without any discomfort or instability.
Even dashing up and down a single flight of stairs needs to be put on hold for a while when you have a sprained ankle.
And that’s without an actual severing of the ankle ligaments.
In a grade or type 2 AC separation, the ligament is actually severed, separating one part of the clavicle from the other, leaving a gap there — and that gap is permanent.
So you must be patient and not get ahead of yourself.
Sure, it stinks having to limit yourself to light weights, but in the long run you’ll be glad that you did.
As a bodybuilder, you may even suffer some “deflation” of your physique.
Be prepared mentally for this so that if you begin really noticing this, you’ll be in a better place mentally to continue with light weight workouts.
So if you keep things in perspective, you will regain your pre-injury bodybuilding status despite having a permanent grade 2 AC separation.