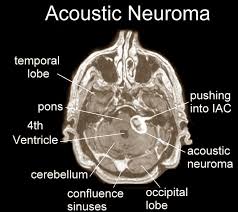
Best Procedure for Preserving Hearing in Acoustic Neuroma

There are different kinds of surgeries for acoustic neuroma treatment, and overall, the prognosis for preserving hearing is poor.
You may be wondering what is the best of these procedures – “best” being a relative term.
Researchers from the University of Michigan Medical School wanted to find out.
The study involved 73 patients who received procedures for their acoustic neuromas between 1999 and 2005.
This large time frame for so few patients exemplifies the rarity of the benign tumor.
The procedure studied is called MCF: middle cranial fossa—an approach from above the ear.
Three-fourths of patients who had useful hearing prior to this surgical procedure had a useful hearing level post-surgery.
The caveat is that, according to H. Alexander Arts, MD, the acoustic neuroma needs to be “small” to “have a good chance of preserving your hearing,” says the report in Otology & Neurotology (2006)
Another surgical procedure, as well, has the potential to preserve hearing: the suboccipital approach (from behind the ear).
But the researchers conclude that the MCF approach is better as far as less chance of injuring the hearing nerve.
Hearing Preservation Rates after Acoustic Neuroma Surgery Are Improving
• This study points out that when non-MCF procedures are used, there’s a 30 percent rate of preserved hearing.
• The middle cranial fossa approach is being used more often.
• MRI technology is catching more acoustic neuromas when they are small.
One of the study’s limitations, however, is it’s very small size: 73 suhjects.
Learning that you have a brain tumor is unsettling enough without having to stress over what surgical technique should be used, if you’ve been told that the mass needs to be removed.
“The success rates for preserving hearing and acoustic neuroma surgery really depends on the expertise of the surgical team rather than the particular approach,” says Ted McRackan, MD, MSCR, Director, Skull Base Center; Assistant Professor, Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina.
“There are data suggesting that the middle fossa approach has better preservation rates than the retrosigmoid approach, but whichever approach the surgeon is most comfortable with likely gives you the best chances of success.”
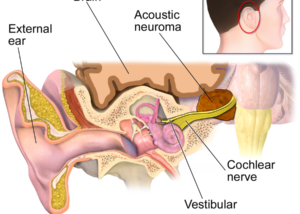
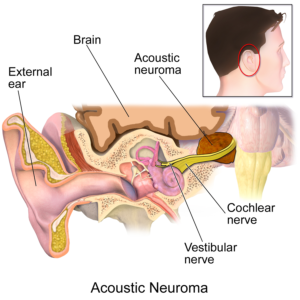
Acoustic neuromas are very rare. The most common symptoms are sudden tinnitus in one ear only, along with sudden hearing loss in that ear.
However, this symptom duo in only one ear almost always has a far more benign cause.
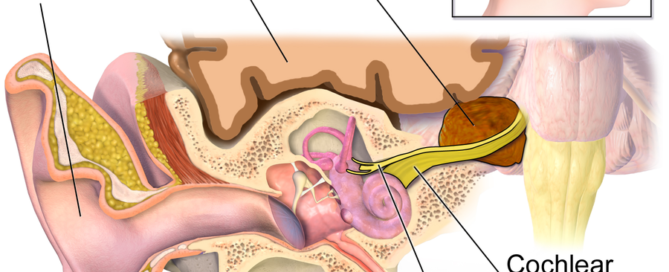
 In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2006/03/060306114450.htm
Is There a Drug that Can Stop Acoustic Neuroma Growth ?
The possibility that a common over the counter drug can stop or slow down the growth of an acoustic neuroma is very promising.
If you’ve been diagnosed with an acoustic neuroma, and your doctor has recommended “watchful waiting” rather than surgery or radiation, there’s a drug you should ask him about.
It is aspirin.
“There is some preliminary evidence showing that aspirin usage is associated with a decreased growth rate for acoustic neuromas,” says Ted McRackan, MD, MSCR, Director, Skull Base Center; Assistant Professor, Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina.
“However, the evidence is far from concrete and additional studies are being done to further evaluate this question.”
These studies on the same course as the one that’s reported from 2014 in Otology & Neurotology.
This study says that for the first time, use of aspirin has been found to correlate with halted growth of this very rare auditory tumor.
The research comes from Massachusetts Eye and Ear, Harvard Medical School, Massachusetts Institute of Technology and Massachusetts General Hospital.
Common Drug Seems to Slow Growth of Acoustic Neuroma
• Over 600 people with acoustic neuroma were analyzed for the study.
• There currently is no drug that is marketed as a deactivator to this tumor’s growth.
• But aspirin was shown to be promising in this study.
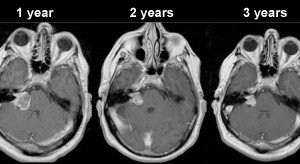
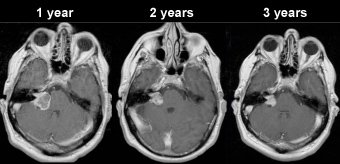
• The subjects, who took aspirin, were followed with multiple MRIs.
• A correlation was found between the subjects who took aspirin and the rate of growth.
The study shows that there is a “potential therapeutic role” of this drug in slowing down the growth of an acoustic neuroma, says Konstantina Stankovic, MD, in the report, leader of the study and an otologic surgeon.
The study did not look into whether or not a daily aspirin can actually prevent the initial development of an acoustic neuroma.
Daily aspirin use comes with the risk of internal bleeding.
Do not proceed with daily intake of aspirin without first consulting with your medical team.
That all said, this study is very good news for those who have been diagnosed with an acoustic neuroma, as the “headache drug” is very well-tolerated by most people.
A Subsequent Study
A study published in 2019 shows that aspirin had no effect on an acoustic neuroma’s growth.
It’s advised that patients keep current on the latest studies.
An acoustic neuroma is benign (cannot spread).
 In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Blausen.com staff
Source: sciencedaily.com/releases/2014/01/140124110705.htm
High Dose vs. Low Dose Radiation for Acoustic Neuroma Treatment
Higher radiation doses for acoustic neuroma can actually damage hearing, but are lower doses enough to destroy this tumor or at least stop it from growing more?
When radiation is used, the vast majority of these benign tumors do not grow back, points out Maria Werner-Wasik, MD., an associate professor of radiation oncology at Jefferson Medical College of Thomas Jefferson University, in a report.
Could lower doses of radiation treat acoustic neuroma as effectively as higher?
• The researchers compared two groups: 74 patients who received small but daily doses of radiation, and 41 patients who also received daily small doses—but smaller than in the first group.
• Local tumor control for both groups was the same.
• Toxicity to the fifth and seventh cranial nerves was the same in both groups.
• However, hearing preservation in the smaller-dose group was better.
“We think the lower dose level is associated with equally good local control and better hearing preservation,” says Dr. Werner-Wasik in the report.
Two additional benefits of the smaller doses of radiation are those of fewer visits and shorter treatment times.
Dr. Werner-Wasik also adds that similar results were found by other researchers.
Gamma Knife (targeted radiation) treatment is becoming more common for patients with acoustic neuroma, for which surgical resection causes permanent hearing loss for most patients.
Dr. Werner-Wasik aims to continue the research using even smaller doses of radiation for treating acoustic neuroma, which is a benign tumor.
It’s estimated that between 2,000 and 3,000 Americans are diagnosed every year with it.
What Kind of Doctor to See After Acoustic Neuroma Removal
“In modern acoustic neuroma surgery, the surgical team consists of a neurotologist and a neurosurgeon,” says Ted McRackan, MD, MSCR, Director, Skull Base Center; Assistant Professor, Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina.
“Depending on the practice setup, you may follow up with one or both of these physicians after surgery.”
 In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: sciencedaily.com/releases/2006/11/061108154942.htm
Acoustic Neuroma: Gamma Knife (Radiation) or Regular Surgery?
In plain English which is better for acoustic neuroma treatment: radiosurgery (pinpointed radiation on the tumor) or “under the knife” surgery in which the tumor is cut out?
If you’ve been diagnosed with an acoustic neuroma, you may already know that there are three main treatment options (besides surveillance):
• Radiosurgery (“cyber knife,” “Gamma Knife” or targeted radiation)
• Regular surgery (microsurgery)
• Transcanal surgery (not as common)
Karpinos et al made a comparison between radiosurgery and regular surgery for acoustic neuroma in 96 patients.
Gamma Knife vs. Surgery to Treat Acoustic Neuroma
• Between 1993 and 2000 the subjects were treated at Memorial Hermann Hospital, Houston.
• Subjects who had regular surgery had larger tumors and were younger when compared to the Gamma Knife group.
• Tumors were divided into small, medium and large.
Tumor Growth Control After Treatment
• 100 percent for regular surgery
• 91 percent for Gamma Knife
Measurable Hearing Preservation
• 57.5 percent for Gamma Knife
• 14.4 percent for regular surgery
Facial Neuropathy (problem with facial nerve)
• Development of facial neuropathy in the surgery group was “significantly higher” than in the radiosurgery patients.
Trigeminal Neuropathy (problem with cranial nerve)
• You guessed it: The surgery group had a “significantly higher” rate of neuropathy.
Miscellaneous
• Microsurgery patients had a longer hospital stay.
• Microsurgery patients had more perioperative complications (this means during and post-operative phases taken together).
The full report is in International Journal of Radiation Oncology (12/2002).
Conclusion
“The decision of whether to observe versus operate versus perform radiosurgery (Gamma knife) is complex and dependent on the patient’s age, symptoms (balance issues and hearing), tumor size and characteristics, and patient’s values,” says Ted McRackan, MD, MSCR, Director, Skull Base Center; Assistant Professor, Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina.
“The patient should discuss all options with his or her treating physician.” There is no one-size-fits-all template.
Acoustic Neuroma Risk Factors
One primary risk factor for this benign tumor of the inner ear is genetic predisposition.
Individuals with a rare genetic disorder called neurofibromatosis type 2 (NF2) are at a significantly higher risk for developing acoustic neuromas.
NF2 is an inherited condition characterized by the growth of noncancerous tumors on nerves, including those associated with hearing and balance.
Another potential risk is exposure to environmental factors, though this connection is less well-established.
Some studies suggest that prolonged exposure to certain environmental toxins or radiation may play a role in the development of acoustic neuromas, but more research is needed to confirm these links.
Age and gender also influence risk. Acoustic neuromas are most commonly diagnosed in people between 30 and 60, and they tend to occur slightly more frequently in women than in men.
However, the reasons for these demographic patterns are not yet fully understood.
 In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: redjournal.org/article/S0360-3016(02)03651-9/abstract
How Heavy Should a Woman Lift Weights for Workouts ?

Women who are new to strength training — lifting weights — may wonder just how much they should lift for their gym workouts.
The rule of thumb for women is the same as for men, if you’re thinking in terms of safety. (more…)
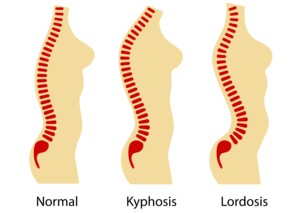
Why Is Dr. Nowzaradan of 600 Pound Life Always Hunched Over?

Ever notice that “Dr. Now” on “My 600 Pound Life” has a hunchback?
Are thousands of hours hunched over during surgery the cause of Dr. Nowzaradan’s hunched back?
Or is Dr. Now’s perpetual hunching over just bad posture?
• It’s not bad posture.
• It’s not caused by thousands of hours performing surgery.
• If it were caused by all the surgery he’s performed, why aren’t most other surgeons — especially those over 60, afflicted with this condition?
The condition that makes Dr. Younan Nowzaradan “hunch over” is called kyphosis.
I sent the photo of Dr. Now in this post to Justin J. Park, MD, a board certified orthopedic spine surgeon with The Maryland Spine Center at Mercy Medical Center in Baltimore, MD.
Dr. Park explains, “Although ‘hunching over’ or development of kyphosis is a natural part of aging for both men and women, I think that the man in the photo has a more severe form of kyphosis that is not part of natural aging.
“He may have a condition called Scheuermann’s kyphosis. It often develops in adolescence and can be a cause of back pain.”
Kyphosis is an abnormal curvature of the upper spine and has nothing to do with bad posture.
Shutterstock/Nemanja Cosovic
“Kyphosis is a result of disc degeneration and vertebral body collapse that leads to the deformity,” says Dr. Park.
“Because it is a structural condition, people can’t ‘just straighten out’ from it.”
When they lean over or bend over, the curvature, or the so-called kyphotic curve, becomes more pronounced.
In Dr. Now’s case, we don’t know for sure what the cause is, but he clearly has kyphosis.
Scheuermann’s disease is a malformation of the spine that begins after puberty.
The treatment for Scheuermann’s is a special back brace applied to the young patient who’s still growing; this may arrest progression of the rounding of the upper back.
However, Dr. Park says, “Unfortunately, bracing for kyphosis oftentimes is not effective in preventing further deformity.”
 Dr. Park’s advanced surgical techniques allow him to perform precise and delicate surgeries. He offers the latest in degenerative spinal fusion, minimally invasive surgery, spinal trauma and complex spinal deformity correction.
Dr. Park’s advanced surgical techniques allow him to perform precise and delicate surgeries. He offers the latest in degenerative spinal fusion, minimally invasive surgery, spinal trauma and complex spinal deformity correction.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
“My 600 Pound Life: The Enablers’ Story”

More attention must be given to the disenchanted souls on “My 600 Pound Life”: the enablers!
One of the recurring themes among the people who enable (bring huge amounts of food to) a person with super morbid obesity is, “I love her; how can I say ‘No’?”
Viewers are incessantly stunned by these types of comments straight from the mouths of the enablers — who may be the spouse, significant other, parent, child or even sibling of the super morbidly obese man or woman who’s bed- or chair-ridden due to their size.
There are many things in life that are incredibly difficult to do. Saying “No” to your 600 pound family member should not be one of them — when it’s literally a matter of their life or death.
TLC’s “My 600 Pound Life” follows the stories of people in their 20s to 50s who weigh at least 600, but sometimes over 750 pounds.
Many enablers are spouses or significant others.
I’ve watched every episode of “600 Pound Life” thus far. A common scenario is that a man marries a woman who weighs around 400 pounds — but over time, she gains even more weight.
Less common is a woman who marries a man of this weight, then post-marriage he gains and she enables, and it’s a vicious cycle.
The eating-disordered spouse (or significant other) continues gaining weight until she or he is rendered either virtually non-functional or semi-functional.
The able-bodied spouse continues to bring the 600 pounder food in gigantic quantities.
How much blame should we place on the enablers in “My 600 Pound Life”?

Dr. Younan Nowzaradan, the bariatric surgeon featured on “My 600 Pound Life,” has passionately called out enablers on quite a few episodes.
He clearly places some of the blame on the enabler. This is obvious when he first meets the patient and the enabler with him or her.
One enabler, the mother of the subject, even explained that there was no point in saying “No” because her daughter was capable of obtaining the food anyways.
Don’t these enablers realize that saying “No” can mean the difference between 600 and 500 pounds?
Perhaps over time, refusing to play the role of enabler would help the subject lose some weight — and “some” is better than continuing to gain.
Weighing 500 pounds is dangerous, but not as dangerous as 600 pounds.
Is It an Issue of Will Power with the Enablers?
It’s a defeatist approach, bringing the food because “She’ll get it anyways.”
She—or he—if severely compromised by all the body weight, will NOT always get the same amount of food “anyways.”
It would be too painful to “anyways” get the same amount of food.
• It takes all of their might just to get into a car.
• It takes all their energy just to walk from bedroom to kitchen.
• It’s logical to conclude that without the enabler feeding them, these subjects would actually consume FEWER calories.
If the enabler stopped enabling, a severely incapacitated overeater would be forced to, for example, consume 15,000 calories a day rather than 20,000.
Several thousand calories less per day would result in weight loss — and again, 500 pounds is not as bad as 600 pounds.
- So 3,500 calories = one pound of fat.
- If someone normally eats 20,000 calories a day, then drops to 15,000 because the enabler is no longer bringing them food, the weight loss will be rapid…AT FIRST.
But they won’t keep losing 42 pounds indefinitely at 15,000 calories per day.
There will very soon be a plateau, because 15,000 a day is enough food for seven adults.
But as mentioned, SOME weight loss is always better than staying at the same gargantuan weight, let alone continuing to gain fat.
But won’t the weight loss make the subject more mobile and hence, more able to get up and cook big meals?
Most likely this is exactly what would happen, and they would be right back up there at 20,000 calories/day — and start gaining.
However … this likely outcome should never be used as an excuse for enabling the individual!
Furthermore, dropping 50 pounds JUST MIGHT spark motivation in the subject to continue trying to lose weight.
The enablers on “My 600 Pound Life” will never be able to come up with a logical, rational, understandable excuse for their behavior — at least none that Dr. Nowzaradan accepts.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Stronger, Tighter Abdominal Muscles with 3 Core Routines

For tighter and stronger abs, do the following core exercise routines for these muscles.
Not only are these great ab routines, but it’s very important to follow these instructions so that you have the correct form.
Bad form, while performing ab exercises, will sabotage your attempts at getting stronger, tighter abdominal muscles. (more…)
Numbness on ONE Side of the Nose: Causes Include Tumor

Numbness on one side of your nose is an alarming symptom if you have no idea why it’s there, such as a recent blow to the nose or cosmetic surgery (rhinoplasty).
This post doesn’t focus on global or even-sided numbness, but numbness on one side (unilateral) of the nose. Oddball symptoms like this often make people suspect a tumor. (more…)
Can Listening to Live Band Music Damage Your Hearing?

Don’t people realize that sitting on the deck of some bar & grill to listen to the live band music will damage their hearing?
The people who do this tend to do it on a regular basis, and it’s that cumulative exposure that puts them at high risk for permanently dulled hearing. (more…)