Barbie Now Has a Realistic Body, but Her FACE Is Unrealistic!

It’s supposedly a big achievement that the Barbie doll body now comes in a curvy or “realistic” version—yet her face remains totally unrealistic. (more…)
Contraindications for Ventricular Assist Device in Heart Failure
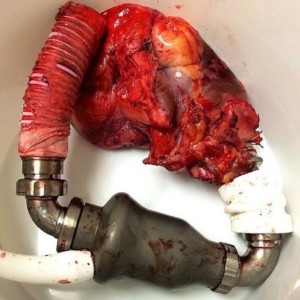
It would seem that most patients with advanced heart failure who are getting worse would be suitable candidates for a ventricular assist device. (more…)
Cardiorenal Syndrome Death: Would Sooner Intervention Matter?

If someone with chronic heart failure goes into acute decompensated mode triggering cardiorenal syndrome and dies, is there a sooner point in time for which medical intervention could have saved this individual? (more…)
Does Ejection Fraction Decrease with Acute Heart Failure?

How can doctors tell that ejection fraction has worsened over the course of a few days in someone admitted with acute decompensated heart failure if only one echo was taken on the day of admission? (more…)
What Contraindicates Drug Therapy for ADHF & Worsening Kidneys?

The contraindications for drug therapy in critically ill patients with acute decompensated heart failure with worsening renal function leave physicians in a very tough spot, because without these drugs, the patient is sure to die. (more…)
Cardiorenal Syndrome in Elderly: Who Gets Drugs, Who Doesn’t?

What determines when drug treatment in the elderly with acute heart failure and worsening renal function can be helpful vs. harmful?
Cardiorenal syndrome has no clear-cut cookie-cutter treatments. (more…)
Can Gym Workouts Offset Blood Clot Risk from Watching TV ?

Bad news for workout enthusiasts who watch a lot of TV: Your gym exercise may not cancel out the blood clot risk of sitting a lot in front of the TV.
Now if you walk on a treadmill during most of your TV viewing, or otherwise are on your feet, then you need not worry about a heightened risk of developing a blood clot — also called a deep vein thrombosis.
However, most people, including those who engage in regular gym workouts, spend most of their TV viewing time sitting.
Study Shows this Again
A study led by Yasuhiko Kubota (Springer’s Journal of Thrombosis and Thrombolysis, Feb 2018) says that excessive sitting increases the risk of blood clots whether you’re sedentary or exercise.
Prolonged sitting can lead to DVT via impairing normal circulation in the legs and feet.
Kubota, from the University of Minnesota, analyzed data from 15,189 Americans 45 to 64.
Beginning in 1987, participants were asked about their health, exercise habits, if they smoked or if they were overweight.
Type of exercise was not specified. It’s fair to wonder how many were bodybuilders, mountain climbers, martial artists and marathon runners vs. more recreational level exercisers.
Over many years the participants were followed, being asked if they’d received any hospital treatment.
Hospital records and imaging tests were analyzed. There were 691 DVT related incidents up to the year 2011.
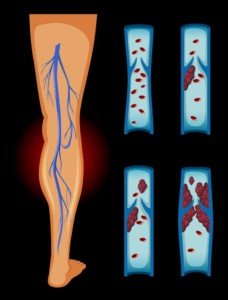
Blood clot in leg. Source: Vecteezy.com
Exercise Doesn’t Undo TV Sitting Time: Blood Clots Still Happen
• Participants who watched TV often had over 1.7 times the risk of a venous thromboembolism compared to participants who never or only occasionally watched TV.
• Body weight and exercise habits were adjusted for, yet this increase risk of DVT persisted.
This study, as well as similar analyses, begs the question:]
Is there an increased risk of DVT from excessive sitting in people who KILL it at the gym?
What exactly is exercise?
Having been a fitness professional and enthusiast for years, I am very well aware that when people are asked if they “exercise,” many will unknowingly inflate the answer.
For example people might consider it exercise to walk a tiny dog a few times around a block or do housework.
But what about DVT risk in people who, for instance, do CrossFit or regularly do high intensity interval training, grueling five mile hikes or train for powerlifting competitions?
Hopefully, studies that focus on strenuous exercise will be carried out in the near future.
Tips on Sitting Less While Enjoying TV
- Is there room for a treadmill so you can walk while watching TV?
- Take up yoga and do it while watching TV.
- Do shadow boxing or karate kicking.
- March in place, do kettlebell swings, planks, squats, ANYTHING to keep your butt off the cushion.
- You can also stand in pretty much one spot while watching TV. You don’t have to exercise during the program, but inserting some exercises will add value to your overall fitness regimen.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com, pressfoto
Source: sciencedaily.com/releases/2018/02/180221122555.htm
Fasting Glucose Always in the 90’s: Why You Should Worry

Is a fasting blood sugar that’s always in the 90 range as good as always in the 80’s or 70’s, or does this mean you’re at higher risk for eventually developing type 2 diabetes? (more…)
Dangers of Double Dose of High Blood Pressure Drug

There is good reason never to double up on a drug for high blood pressure if you miss a dose.
“Double dosing on hypertension drugs can be potentially dangerous (even fatal), but most often, there are no significant results,” says Stacy Mitchell Doyle, MD, resident physician of FoodTherapyMD and long-time advocate of plant-based nutritional protocols.
“What can happen is the combination of several factors: Your age (elderly people don’t tolerate drops in pressure as well as younger people), the dose of the medication, what your initial pressure was before you took the extra dose, and what the actual medication is,” explains Dr. Doyle.
“For example, if you took too much of a beta blocker medication, your heart rate can drop to dangerously low levels which can cause syncope (passing out) or even heart block or heart attack.
“If you take too much medication and feel dizzy, weak or have pains in your chest, seek medical attention right away.”
If side effects or missing doses of your high blood pressure medication worry you, consider the idea of weaning off the drug (with your prescribing physician’s approval) and controlling your blood pressure via natural means – mainly, a change in diet.
A switch from the standard American diet (appropriately abbreviated as SAD) to a plant-based diet that restricts processed foods, may very well move your blood pressure from the hypertensive range to the normal and even low-normal range.
By focusing on whole foods like fruits, vegetables, whole grains, nuts and seeds, you reduce your intake of sodium and processed foods, both of which can contribute to high blood pressure.
Plant-based diets are naturally high in potassium, fiber and antioxidants, which support healthy blood vessels and better overall heart health.
Studies have shown that adopting this type of diet can lead to significant reductions in both systolic and diastolic blood pressure.
In addition to dumping the SAD way of eating, an exercise program of aerobics and strength training will also lower baseline blood pressure.
Sure, it’s easier to just take a pill every day, but wouldn’t it be nice to have naturally low baseline blood pressure along with a stronger, fitter heart, lungs, muscles and bones?
 FoodTherapyMD™ is the brainchild of Dr. Mitchell Doyle and recognizes that phytonutrients, the substances that make plant food so amazing, can be tailored to fight specific disease states.
FoodTherapyMD™ is the brainchild of Dr. Mitchell Doyle and recognizes that phytonutrients, the substances that make plant food so amazing, can be tailored to fight specific disease states.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sirtravelalot
Fasting Glucose Reading of 119: How Dangerous Is This?

It’s not health anxiety if you keep worrying about your fasting blood sugar being around 119.
Because if you keep seeing 119, you’re in big trouble – and your excessive worrying is quite justified. (more…)