Esophageal Cancer Misdiagnosed As Anxiety in a Woman
Pain or trouble swallowing, food getting stuck in your throat or chest, can be esophageal cancer.
Clever Ways to Beat College Peer Pressure to Drink & Smoke
Are you in college and feel pressure to drink and smoke?
Perhaps the pressure is your own stress, or maybe it’s new friends or just the general atmosphere. (more…)
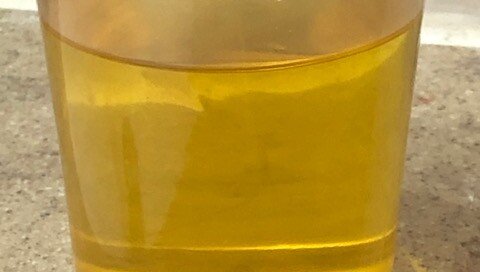
What Makes a Man Urinate in Cups or Bottles?
Do you have a roommate or husband who regularly pees in cups or bottles, and worse yet, lets them accumulate?
Is this laziness or mental illness? (more…)
Explosive Watery Foul Diarrhea with IBS: Misdiagnosis Possible
If you’ve been diagnosed with IBS due to daily explosive, watery smelly diarrhea that comes with little warning, you might not have IBS after all.
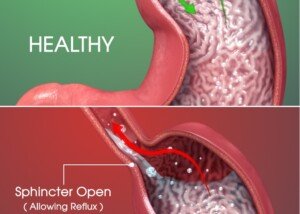
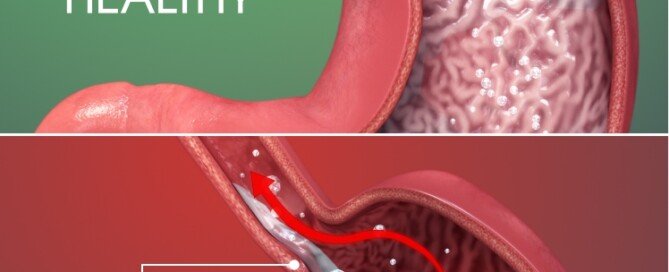
Why Can GERD Cause Chest Pain 2 Seconds After Swallowing Food?
You have no problem swallowing food but two seconds later, you feel a very brief pain or pressure in your chest.
Why Can GERD Cause Pain in the Right Upper Abdomen?
Pain in the upper right abdomen can be from GERD, though this isn’t one of the more likely causes of discomfort in this area. (more…)
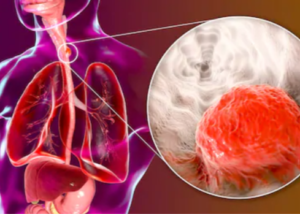
How Long It Takes GERD to Turn into Esophageal Cancer?
GERD can lead to esophageal cancer.
But how long does it take for the chronic acid reflux to turn into this very deadly cancer? (more…)
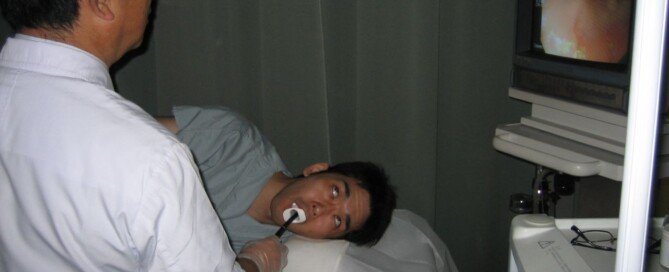
Routine Upper Endoscopies for Esophageal Cancer Screening for All?
If colonoscopies are recommended for routine colon cancer screening, why aren’t upper endoscopies advised for routine esophageal cancer screening?
How Long Does It Take Chocolate to Trigger Acid Reflux?
You’re a chocoholic and will never give up this heavenly food to prevent acid reflux.
So maybe you’re wondering how long it takes chocolate to trigger it. (more…)