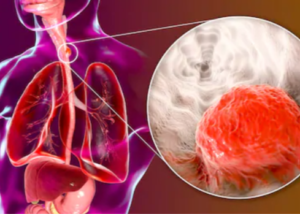
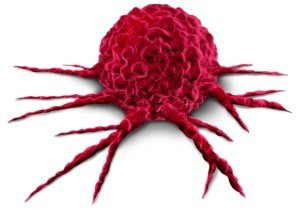
Trouble Swallowing Food: Anxiety or Esophageal Cancer?
Is there a way you could tell if your trouble swallowing food may be esophageal cancer rather than anxiety? (more…)
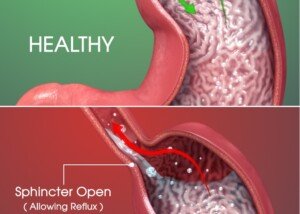
Weightlifting Guide: Nissen Fundoplication for Hiatal Hernia
Did you have a Nissen fundoplication for hiatal hernia and are confused about weightlifting guidelines?
Strength training, bodybuilding & powerlifting require clear, concise guidelines that should not leave the patient wondering, guessing or interpreting the wrong way.
Right Chest Pain After Upper Endoscopy: Causes, Solutions
You had an upper endoscopy earlier in the day yet still have right chest pain or chest pain in general.
Morbidly Obese COVID Survivor Feels Fat Shamed by Hospital Staff

A morbidly obese COVID survivor has accused frontline heroes of fat shaming when she was in the ER and then COVID unit.
Cindy on My 600 Pound Life: Seana Vibes but Worse
Cindy on “My 600 Pound Life” shows serious Seana vibes and an even bleaker future.
Remember Seana from Season 2020? (more…)