What Makes My Gas Smell So Bad?

Pheeuw, do you have really bad smelling gas?
It’s been said that really foul smelling gas means that the offender is very healthy. Of course, this is just a crazy myth.
“Silent but deadly” has been used to describe the smell of human gas. I asked what makes flatulence smell so bad to Edward Cruz Paredez, MD, a board certified gastroenterologist based in La Jolla, CA.
First of all, just what are “farts” made of?
Dr. Paredez explains: “Flatus is made of nitrogen (N2), oxygen (O2), carbon dioxide (CO2), hydrogen (H2), and methane (CH4), which account for more that 99 percent of expelled intestinal gas.”
So what about flatulence, then, is responsible for its awful odor?

Shutterstock/pathdoc
Dr. Paredez continues: “The hydrogen sulfide and other compounds (mercaptan, butyric acid and carbonyl sulfide) make the released gases smell bad.
“Humans actually expel little methane compared to ruminants such as cows and sheep.”
There is another explanation yet, for why the gas of humans stinks so bad.
“Humans hold their gas in much of the day and allow longer periods of fermentation compared to most animals who pass gas every hour!” says Dr. Paredez.
“This is especially true with the modern workforce who work indoors in close proximity to other people (i.e., cubicle workers).”
Interestingly, a person may not even think that his own flatulence smells that bad.
But the odor from the flatulence coming from other people can just about knock him flat on his back.
“A change in diet or a medication can often trigger a period of particularly bad smelling gas,” says Dr. Paredez.
Some people have reported that cutting back on carbohydrates, especially the carbs that are found in processed food, results in less flatulence, and thus, less odor.
Some medical conditions can cause very foul smelling gas, such as irritable bowel syndrome and inflammatory bowel disease.
However, these conditions bring with them other symptoms that are difficult to ignore, such as diarrhea, change in appearance of stools, abdominal cramps and sometimes abdominal pain.
If you’re not able to trace your foul smelling flatulence to foods, then make an appointment with a gastroenterologist, who will then order some tests to see if there is a medical cause.
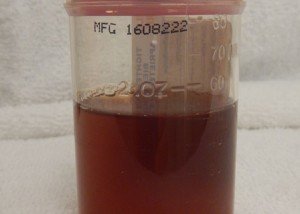
A stool sample test may be one of the tests ordered.
Your doctor may also recommend a colonoscopy, even if you’re in your 20s or 30s; colonoscopies are useful for detecting inflammatory bowel disease.

Dr. Paredez has been named a Top Doctor by San Diego Magazine and has also received a 2016 “People Love Us on Yelp” Award.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Aaron Amat
Painless Ongoing Diarrhea As Only Symptom: What This Might Be

Are you experiencing sudden diarrhea out of the blue for no apparent reason, and other than the diarrhea, you feel fine?
Is the diarrhea particularly watery or “liquidy”? Perhaps between episodes of this mysterious diarrhea, you feel perfectly normal, even quite fit and healthy.
What medical condition presents with sudden-onset diarrhea that then persists, and no other symptoms?
It may very well be microscopic colitis. However, it may also come with other symptoms: abdominal cramps, nausea and mild joint aches.
But painless diarrhea is the key symptom of microscopic colitis.
“The differential for painless diarrhea would include microscopic colitis, irritable bowel syndrome, cancer, food allergies or sensitivities, some infections, pancreatic insufficiency and medications,” says Alan Gingold, DO, a board certified gastroenterologist with Central Jersey Ambulatory Surgical Center.
“Microscopic colitis is a chronic inflammatory condition of the colon where the inflammation is at the cellular level and can only be seen by microscope.”
I’ve had microscopic colitis, and my gastroenterologist told me that this can be mild to severe.
In severe cases, a person may be having diarrhea many times a day and lose 30 pounds.
“The disease is broken down into two subtypes: lymphocytic colitis and collagenous colitis,” says Dr. Gingold.
“Usually presents in middle-aged females and presents as intermittent bouts of non-bloody diarrhea that typically comes and goes on its own.”
Men and younger women are not immune, though.
The symptoms of microscopic colitis can mimic the symptoms of an intestinal infection that’s limited to the intestines, versus an infection that goes body-wide and causes a fever.
My doctor initially diagnosed me with an intestinal infection — before he performed the colonoscopy.
Before the doctor entered the colonoscopy room, his nurse actually suggested that I had IBS — irritable bowel syndrome.
The nurse then thought that my diarrhea might have been caused by mental stress.
He told me that he himself suffered from diarrhea for two weeks following his divorce.
But I knew my diarrhea couldn’t have been caused only by stress, because it was not normal-appearing diarrhea.
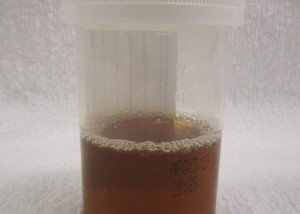
The diarrhea of my microscopic colitis was light brown, almost tan, and tended to assume a tinge matching the color of the foods I had eaten the day prior.
I saw chunks of food in these loose, flimsy stools
Sometimes the bowel movements were pure diarrhea, spewing out very easily and dispersing all over the place in the toilet water.
Other times it appeared to be in solid pieces, but then when I prodded the pieces with a cotton swab, they instantly dispersed. I saw food bits everywhere.
This was all the result of microscopic colitis, an inflammatory bowel disease.
The Cause?
“The underlying causes of microscopic colitis is unknown,” says Dr. Gingold.
“It may be due to an autoimmune condition — although chronic use of NSAIDs (e.g., Alleve) have also been suggested as a possible etiology.
“Because there are many other conditions that can present similarly, it’s a diagnosis made by taking a biopsy of the colon during an endoscopic exam by your gastroenterologist.”
Samples of the inner lining of the large colon are collected and sent to a pathologist.
This is why a colonoscopy is required to confirm microscopic colitis.
If you’ve been experiencing sudden-onset (though this is not always the case) diarrhea, particularly watery in nature, and especially if it contains food particles — and you have no other symptoms — you may very well have microscopic colitis.
But remember — only a colonoscopy can confirm this.
Microscopic colitis may resolve on its own for some individuals.
In severe cases, medications can be prescribed. Kefir may also relieve the diarrhea.
 Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
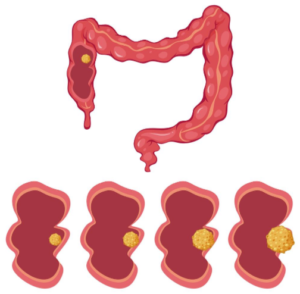
IBS (Irritable Bowel Syndrome) or Colon Cancer Symptom Comparison
Symptoms of IBS (irritable bowel syndrome) and colon cancer are nearly identical.
In fact, they are so similar that I had to wonder if there was a way that a person, who is experiencing troubling symptoms that fit the bill for IBS — but also for colon cancer — can tell at home the likelihood that his symptoms point more towards IBS than colon cancer, or .
.. dreadfully, point more towards colon cancer than irritable bowel syndrome.
The symptoms of irritable bowel syndrome are terrifying to anybody who experiences them and is familiar with the symptoms of colon cancer! They’re virtually the same!
Unfortunately, when it comes to if there are any ways that the patient at home can try to determine if his symptoms point more towards either irritable bowel syndrome or colon cancer:
“None — IBS is a diagnosis of exclusion and should only be made in my opinion after a full evaluation,” says Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
“Blood in the stool (obvious or found in fecal occult blood testing) always requires a structural evaluation (i.e., colonoscopy).”
Suppose a person develops IBS, but out of fear or lack of money, refuses to see a doctor.
Instead, he just hopes that the alarming gastrointestinal symptoms are indeed irritable bowel syndrome, vs. colon cancer.
He decides that as time goes on, if the symptoms don’t worsen, this makes it increasingly unlikely that it’s a malignancy.
He also decides that as long as new symptoms don’t arise, such as jaundice (possible sign that colon cancer has spread to the liver), that his condition is likely benign.
After a long enough time passage, with no worsening symptoms or unexplained weight loss, and still able to function quite well physically, a person in this situation may come to assume that whatever’s going on isn’t colon cancer.
After all, if a long enough time passage has occurred, he is likely to conclude that if it were colon cancer, it would have killed him already, or, at least, rendered him too sick to get out of bed.
This hypothetical situation will put the person through unspeakable anxiety.
Why not just get the colonoscopy for peace of mind, even if you have no insurance?
Dr. Jones explains, “All too frequently, patients have months or even years of symptoms attributable to IBS who are subsequently found to have colon cancer as the underlying cause.
“The ‘it’s better so I’m better’ strategy is not one I would recommend.
“Rather, if there are limited resources, I would seek out a public health care center or clinic and follow through with an evaluation by a health care professional.”
Warning: A person may very well have IBS, but then by sheer coincidence, develop colon cancer, and hence its symptoms.
A diagnosis of IBS should never make a person feel immune to colon cancer.
Too many people are walking around with a diagnosis of irritable bowel syndrome despite never having a colonoscopy to rule out some other cause such as colon cancer.
Dr. Jones says, “My recommendations are that if an improved high fiber diet, supplemental fiber and probiotics over 2-4 weeks do not improve symptoms, patients need evaluation by a digestive health professional.”
Anti-diarrheal or laxative agents should not improve symptoms of colon cancer.
“If we are going to catch some of these atypical earlier colon caners, we must lower the threshold for colonoscopic evaluation.
“And strongly consider lowering the age at which we begin the discussions about colon cancer signs, symptoms, family history, to age 40, with colonoscopies recommended at age 45 for all.”
The argument against this is that colonoscopy is an invasive procedure with risks, namely perforation of the colon.
This is rare, however. Another argument is that colon cancer is uncommon in people under 50, particularly 20s and 30s.
Of such patients, 15.1 percent are diagnosed between age 45 and 54, according to the National Cancer Institute as of 2021.
However, this low incident rate is of no consolation to these younger patients!
“I think this will be a hot topic ongoing in the future and like the new recommendations for breast and cervical cancer, will be debated in the public forum,” adds Dr. Jones.
“I favor finding the polyp and skipping the cancer. Previvor trumps survivor any day in my practice.”
IBS (irritable bowel syndrome) Symptoms
- Abdominal pain/cramping
- Feeling bloated
- Gas
- Diarrhea
- Constipation
- Alternating diarrhea and constipation
- Mucus in stool.
- Symptoms may not respond medical treatment.
Additional Symptoms
Change in stool caliber and consistency including stools that are hard, like pellets or pencil-thin.
After having a bowel movement, you may still feel incompletely voided. More symptoms: fatigue, backache.
Colon Cancer Symptoms
- A change in stool caliber and consistency — including pencil thin stools
- Diarrhea
- Constipation
- Alternating diarrhea and constipation
- Abdominal pain/cramping
- Gas or a bloated feeling
- Sensation of incomplete voiding after a bowel movement
- Fatigue without explanation
- Blood in the stool; may appear red, dark or like a gooey tar
- Leg pain is possible.
Blood in the stools or “tarry” stools is not common with IBS.
However, these symptoms don’t always occur with colon cancer, either.
Unexplained weight loss is another feature of colon cancer, but people with IBS can also experience weight loss from all the diarrhea.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings. Colon Cancer Prevention Project
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Dragana Gordic
Causes of Thin Narrow Stools Besides Colon Cancer
If your thin or narrow stools have you fearing colon cancer, there are other causes of narrow thin stools besides cancer of the colon.
A number of factors can determine bowel movement caliber (shape, texture, color, etc.), says Whitney Jones, MD, a national expert and frequent speaker on early-age onset colon cancer prevention, and Founder, Colon Cancer Prevention Project.
Dr. Jones explains, “Stool content (e.g., solids vs. liquids), the amount of time stool spends in the gastrointestinal tract (i.e., transit/motility), and the function of the anal sphincter are all known to be involved in this process.
“Alterations in stool consistency and a resultant ‘change in bowel habits’ are known symptoms of a number of disease processes such as inflammatory bowel disease, cancer, and irritable bowel syndrome.”
And the possible causes of narrow or thin stools don’t stop there.
Have you increased your fiber intake lately?
This can cause BMs to come out thinner than usual.
Have you been eating Olestra or anything with sorbitol?
Dr. Jones says, “Ultimately, any process that affects stool consistency (e.g. dietary changes,), bowel transit or motility (e.g. chronic constipation, medicines, inflammatory conditions involving the GI tract), and/or anal sphincter function (e.g., rectal cancers, trauma, and surgeries) could result in long narrow stools.”
Your BMs may even be on the narrow side on a normal basis, and you’ve only noticed recently because perhaps you read an article on colon cancer.
Schematic of colon cancer. Source: vecteezy.com
Dr. Jones stresses that what’s particularly important is whether or not narrow, thin stools are outside the norm for your typical BM appearance.
Don’t delay discussing any change in bowel habits with a gastroenterologist.
Though narrow, thin stools can result from colon cancer, this does not mean that if you have skinny BMs, you probably have colon cancer.
It’s actually most likely from a condition other than colon cancer. This includes diverticulitis.
In fact, it might even be from microscopic colitis, which I’ve had.
One day a very long BM came out and it was on the narrow side, more narrow than usual, but not what I’d consider as thin as or like a pencil.
What made the stool appear more narrow than usual, however, was perhaps its very long length.
I imagined it being segmented, and realized that if broken into thirds or fourths, it wouldn’t seem as “narrow.”
It just so happened that this particular BM didn’t break up upon hitting the water.
Dr. Jones explains, “Regarding the caliber of stool and its correlation with the presence of left sided colon cancer, the data currently available does not necessarily indicate that narrow stools should alert patients or physicians of a possible malignant process.
“The notion that left sided colon cancer or rectal cancer often presents with narrow stools is based upon the anecdotal opinion of expert physicians of the late 19th/early 20th century.”
Dr. Jones adds: “There are no prospective studies and only a few retrospective studies in the literature that indicate that long narrow stools are correlated with cancer.
“This conception has been propagated throughout the medical literature mostly based on tradition.”
Most early colon cancer presents with no symptoms.
This is why there’s the extreme importance of getting screened for this killer with a colonoscopy.
This should begin at age 45 for people at average risk (due to age) for the disease, and then done every 10 years, unless otherwise indicated by the physician.
Anal cancer, which is rare, can also cause “narrowing of the stools,” according to the American Society of Colon and Rectal Surgeons.
 Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings.
Dr. Jones’ practice interests include prevention and treatment of colon cancers, pancreatic disease and biliary disease. He has authored numerous scientific articles, reviews and abstracts and presented at a variety of national and international scientific meetings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/sasha2109
Sources: Dig Dis Sci (2009) 54:208-211; fascrs.org/patients/disease-condition/anal-cancer
Causes of Blue and Green Urine, and Solutions

Ever have blue or green urine?
Gee, what causes urine to be green or blue or blue-green?
I asked Dr. Courtenay Moore, MD, urologist in the Glickman Urological & Kidney Institute at Cleveland Clinic, about what can cause your flow to turn blue or green.
Dr. Moore explains: “Certain medications can cause blue urine. For example, IV administration of methylene blue can cause both urine and feces to be discolored in this manner.
“Other medications that can result in blue urine include: Urised, amitriptyline, indomethacin (Indocin), cimetidine (Tagamet), and phenergan.” Another medication is Trac Tabs.
Additional Medications that Can Turn Urine Blue
– Triamterene, a mild diuretic.
– Rinsapin, an antibiotic. This can also cause your excrement to turn green.
– Viagra
– Any other medication that has a blue dye in it.
Additional Causes of Blue Urine
Multivitamins, excess B vitamins, and food dyes. Best bet: avoid eating foods that contain dyes. The body does not need artificial colorings in it.
Medical Problems that Can Cause Blue Urine
– Dr. Moore says, “A medical condition called familial hypercalcemia, also known as blue diaper syndrome, because children with the disorder have blue urine, could also be the source of the discoloration.”
– Another medical condition, called indicanuria, can be a culprit.
– And yet another medical problem is infection by the bacterium called pseudomonas.
Specific Causes of Green Voiding
– Dr. Moore says, “The likely source of green urine is a food source, such as asparagus.”

Freepik.com, timolina
– Additional causes: propofol, an anesthetic;
– According to urinecolors.com, there are no known diseases that would cause green fluid output.
However, according to urology.stanford.edu/about/articles/abnormal_urine.html, green urine can, indeed, be caused by a medical problem: “…caused by bile when there is a fistula between the urinary tract the intestines.”
Nevertheless, the good news is that cancer does not cause green or blue excrement.
Best Way to Monitor Urine Color
Obviously, men can do this more conveniently than women. Women can view the color of their urine on tissue paper after they wipe themselves.
But don’t wait till then, however, especially if the tissue paper is colored or textured. Women can view their fluid-void by observing the voiding action.
Make sure the lighting is adequate and you are positioned in a way that allows a good view.
For best viewing for both men and women, void into a clear plastic cup.

If one is not available, make sure that the toilet bowl is clean and free of any cleaning agents that add color to the toilet bowl water.
Make sure the lighting is adequate.
Should you decide to seek medical consultation, see a urologist.
If your medical plan requires an initial visit with a primary care physician, ask for a referral to a urologist.
A doctor will perform tests to determine any medical causes of color changes.
Dr. Moore’s clinical interests include voiding dysfunction, incontinence, female reconstructive surgery and female sexual dysfunction.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/PORTRAIT IMAGES ASIA BY NONWARIT
Source: urology.stanford.edu/about/articles/abnormal_urine.html
What Blood in Urine Means
Red Urine Has Many Causes: Some Life Threatening, Some Harmless
Red urine sometimes means blood in the urine, but sometimes it doesn’t.
Either way, you need to find out the cause of red or rust colored urine.
Some causes of red/blood in the urine are serious, including cancer; while some causes are quite benign (harmless).
These include repeated jarring from exercise. This happened to me some years ago when I was pedaling super furiously on a stationary bike, jostling it around: equipment I normally didn’t use.
A visit to the restroom right after revealed blood stains on my panties, but no blood or red in the urine, nor any red staining after that visit.
“Any trauma, regardless of how seemingly trivial, may cause bleeding within the urinary tract,” says Andrew Stephenson, MD, Section Chief and Director, Urology Oncology; Professor (PAR), Department of Surgery, Division of Urology, Rush Medical College.
“Gross (visible) blood in the urine after trauma is a reason to seek medical attention.”
What do these symptoms really mean?
Dr. Stephenson explains, “Microscopic blood cells in the urine is very common and may not be associated with any disease process within the urinary tract — about 5-10 percent of patients with microscopic hematuria (blood in urine) will have an identifiable cause (e.g., kidney stone, bladder cancer, etc.).
“Gross [visible] blood in the urine is usually associated with urinary tract pathology (e.g., kidney, bladder or prostate disease) or stones or infection.

Visible blood in urine can cause a tea or cola color, as well as an orange-red color. Credit: James Heilman, MD/CreativeCommons
What percentage of people who have kidney/bladder/prostate cancer, have this symptom?
“Blood in the urine from prostate cancer is uncommon in the absence of advanced disease,” says Dr. Stephenson.
“Most patients with bladder or kidney cancer will have microscopic blood cells present in the urine.”
Is this a very rare, or very common (or some range in between) symptom of kidney/bladder/prostate cancer?
“Three to five red blood cells per high-powered field on microscopic examination of the urine on more than one occasion is an indication for further investigations.”
How often or what percentage of diabetics have the symptom?
“Very uncommon in the absence of infection.”
Is this a common symptom of kidney stones?
“Yes. Also, abdominal pain or flank pain will be present if the stone has passed from the kidney into the ureter.”
More Additional Causes
Red Color but no Blood
Porphyria — a skin and nervous system disease
Beets, blackberries, rhubarb pie
Ex-lax and other laxatives
Some prescription drugs including antipsychotics (Thorazine)
The anesthetic Diprivan
Chronic poisoning from mercury or lead

Urine color affected by beets. Jmarchn/CC BY-SA 3.0
Blood
Strenuous exercise in addition to fierce stationary bike pedaling, such as distance running and jumping drills.

Distance runners are most at risk, but those who do any strenuous exercise involving the lower body can have urinary bleeding.
Urinary tract infections
Cancer of the kidney or bladder (occasionally)
Visible hematuria in children can be caused by a kidney inflammation from a viral or bacterial infection.
See a doctor when:
1 Two or more incidents of the symptom occur, regardless of time lapse in between.
2 Visible hematuria lasting beyond 24 hours
3 Urine color changes are not triggered by medications, dyes or food.
 Dr. Stephenson’s clinical and research focus is the treatment of prostate, bladder, kidney and testes cancer. He has published over 100 articles in peer-reviewed journals.
Dr. Stephenson’s clinical and research focus is the treatment of prostate, bladder, kidney and testes cancer. He has published over 100 articles in peer-reviewed journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Eag1eEyes
Brain Zaps from Cymbalta, Effexor and Paxil Explained

Brain zaps from Effexor, Cymbalta and other antidepressants are as follows:
“Electrical currents” or “shivers” that run through your brain when you try to get off Effexor, Cymbalta or Paxil, three commonly prescribed antidepressants, notorious for causing withdrawal brain zaps.
Ever wonder why, however, antidepressant drugs like Cymbalta, Effexor and Paxil create the brain zap sensation in the first place?
Brain zaps from trying to get off Effexor, Cymbalta and Paxil: What’s going on?

“There are no definitive answers to this question, only postulates or theories, so my answer is pretty short – as are the theory explanations in the literature,” explains Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
“The so-called ‘brain zapping’ is most prevalent when antidepressants are abruptly discontinued without any tapering whatsoever, and is most common with the antidepressants that have the shortest ‘half-lives.
“Half-life is defined as the amount of time it takes for 50 percent of any drug molecule – from peak plasma levels – to be excreted from the system.
“With this in mind, brain zapping discontinuation syndrome would be most prevalent with Paxil, Effexor, Cymbalta, and to some extent Zoloft.
“There is little if any discontinuation effects with Prozac due to its very long half-life of seven days.
“My thinking is that when the aforementioned antidepressants are stopped, sudden decreases in norepinephrine, serotonin and possibly dopamine levels cause an interruption in signaling capabilities in the brain’s limbic system.
“This interruption in signaling causes a neuropathy of sorts, which manifests itself as shock sensations in the extremities (hands and feet in particular) as well as the brain zapping.
“These withdrawal effects are much worse upon abrupt discontinuation, but they also occur with tapering.”
Some people abruptly stop taking Effexor, Cymbalta and Paxil, often for side effects, and/or because these antidepressants didn’t relieve depression symptoms.
Such individuals should not be surprised, then, that they get brain zaps.
Though brain zaps can result even when tapering off Effexor, Cymbalta or Paxil, it’s possible that in some people, brain zaps would occur only from abruptly quitting these antidepressants, and not from a gradual tapering off.
When it’s time to go off the antidepressants Cymbalta, Effexor or Paxil, either due to side effects or because you believe you’ve conquered your major depression, consult with your prescribing physician (or new physician if your insurance plan changes) about tapering off to minimize brain zaps.
 Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Twitching Calf Muscle Strength Tests and ALS Obsession

Are your calf muscles twitching?
Are you scared it’s ALS?
How can you tell this isn’t ALS?
Even if you had a negative EMG, you may still not be reassured and may be continuing to obsess about twitching calf muscles.
If you’re scared you have ALS due to twitching calf muscles, here are strength tests that, if you pass, should be of reassurance.
Are your calf muscles twitching?
Are you scared it’s ALS?
Even if you had a negative EMG, you may still not be reassured and may be continuing to obsess about twitching calf muscles.
Or, worse yet, perhaps you have no medical insurance and can’t afford to pay out-of-pocket for an EMG.
Strength tests for muscles will help tremendously in dissolving fear of ALS.
If you struggle at all but ultimately complete the exercise, do NOT let the struggling cause panic.
When I was a personal trainer I deliberately had my gym clients perform exercise routines that made them struggle.
So if there’s struggling, it’s likely because of the exercise itself, plus anxiety and being out of shape.
If a person has a pathological foot drop, that individual will not be able to perform these exercises, period. (You probably already know how a “foot drop” relates to ALS.)
This test is not about a perfect, flawless performance. It’s about completing the exercises regardless of skill level.
A person will either complete them or won’t. Never mind how long it took, how many attempts it took or how difficult it was
Calf Strength Test #1
Stand at top of staircase (or any steps), but backwards. Walk down staircase backwards and very slowly, but with each step, place only the ball of foot on the stair. Do not place hands on anything for support.

Each time you place foot on stair, hold position for three full seconds before proceeding down to next step. Expect some struggling; this requires agility.

You’ll find it easy to imagine that a person with ALS affecting calf muscles will not even be able to support their down-coming weight as they place it on the ball of their foot; these muscles control this joint action, not foot muscles.
Expect balance challenges. But if you can make it down just one stair on the ball of your foot, backwards, consider this completion of the test, even though you might lose balance on all the other stairs.
Repeat this test, because the second time won’t be as tricky.
With enough repetitions of this calf muscle strength test, you will eventually make it down every step, on the balls of your feet, holding out for three seconds, without much struggle.
There will be a learning curve and progress, something you will not be able to imagine a person with ALS affecting their calf muscles will experience.
So if progress took half the day before you finally made it down all stairs without losing balance, consider yourself successful.
Calf Strength Test #2
Jump for one minute with a rope, or if one isn’t available, move your hands and arms as though you’re holding one.

Freepik.com
A healthy person will not detect an aberration with the suspect leg; instead, the healthy person’s foot will cooperate and will have the spring of the other foot.
If you feel exhausted after one minute, this means that more aerobic exercise is in order (your heart needs more training), and hence, there’s no reason to fear ALS over this particular feature.
If your calf muscles are burning after one minute, this is normal. A person without ALS affecting calf muscles should be able to jump rope cleanly, even if the calves burn.
Calf Strength Test #3
If it’s your right calf muscle twitching, ask yourself if you had any problems driving today.

Shutterstock/Electrical Engineer
Remember, movement of the foot down against an object, such as a car pedal, is controlled by calf muscles.
The foot must continuously alternate between pressing downward and then releasing the pedal.
This may seem simple and not even seem like a strength test, but calf muscles are working to control these precise gas pedal movements.
A healthy muscle can do this, and if yours did today, don’t panic about ALS.
Calf Strength Test #4
Stand only on the foot of the calf in question. Go up on toes, still just on this foot, while the other foot is off the floor.
Stay up for 10 seconds, then release. For extra reassurance, hold the up position for 30 seconds or stand on an unstable surface.

Shutterstock/Jacob Lund
Calf Strength Test #5
Hop across the room on one foot. A person without ALS foot drop will have no problem doing this.
In addition, “I would also include walking on your heels and toes (this is a part of the neurologic exam and is used to test strength),” advises Mitzi J. Williams, MD, clinical neurologist with Morehouse School of Medicine and clinical advisor for the Multiple Sclerosis Foundation.
“If you are concerned about new neurologic symptoms, seek medical attention,” adds Dr. Williams.

Dr. Williams is author of “MS Made Simple: The Essential Guide to Understanding Your Multiple Sclerosis Diagnosis,” available on Amazon. She is a member of the American Academy of Neurology.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Anut21ng Photo
Sources.: mayoclinic.com/health/amyotrophic-lateral-sclerosis/DS00359; aboutbfs.com
Do You Fear ALS Because Your Muscles Are Twitching?
Muscle twitching is a terrifying topic for many people because twitching muscles is a symptom of a killer disease.
Muscle twitching is very common, affecting millions of people, but ALS, the disease in which muscle twitching is a symptom, is extremely rare.
Nevertheless, a person with twitching muscles may become vulnerable to a terrifying hypochondria in which he or she thinks they have fatal ALS whenever a muscle twitches.
But muscle twitching is a fact of life.
As I type this, my triceps muscle is twitching away. I pulled my sleeve up and watched. Boing, boing, boing, like there was a beating heart below my triceps muscle.
But am I scared I might have ALS?
No. It’s no coincidence that two days ago, I put my triceps muscles through a punishing weightlifting routine.
Two days out from grueling weight workouts often results in strange things, like muscle twitching.
If your muscles are twitching, ask yourself if one or two days ago, you worked that muscle at the gym.

Shutterstock/Jasminko Ibrakovic
“Above all, fatigue is the reason for the muscle twitching,” explains Kevin Plancher, MD, a leading sports orthopedist and sports medicine expert in the New York metropolitan area.
“The muscles are most likely overworked at this point. The nerves that send impulses to the muscles become fatigued as well, which can cause erratic firing of the muscles.”
He adds: “Cramping and twitching can result from increased amounts of sweating that follow exercise.”
The fact that you can see the twitching is NO cause for concern. Of COURSE you can see it; why wouldn’t you be able to see it?
And it could be a good thing.
You can train your mind to accept it, and then perceive it as cool — as in it feels neat when muscles twitch, especially fatigued muscles that are drained from exercise.
When my right hamstring was injured from sport, it would sometimes twitch after being exercised, and it sure felt good !
The twitching was like a little massage machine inside the hamstring, soothing it.
What makes muscles twitch?
Many things. But at the top of the list are two things:
Muscles will twitch even more if your anxiety is related to ALS.
People who suffer from this hypochondria will typically report that one day, a twitching muscle was becoming annoying.
So they googled muscle twitching and several ALS links came up.
The link descriptions clear-out say muscle twitching is a symptom. The person panics and suspects he or she has ALS.

Freepik.com, jcomp
They then visit the ALS site and read that muscle twitching is one of three chief ALS symptoms. The fear intensifies.
Convinced they might have ALS, the person becomes overwhelmed with anxiety, and within minutes, their localized muscle twitching has “spread” throughout their entire body.
Has this happened to you?
Realize that ALS does not instantly “spread.” Though muscle twitching is an ALS symptom, the ALS websites often fail to add a very crucial detail:
This symptom is preceded by, and then accompanied by, “clinical” muscle weakness.
A fearful person who hits a website that actually includes this detail, however, won’t necessarily be relieved, because once they read this, they’ll then suddenly feel “weakness” in a twitching part of their body.
They’ll stand up and test it out, and sure enough, suddenly the area feels weak. This experience is called perceived weakness.
This is how the mind works.
But ALS weakness is serious; it’s not just a feeling of weakness or a perceived weakness.
You can perceive weakness in your leg all you want, but you’ll still be able to trot up a flight of stairs or run across a parking lot.
If you have ALS weakness, those stairs will be impossible to climb without struggling.
Exercise ranks high on causes of muscle twitching because lactic acid collects in the exercised area, and lactic acid and other byproducts of exercise can cause nerves to spontaneously fire away.
In layman’s terms, the nerves are still buzzed from the exercise, and this buzzing can manifest itself one or two days after the exercise.
Anxiety causes twitching because fear signals to muscles to get ready for a battle.
The muscles rev up their engines and this causes twitching.
The muscles prepare for flight or a fight.
This natural neurological response helped humans survive during primitive times; ancient man’s muscles needed to react quickly to an urgent situation (hissing snake, approaching animal, unexpected chance to catch a rabbit for food, etc.).
Other causes of muscle twitching include electrolyte imbalance, calcium and magnesium deficiency, medications, Lyme disease and dehydration.
ALS ranks at the bottom of the list.
 Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.