Older Women’s Panic Attack Can Predict Heart Attack
An older woman who suffers from panic attacks has an increased risk of one day having a heart attack.
And what makes this situation even more frightening is that the symptoms of a panic attack are eerily similar to those of a heart attack.
They are also similar to the symptoms of a pending heart attack.
Panic attack has a predictive value when it comes to a future heart attack for older women.
If an older woman has a panic attack, this could be a harbinger of a future heart attack as well as stroke.
That one panic attack can raise heart attack risk in older women, says a study, over the subsequent five years.
Scary Results of a Study Linking Panic Attack to Heart Attack
The over 3,300 women in the study were followed for five years, and were ages 51 to 83.
Other heart attack risk factors were adjusted for, showing that the panic attack is an independent risk factor for a cardiac and stroke event.
And just how much was the risk raised? At least one panic episode was linked to a four-fold risk of heart attack.
- What’s behind this association?
- What is the mechanism involved?
But Why Is Panic Attack Linked to Heart Attack?
The researchers speculate that the anxiety that’s involve in a panic situation (whether there’s a true stressor or imagined) may contribute to spasm of a coronary artery.
Another factor is that chronic anxiety will thicken the blood, making it more prone to clotting.
“Diagnosing a heart attack in women can be difficult,” says Amber Robins, MD, a board certified family medicine physician in NY.
“Symptoms in men usually include chest pain, arm pain, and shortness of breath,” continues Dr. Robins.
“For women, the symptoms are less specific and could even be as vague as just a ‘weird’ feeling or pressure on their chest or even a panic attack.
“In general, it is always recommended to do things to help prevent heart disease altogether.
“To do this it would include eating a healthy diet (the closer to plant based and whole grain diet the better) along with physical activity.
“Doing these things also can help improve a person’s mood and may even help decrease anxiety.
“The World Health Organization suggests that older adults get at least 150 minutes of moderate exercise weekly or 75 minutes of vigorous exercise per week. This will help improve overall heart health.”
The results of this study are in the October 2007 Archives of General Psychiatry.
 Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
Dr. Robins has been active in various research studies that include gynecologic cancers, adolescent mothers and minorities in medicine.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik/benzoix
Source: sciencedaily.com/releases/2007/10/071001172830.htm
Why Bench Pressing Sometimes Hurts Your Shoulder

Have you noticed that when you bench press that your shoulder mysteriously begins hurting?
Perhaps the bench press is the ONLY exercise that aggravates your shoulder?
Shoulder pain or hurt when bench pressing isn’t that uncommon. I’m a former certified personal trainer and realize that flat bench pressing puts a lot of stress on the deltoids joint, even though bench pressing is chiefly a chest exercise.
However, bench pressing is actually a compound exercise, targeting multiple muscle groups simultaneously, including shoulder muscles, and also including more than one type of joint, all at the same time.
Recognizing that flat bench pressing can cause shoulder pain or make them hurt (not necessarily both at once; sometimes bench pressing causes only one shoulder to hurt), I rarely had my personal-training clients perform barbell chest presses or dumbbell presses on flat equipment. The flat equipment puts more strain on this joint region.
The pain or hurt in your shoulder that you feel, while bench pressing (and I bet it hurts more when using flat equipment as opposed to inclined), is very most likely due to a strain to the rotator cuff region.
The “rotator cuff” is actually four muscles, and they connect to the shoulder joint via tendons.
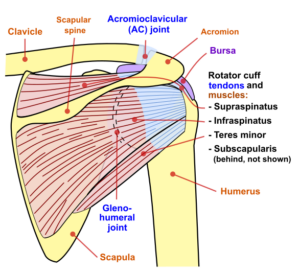
Jmarchin, CC
What typically happens is that either a tendon gets overloaded with more force than it can handle, even though nearby chest or shoulder muscles can handle the poundage; or, one of the tendons becomes frayed by making contact with the humerus bone of the upper arm.
There are other mechanisms of injury in this region, but the two mentioned here stand out in my mind, when it comes to pain or hurt in the shoulder while bench pressing.
It is said that Arnold Schwarzenegger never did pressing using flat equipment for the very reason that it’s potentially injurious to the shoulder joint.
So why does the rotator cuff act up and cause shoulder pain in the first place from bench pressing?
Several factors can be at play, one of which is inadequate warm-up of this sensitive joint.
Many eager beavers jump right into heavy chest workouts without adequate warm-up.
However, warming up prior to this exercise will not really heal an already-injured rotator cuff.
My best advice, to eliminate and prevent recurrence of shoulder pain while bench pressing, is to avoid the flat equipment at all costs.
Use an incline instead. For dumbbell chest workouts, use an incline as well, or use a stability ball.
You can reduce the chances of your shoulder hurting from bench presses by stretching your working muscles between sets; and at the conclusion of the workout, stretch the muscles again for a full five minutes.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/cristovao
Toe Cramp Causes and Solutions
Though the pain of a toe cramp can be enough to make a grown man cry, don’t let toe cramp pain fool you into thinking that toe cramps are caused by any terrible disease.
Searing pain doesn’t always translate to fatal illness. Toe cramps (big and smaller toes) are quite common and often occur in the middle of the night or during exercise.
Causes of toe cramps are many.
Have you ever wondered why toes cramp a lot more than do fingers? What happens to toes, that doesn’t happen to fingers? They’re confined to shoes!
A most common cause of a toe cramp is tight shoes, especially high heels, where the tips of the feet are crammed.
Even though a toe cramp may occur at 3:00 am while you’re shifting in bed, this can still be caused by the shoes you had worn for hours the preceding day. Most common causes of a toe cramp:
Shoes and Boots
This means tight dressy shoes/boots, especially high heels.
Women’s shoes often converge to a point, squeezing out the toes.

Exercise
Runners, particularly distance, as well as long-duration walkers, may find that their activity causes cramping in the toes.
Think about the beating they take while running or long-distance walking.
This includes the hard surface of a treadmill.
It’s no surprise that the cramping toe in the middle of the night is caused by that pounding hike you did the day before.

Dancing, as well, can cause a cramped-up toe, particularly ballet. Don’t rule out yoga as a cause of cramping toes.
“In yoga, one may be holding a position for a considerable period of time, leading to muscle or tendon fatigue which then causes pain or soreness or cramping,” says Bruce Pinker, DPM, who specializes in sports medicine and surgery of the foot and ankle.
“Most muscles and tendons have an elastic quality which allows for extension and contraction, and if overused, will lead to cramping,” continues Dr. Pinker.
“Sudden toe cramps can be due to tendon overuse. It happens to many individuals, especially ‘weekend warriors.’ Lactic acid can build up, leading to discomfort.”
Calcium Deficiency
“It can also be due to a calcium deficiency as well as other nutritional deficits,” says Dr. Pinker.

Shutterstock/marina kuchenbecker
Not enough calcium has been known to cause toe cramps.
If you’re limiting calcium-rich dairy foods due to calories or other reasons, your toes may be paying for it in the form of spasms and cramps.
Magnesium Deficiency
“Magnesium assists over 300 enzyme actions in the body including the production and transport of energy, temperature regulation and the synthesis of protein, while it also relaxes muscles, preventing cramping–especially important to athletes and anyone suffering from toe cramps,” says Carolyn Dean, MD, ND – Medical Advisory Board Member of the non-profit Nutritional Magnesium Association at nutritionalmagnesium.org.
Drugs
Ask your doctor if your prescription drugs might cause toe cramping, especially if you’re taking cholesterol, blood pressure and asthma drugs.
Solutions to Toe Cramps
Limit high heels. Wear them for short periods, but not for work all day. Make sure lower heeled shoes have a roomy toe fit.
Next, include your toes in your exercise regimen.
Most people do not consider the importance of this last point. The muscles at the tips of your feet should be exercised.
The exercise that these muscles get from everyday walking and from your cardio routines is not enough, and here’s why:
Toe muscles need structured, gentle exercises that isolate them, and this includes stretching.
Walking and cardio routines do not isolate these tiny muscles in a gentle way, nor stretch them in a way that your hands can stretch them.
Several times a day for 30 seconds, gently pull toes towards you to stretch the underside muscles. Then curl your toes and hold that position for a few seconds.

Freepik.com, yanalya
In bare feet, spend a few minutes picking up socks off the floor by just curling your toes and forming a pincer-like grip.
Finally, flex and extend toes for a minute here and there throughout the day.
These exercises will condition the tiny muscles in a way that will help guard them against cramping up.
Prior to a yoga session, gently extend and flex the toes, and do some sock retrieving.
Magnesium supplement: “One of the most absorbable forms of magnesium is a powdered magnesium citrate that is taken with hot or cold water,” says Dr. Dean.
Make sure you’re getting enough potassium as well. A calcium and vitamin C supplement will also help. Keep well-hydrated, especially if you exercise.
If you experience a cramp, let it run its course. It should be over in a few minutes.
Remember, pain doesn’t necessarily mean a terrible disease. In the case of toe cramps, this is a benign (harmless) condition, though a royal nuisance.
However, if you decide to seek medical attention, see a podiatrist, an MD who specializes in foot care.
 Dr. Pinker is with Progressive Foot Care, which provides state-of-the-art, full diagnostic testing and treatment of the foot. He’s a professional foot and ankle health and wellness speaker who delivers many original seminars annually such as “Keep On Running.”
Dr. Pinker is with Progressive Foot Care, which provides state-of-the-art, full diagnostic testing and treatment of the foot. He’s a professional foot and ankle health and wellness speaker who delivers many original seminars annually such as “Keep On Running.”

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
What Can Make Your Hip Hurt After Running?
Hip pain after running can have one of multiple possible causes.
And one of them is arthritis – -something that every runner dreads hearing.
What are those several causes of hip pain after going on a run?
But first, my advice to anybody suffering pain in the hips during or after going for a jog or run, is to ask yourself if one side of your body — the side with the pain — was stressed more than the other side.
Years ago I actually had a problem with hip pain after running. In my case, the discomfort resulted from doing wind sprints while holding onto the leash of my German shepherd.
He loves to run full speed, but I wouldn’t let him, and thus, the resulting muscle strain.
He’d be ahead of me, restrained from full speed by my grip on the leash.
But his pulling caused my hip, on that side, to absorb a lot of tension and stress, and hence, the subsequent aching muscle in my hip area that persisted for about 10 days.
Jogging while keeping a steering hand on a “Baby Jogger” can produce a similar result.
Another culprit can be holding onto a treadmill with one hand while jogging; this will throw things off-kilter. Release that hand and swing both arms naturally.
Most Common Benign Causes of Pain in the Hip after Running
“The most common benign causes include trochanteric bursitis; iliotibial band friction syndrome (ITB); and piriformis or gluteal muscle strain,” says Dr. Joseph J. Ruane, a sports medicine specialist with OhioHealth Physician Group.
“More serious causes include stress fracture, pinched nerve in the spine referring to the hip area, and a labral tear or arthritis of the hip joint.”
Trochanteric bursitis: This is hip bursitis, and inflammation of the bursae (plural of bursa, a fluid-filled sac that subdues friction between two uneven surfaces) will cause discomfort.
ITB: The iliotibial band is a thick fibrous band of tissue that runs the length of the outer part of the upper leg to just below the knee.
It begins at the hip, and hence, why inflammation of this structure will cause pain there.
Piriformis muscle strain: Also called piriformis syndrome, this involves the piriformis muscle, located behind the hip.
The piriformis’s tendon may encroach upon the sciatic nerve, causing the pain.
Stress fracture: This is a hairline fracture that, if present in the hip, will cause pain, and running can result in a stress fracture, due to its impacting nature.
Pinched nerve: A nerve that feeds hip movement can become pinched at the spinal column.
Labral tear: Labral tissue is cartilage, and when torn, will cause hip pain. Surgery is the option only when physical therapy has failed.
Arthritis: Osteoarthritis, when it occurs in the hip, means trouble. It’s a degenerative condition and over time, cartilage that normally resides between bones to prevent bone-on-bone friction, withers away, until you have bone-on-bone joint action.
But it need not progress this far to result in a lot of pain during or after running.
Other causes of hip pain after running: weak back muscles, leg length disparity and over-pronation (when the foot rolls inward with each strike on the ground).
Overuse (too much running at once) can simply strain the muscles that act at the hip joint.
If you’re new to running or jogging, proceed gradually. Listen to your body.
If hip pain develops during or after running, don’t try to work through it. Your body is trying to tell you something.
 Dr. Ruane’s practice is dedicated to comprehensive, nonsurgical musculoskeletal care. He is active in clinical research and is a nationally recognized speaker and educator.
Dr. Ruane’s practice is dedicated to comprehensive, nonsurgical musculoskeletal care. He is active in clinical research and is a nationally recognized speaker and educator.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Why There’s Pain Under Your Kneecap During or After Running

So you had a good run, but the second you stop, here comes that gnawing pain beneath your kneecap.
Or maybe it came on during your run.
What IS this and what can be done about it?
Or maybe you awaken the day after running to feel unbearable pain in the knee upon standing?
Or perhaps after sitting a while and then standing, your knee pain is hollering at you?
Causes of Running Related Pain Under Your Kneecap
I asked Dr. Kevin D. Plancher, MD, MS, FACS, FAAOS, a leading NY orthopaedic surgeon and sports medicine expert, questions about what causes knee pain in runners, and solutions to the aggravating knee pain and aching behind the kneecap, that runners often experience.
This kind of knee discomfort is called patellofemoral pain, and is also known as patellofemoral pain syndrome.
It’s also commonly referred to as chondromalacia, but you’ll soon see why these two terms are not interchangeable.
How can a person self-diagnose chondromalacia/patellar-femoral syndrome? (Some people have a large medical insurance deductible!)
Dr. Plancher explains, “Patellofemoral pain syndrome and chondromalacia patella are two separate entities, and should not be confused with one another.
“Patellofemoral pain syndrome is pain from behind the patella, and chondromalacia patella is fraying and/or damage to the articular cartilage of the patella. Chondromalacia is a surgical finding and not a diagnosis.
“Patellofemoral pain is commonly found in adolescents, especially young females, and has been estimated to account for up to 30% of all injuries seen in sports medicine clinics.
“Patellofemoral pain syndrome is a multifactorial condition, and mechanisms which cause this condition can be overuse or overloading, abnormal patellar tracking, or direct trauma.
“Other factors which may predispose an individual include muscle dysfunction, pes planus foot type, malalignment, muscle and soft-tissue tightness, congenital abnormalities of the patella or patellar groove, etc.”
Symptoms
Dr. Plancher explains, “Symptoms individuals commonly report are pain during and/or after activity, pain after prolonged sitting, crepitus (grinding), stiffness, and a sensation of giving way while ascending/descending or walking on an incline.
“The pain is usually described as a dull or achy sensation and arises from behind the kneecap.”
(This particular knee discomfort syndrome has also been described as a “fullness” sensation in the knee, or a tightness.)
Will a person with this knee problem necessarily have every single symptom?
“Individuals with patellofemoral pain syndrome may experience one or all of the previously listed symptoms,” says Dr. Plancher.
Can a person have knee pain just from running but be free of knee discomfort when climbing stairs or using the gym’s revolving staircase?
Dr. Plancher says, “Patellofemoral pain syndrome is the most common injury in runners, and running on a crowned road (repetitively in the same direction) increases the risk due to the altered biomechanics placed on the foot and ankle.
“Descending stairs typically causes more pain than ascending. This is because when descending, the contact area between the patella and femoral articulation is small, placing a great deal of stress over that small area.
“When ascending, the contact area is larger, therefore distributing the forces over a greater area.
“Patellofemoral joint reaction forces have been calculated at 3-4 times the individual’s body weight while ascending or descending.
“Patellofemoral pain syndrome is also different from jumper’s knee. Jumper’s knee is a layman’s term for patellar tendonitis.
“Patellar tendonitis is an overuse injury to the patellar tendon, which is frequently seen in jumping athletes such as basketball and volleyball players.
“The location of the pain in patellar tendonitis is typically located along the patellar tendon and not from beneath the patella.
“However, patellofemoral pain syndrome can occur in individuals who perform a great deal of jumping.”
Why is it that a person with patellar-femoral syndrome can feel minimal knee pain while running, and barely any knee pain the rest of the day after the running, but then next morning awaken with searing knee pain?
“Increased amounts of endorphins are released during moderate to strenuous continuous exercise, which may mask the symptoms during such activities,” says Dr. Plancher.
“This phenomenon can cause more harm than good, as an individual may exceed their physical limit.
“Once the effects of the endorphins wear off, the individual may start to experience pain that they did not during their run.”
Why is it that someone with chondromalacia/patellar-femoral syndrome suffers notably more knee pain after sitting for long periods, but then the knee pain dissipates somewhat after walking around?
“Individuals with patellofemoral pain have an increase in symptoms during prolonged sitting due to the increased pressure from the articulating surfaces over a period of time,” explains Dr. Plancher.
“This often dissipates somewhat after walking a short period, due to the varying forces across the knee during gait.”
The motion of squatting is strongly advised against in someone with chondromalacia/patellar-femoral syndrome, yet the very act of squatting with the thighs parallel to the floor may alleviate the knee pain in some individuals.

Freepik/master1305
In fact, for some this alleviates the discomfort after an entire leg workout session at the gym consisting of squats and leg presses. Why?
“Squatting is strongly advised against in individuals with patellofemoral pain syndrome due to the increased stress being placed through the articulation of the patella and patellar groove with active knee flexion,” says Dr. Plancher.
“However, as flexion increases, the surface area of the patella articulating with the patellar groove increases, thus decreasing the overall force placed on the joint, which may be the cause for the decrease in symptoms.”
What would cause the patella to “float” or be wobbly or loose upon lightly pressing on it, while the leg is outstretched on the floor?
“Although joint effusion is not commonly associated with isolated patellofemoral pain syndrome, an effusion may occur.
“The increased fluid in the joint may cause the patella to appear to ‘float’ compared to the uninvolved side.
“If a large effusion is present you should seek out care from a qualified sports medicine professional to evaluate if there are other pathologies present.”
At what point can a patient know he’s good to go for all-out exercise, if after the knee is feeling great for a week, he has a relapse? Is this a timeline thing?
“It’s not recommended that an individual return to their normal exercise routine immediately after their pain has resolved,” notes Dr. Plancher.
“It is recommended that the individual gradually progress their training back up to their normal exercise regimen, typically increasing their time and/or distance by 10% each week.”
This may help decrease the chance of recurrence as well as become more confident with her knee.
Gradual increases in training will also help build endurance and may help decrease other musculoskeletal injuries.
 Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
 Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Lopolo
Forearm Pain Doing Biceps Curls: Cause and Solution

I solved my forearm pain that occurred during biceps curls.
If you’ve been suffering forearm pain from biceps curls, you might be experiencing exactly what I experienced.
I’m a former certified personal trainer, but even personal trainers can get muscle tweaks every now and then.
I had to stop doing biceps curls because of the discomfort in my right forearm.
But the forearm pain was not caused by the biceps curls.
It was caused by neutral grip pull-ups, using the “V” bar slung atop a standard pull-up bar.

When you do pull-ups with the “V” attachment, it creates a unique stress on the lower arms.
The problem didn’t all come at once, however. After a pull-up session one day, I noticed a little discomfort in my right forearm that I connected to the pull-ups, but didn’t think too much of it.
The following week, I repeated the pull-up routine, and afterwards, felt more of the “pain” in my forearm.
In fact, while doing the pull-ups, I felt it, but didn’t think it was a big deal.
I also had been feeling the forearm “pain” while doing biceps curls.
The discomfort was located at the brachioradialis muscle, right up to the part where the arm bends.

Anatomist90, CreativeCommons
The next week, again I did the pull-ups, and afterwards, realized that whatever was going on in my brachioradialis wasn’t going away too soon.
My chest-biceps workout came three days after my pull-up workout, and I noticed that my forearm really bugged me when doing biceps curls.
The next week, I was able to do pull-ups, while still detecting the annoying tweak. But from that point, biceps curls were a problem.
For some reason, I never had to give up pull-ups; the discomfort was marginal and doable.
But during biceps curls, my forearm felt injured, and I had to finally admit it:
I had to stop doing biceps curls in order for my forearm to heal.
My elbow joint was not affected. This was a self-diagnosed muscle problem with no tendon involvement.
If a tendon were indeed involved, it should have made pull-ups painful.
On the other hand, this was the slowest-healing muscle-only injury I’ve ever had.
It kept me from doing heavy biceps curls, and in my case, I either do them heavy, or I don’t do them at all.
I hate working biceps, and doing them heavy (4-10 rep max) gets the job over more quickly.
I also couldn’t do heavy hammer curls without forearm pain.
And this forearm pain carried over to dumbbell shoulder presses, in that upon bringing the weights down to my lap after completing a set, caused pain in my brachioradialis (a forearm muscle).
To bring the weights down requires the same muscle action as the negative of a reverse biceps curl or hammer curl.
And thus, bringing the dumbbells down incited forearm pain; I use only heavy dumbbells for military press, and thus, had to replace this exercise with machine military press.
Solution to Forearm Pain During Biceps Curls
Do hammer curls with 5-pound weights, 20 reps, three sets, one minute in between sets.
It’s best that you do these standing or seated, rather than with a preacher curl machine.
If this causes annoying discomfort, stop at fewer reps, maybe 12 or even 8. If the forearm pain is really nasty, use even lighter weights.
The goal is to reintroduce the injured muscle to the concept of weightlifting, but in a baby-steps way.
Do this every time you’re at the gym if you can remember. I’d remember to do it 2-3 times per week.
The 5-pound weights actually bought out a subtle pain in my forearm, but it was very doable.
Ironically, throughout all this, I was able to keep doing the pull-ups. Strange, I know.
When 20 reps of the 5-pound weights no longer brought out forearm discomfort, I moved up to 8-pound dumbbells, and repeated the protocol: three sets of 20 reps of hammer curls.
I felt mild tweaking in the forearm, but it was very tolerable. When it disappeared, I switched to 10-pound dumbbells. You get the picture.
It took a few months before 20 reps of 15-pound dumbbell hammer curls no longer brought out the forearm pain.
At this point, I considered myself completely rid of whatever happened to my brachioradialis, and deemed myself ready to return to heavy biceps curls and dumbbell military presses.
Oddly, despite a two-month absence from biceps curls, I hadn’t lost much strength; I was at about 95 percent.
There was also no forearm pain upon bringing dumbbells down to my lap after finishing a shoulder press set, though there was some loss of strength.
Forearm pain while doing dumbbell curls?
Avoid that which really brings out the forearm pain, and commit yourself to a “baby-steps” type of rehabilitation. BE PATIENT.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer who helped her clients achieve fat loss, muscle growth, strength and improved fitness.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer who helped her clients achieve fat loss, muscle growth, strength and improved fitness.
.
Top image: Shutterstock/staras
Ankle Pain After Running: Causes and Solutions
Do you suffer from ankle pain after running but can’t figure out what could be causing this?
There can be a number of causes — and each cause has a unique solution.
Ligament Strain or Sprain
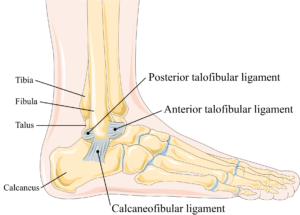
Ankle ligaments. Laboratoires Servier, CC BY-SA 3.0 creativecommons.org
Most runners have “rolled” an ankle at some point, and this can result in the overstretching or the micro-tearing of a ligament.
“The most common cause of ankle pain after running is an ankle sprain,” says Dr. Dave Candy, a board certified specialist in orthopedic physical therapy.
“This would happen after ‘twisting’ your ankle from stepping off a curb wrong or stepping on some other uneven terrain.
“This stretches or tears ligaments, usually on the outside of the ankle.”
Tarsal Tunnel Syndrome

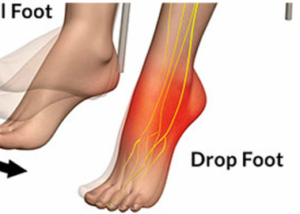
Tarsal tunnel. Nicole Williams, Jake Willet, Damian Clark, David Ketteridge/creativecommons.org
Another cause of ankle discomfort following a running session would be tarsal tunnel syndrome.
“Tarsal tunnel syndrome is an irritation or compression of the tibial nerve at the ‘tarsal tunnel’ — which is behind the bump on the inside of the ankle (medial malleolus),” says Dr. Candy.
“Most commonly, symptoms of tarsal tunnel syndrome are pain, numbness or tingling in the feet.
“This can sometimes be mistaken as plantar fasciitis. However, it is possible to have pain locally on the inside of the ankle as well.”
Osteochondral Defect or Arthritis
“Occasionally, if you run a lot of excessive mileage over a long period of time, you can develop an injury to the cartilage in the ankle joint,” says Dr. Candy.
“An osteochondral defect is an acute injury to the cartilage in the ankle joint, whereas arthritis is a gradual wearing down of the cartilage over time.”
Lack of Structured Motion
Another cause of ankle pain after some running may be simply due to lack of structured motion in the foot.
You may think you’re getting plenty of this when jogging all over the place, but jogging or running takes place in a linear path.
Unresolved Past Injury
When running causes ankle pain, this may also signal a past, unresolved injury to the foot, such as an ankle sprain that you only thought had resolved.
Sure, everything feels fine when you’re on the job, for instance, but once the feet get pounding on the pavement or treadmill, pain sets in from a not fully healed sprained ankle or strained tendon from the past.
Solutions to Ankle Pain After Your Run
Dr. Candy explains, “Adjusting mileage and frequency of running are always the first-line treatments for any of these problems. You should not run through pain.
“Ankle braces can help in the short-term for ankle sprains.
“Orthotics and/or shoes with good arch support can be helpful for tarsal tunnel syndrome and/or arthritis.”
You’ll want to try Birkenstock arch supports — these are durable, very long-lasting, comfortable and effective.

Birkenstock arch supports
“Additionally, stretching your calves and improving ankle stability through doing heel raises and balance exercises can be helpful for any of the above ankle problems.
“Outside of that, consider seeing a physical therapist to get recommendations that are more specific to your particular problem so that you can get back to running pain-free as quickly as possible.”
A great ankle ligament strengthening exercise is to walk backwards on the balls of your feet: with feet facing foward, facing outward and then facing inward.
Don’t delay if the discomfort in your ankle doesn’t seem to be diminishing once you’ve begun taking corrective measures such as new footwear, arch supports, jogging on softer terrain, stretching, cross-training, etc.
 Dr. Dave Candy, PT, DPT, is a specialist in orthopedic physical therapy and owner of More 4 Life. He’s the author of Chronic Pain: You’re Not Just Getting Older, You’re Not Crazy, And It’s Not All In Your Head, available on Amazon.
Dr. Dave Candy, PT, DPT, is a specialist in orthopedic physical therapy and owner of More 4 Life. He’s the author of Chronic Pain: You’re Not Just Getting Older, You’re Not Crazy, And It’s Not All In Your Head, available on Amazon.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Aching Bad Calf Cramps: Causes, Treatment, Prevention

The most agonizing pain in the calf comes at some point during your sleep, but calf cramps can also strike you during athletic training.
They can instantly halt whatever it was you were doing.
Calf cramps can be exceedingly painful, and everyone has experienced this pain at least once in their life.
What really goes on when a calf cramp comes on, which can take only a few seconds from painless to horribly painful?
There are actually several causes of calf cramps.
Dehydration is one of them. This doesn’t mean gasping for water as though you’ve been wandering in a 100-degree desert for days. You can be dehydrated and not even feel thirsty.
To prevent this, make a point of drinking six to eight glasses of water every day, whether or not you are thirsty for it.

Shutterstock/The Faces
You don’t have to drink a whole glass at once. You can sip throughout your waking moments. Lack of hydration can speed up the calf (and stomach) cramping process.
Not getting enough rest, and/or overexercising, is the next cause.
Calf cramping can occur if you’re pedaling hard on a bicycle for a prolonged period, exceeding the time that you normally spend pedaling.
Or an extra-long hiking bout up steep grades can cramp the calves up.
The cramping can come on suddenly, and if you’re a few miles from the trail head, you have no choice but to continue hiking for that distance, making the cramping worse.
Vitamin deficiency is the third possible culprit. It’s believed that the depleted levels involve phosphorus, magnesium, calcium, sodium and potassium.
Insufficient warming up also can lead to calf pain. Stiff calves are more vulnerable to cramping up.
Another cause of calves cramping up is magnesium deficiency.
“When your muscles are engaged in the rapid-fire contraction and relaxation of physical exercise, if there is too much calcium (the initiator of contractions) and too little magnesium (the initiator of relaxation), muscle cramps and a buildup of lactic acid can result,” explains Carolyn Dean, MD, ND – Medical Advisory Board Member, Nutritional Magnesium Association at nutritionalmagnesium.org.
“Eighty percent of the population has magnesium deficiency, which means that as you stretch your legs, which requires calcium to initiate that contraction in the muscle, if you don’t have magnesium to relax that muscle, the contraction continues into a cramp/charley horse or muscle spasm or twitch.”
Lastly, poor circulation, as a result of tight socks, can cramp calves.
Solutions to the Pain of Calf Cramps
An obvious solution is to cease the activity, or take a rest if you’re out in the wilderness, and massage the affected area.
Taking a magnesium supplement will also help, and Dr. Dean says it should be in powder form because this is the most absorbable.
Also do some stretching, and drink water. But to prevent calf cramps, it’s important to warm up before exercising.
I always see people jumping on the treadmill and going straight into a six or seven mph run; no slower jog preceding it, not even a walk.
It’s also not smart to exit fast running and enter straight into a seated position.
Transition out of fast running to slow running, and then a few minutes of walking, if you are vulnerable to calf cramping.
Slip in calf stretching throughout your workout, even if it’s an upper body day.
While you’re waiting for someone to finish up on the seated chest press equipment, for instance, do some calf stretching.
Drink water before, during and after exercise, whether or not you are thirsty.

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ANN PATCHANAN
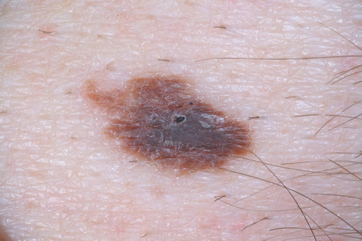
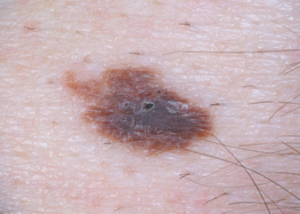
What Does Precancerous or Atypical Mole Mean?
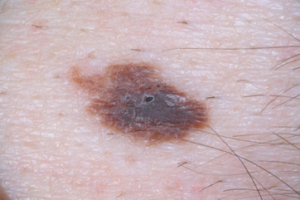
Atypical Mole
Have you been told you have a precancerous or atypical mole?
Or maybe you were not satisfied with your doctor’s response to “What is a precancerous mole? What does atypical mean?”
Maria M. Tsoukas, MD, PhD, Assistant Professor, Dermatology Section, University of Chicago, will explain in detail just what a precancerous (atypical) mole means.
First of all, if you’re concerned about a precancerous or “atypical” mole, make sure that you consult with a dermatologist as opposed to your primary care physician.
Dr. Tsoukas explains, “Moles are common skin growths. They are correctly called melanocytic naevi (American spelling ‘nevi’), as they are due to a proliferation of the pigment cells, melanocytes.
“If they are brown or black in color, they may also be called pigmented nevi. Moles are benign in nature (harmless), but malignant melanoma (cancerous) may arise within a mole.”
About 30 percent of melanomas arise in a pre-existing lesion.
Dr. Tsoukas continues, “Some of the nevi appear since birth. There can be nevi that normally appear till around the 35th year of age.
“In pigmented and non-pigmented melanocytic nevi, we may identify clinically and histologically [with a microscope] certain atypical features.”
Atypia means the cells show some unusual features.
“In clinical examination by an expert, even when atypia is detected, malignancy cannot be excluded,” says Dr. Tsoukas.
“In those cases we obtain a specimen for histologic examination under the microscope or biopsy.”
Even if you’re planning on having a normal looking spot removed for cosmetic reasons, request a biopsy just in case.
Dr. Tsoukas says that in clinical examination, dysplastic (atypical) nevi are often bigger than other moles, and tend to be abnormally shaped and colored.
They can be anywhere including non-sun exposed skin.

Atypical moles (dysplastic nevi). Shutterstock/Mikel Ugarte Gil

Atypical mole. Source: cancer.gov
When nevi are present with a lot of clinically defined atypical features, a biopsy is indicated to evaluate for melanoma — which kills one American every hour.
“In microscopic evaluation there are certain features that are met so as a tumor is defined as malignant,” explains Dr. Tsoukas.
“Dysplastic (atypical) nevi may present with some of those abnormal features under a microscopic evaluation.
“However, they do not meet all criteria to be diagnosed as melanomas under the microscope.”
Think of a continuum: At one end is benign, and at the other end is melanoma.
An atypical (dysplastic) mole sits somewhere between both ends of the continuum.
“This means that atypical nevi have some features that we see in melanoma, in clinical exam and under the microscope, but not all of them.”
So, in theory, any nevus that looks pathologically atypical can evolve into melanoma.
However, if the microscope shows mild atypia, this isn’t nearly as concerning as severe atypia. Moderate atypia falls somewhere in between.
Now, what percentage of melanomas actually arise from an atypical mole?
Dr. Tsoukas says those who have dysplastic nevi without family history of melanoma face a 7 to 27 times higher risk for developing melanoma.
However, this doesn’t mean that an atypical mole will necessarily transform into melanoma, although a severely atypical mole — as just mentioned — has the highest chance for melanoma transformation.
“We carefully examine and thereafter remove atypical moles (entire lesion) via biopsy or surgical excision techniques in the office.”
Having many dysplastic nevi is one of the risk factors for melanoma.
“Someone with many dysplastic nevi and personal history or with 1st-degree relatives who have had melanoma has an extremely higher lifetime risk of developing melanoma, than general population” says Dr. Tsoukas.

Melanoma under magnification. Shutterstock/Nasekomoe
Additional risk factors include: fair skin, sunburn history, indoor tanning, advancing age (though teens and children can get melanoma) and immunosuppression.
Remember the mnemonics for mole assessment: ABCDE
A – Asymmetry; one half of the mole does not match the other.
B – Border; ragged, notched or blurred.
C – Color; non-uniform and changing; mottled appearance; may include areas of red, white and blue; beware of new blackness in a mole.
D – Diameter; though melanoma is usually bigger than 6 mm (larger than pencil eraser) upon diagnosis, they can be smaller.
E – Evolving; beware of a changing mole and don’t hesitate to seek medical advice.
Dr. Tsoukas’ clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.
clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources: American Cancer Society National Cancer Institute
Are Purple Moles Normal or Possible Cancer?

Do you have a purple mole? If so, are you worried that your mole has cancer because it’s purple?
“The color of a mole may vary within normal ranges, and purple color may not necessarily mean harmful or harmless mole,” says Maria M. Tsoukas, MD, PhD, Assistant Professor, Dermatology Section, University of Chicago.
Thus, a normal mole may indeed appear to be purple. So if the question is, “Does a purple mole mean cancer?” then the bigger question should be:
Has your mole always been purple?
If it’s been this color for years, then you can assume that this is the normal nature of the skin spot.
On the other hand, if the mole has recently taken on a purple color — get it examined by a dermatologist.

Shutterstock/Albina Glisic
When a mole changes color, this can signal melanoma skin cancer, the deadliest skin cancer, with a very low five-year survival rate once this skin cancer has spread to other sites in the body.
Dr. Tsoukas explains, “The colors that we see are based on optics in human skin with regards to structures existing under our skin.
“As a general rule, red hue is due to vascular network lying in the top layers of our skin. Pigmented cells located deep in our skin may cause a bluish appearance.
“In examination of moles we are also using, along with clinical observation, dermoscopy where we have now established certain patterns of moles.
“However, confirmation is obtained by biopsy of mole and examination under microscope.”
Normal moles can come in the following colors: tan to dark brown and any shade in between; flesh colored; pink; blue; and black.
The color of a mole should be uniform.
If there is change in color, that’s when to be concerned and make an appointment with a dermatologist.
Melanoma can present in the following colors: flesh toned, white, red, blue, pink, purple, tan to dark brown, black and grey.
“Therefore, color of mole cannot confirm with regards to benign or malignant growth.”
A melanoma can be comprised of several of these colors. The key again is if the pigmented spot has been changing in color.
If you’re not sure if that purple spot on your skin has always been there, or whether or not the skin lesion has always been purple as opposed to another color, then play on the safe side and have a dermatologist look at it.
Also, what you think is a purple mole might actually be another type of skin lesion, such as a seborrheic keratosis, a benign skin lesion or barnacle that’s completely harmless.
“That’s why you need to seek medical advice to confirm,” says Dr. Tsoukas.