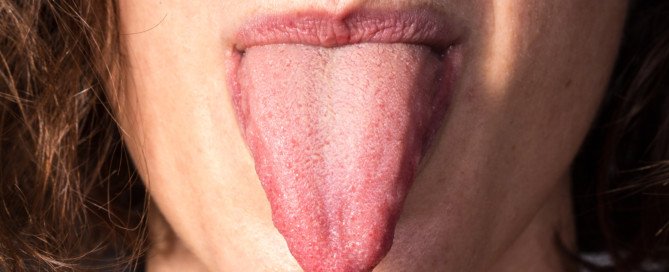
Yellow Tongue Causes: Is One Cancer?

An ear, nose and throat doctor addresses the various causes of a yellow tongue.
If you’ve been noticing lately that your tongue is looking rather yellowish, perhaps you’ve been wondering if this might possibly mean cancer.
And if not, what on earth could possibly be causing this oddball symptom? Could it mean something serious?
There are various possible causes of a yellowish tongue.
But thank goodness, cancer is not a likely cause of this strange symptom.
The following situations are more likely to be the culprits.
COMMON VICES

Shutterstock/Slava Dumchev
“If you drink a lot of coffee and/or smoke cigarettes, the healthy pink membranes of the tongue can be stained yellow,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Other things that can stain the tongue are tea and other tobacco products,” continues Dr. Silvers.
“Quit or reduce smoking and consider less coffee and tea intake. You can gargle or brush your tongue after consumption of staining liquids.”
ACID REFLUX

Shutterstock/Monster e
“Acid reflux can change the pH in the oral cavity and lead to a yellow coating on the tongue; trial of reflux medication may be helpful,” says Dr. Silvers.
Follow the instructions and begin with the lowest recommended dose.
YEAST INFECTIONS
“Recent courses of antibiotics, poor ability to fight infection and steroid inhalers for asthma can lead to yeast infections,” says Dr. Silvers, “which can have a yellow/grey color to the tongue. The tongue should be cultured by your doctor.”
A tongue with a yellow tinge is usually a temporary and harmless issue.
RARELY can this mean a problem with one’s liver or gallbladder.
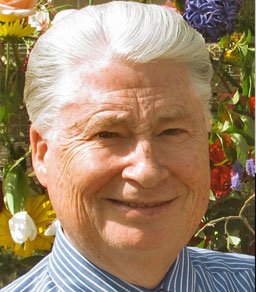
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/donikz
Burning Tongue: 9 Causes, One Life-Threatening

An ear, nose and throat doctor explains the 9 possible causes of a burning tongue, and one of these conditions can kill you.
A burning tongue can have numerous causes, says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Burning tongue can be caused by dehydration, certain medications (which tend to lead to dry mouth), acid reflux, diabetes (dry mouth), infection (yeast), tongue ulcer or menopause,” explains Dr. Silvers.
New Medications
“If the symptoms started within days or weeks of starting a new medication, then speak with your doctor, as this may be the cause,” says Dr. Silvers.
Diabetes
“If you have excessive thirst and tongue irritation, then see your doctor for routine blood testing to check for diabetes.”
Diabetes is a life-threatening condition that also increases the risk of heart attack, heart disease, stroke and dementia.
Yeast Infections
“Recent courses of antibiotics, steroid inhalers for asthma and poor ability to fight infection (seen with HIV or other autoimmune disorders) can lead to yeast infections and cause a burning tongue; see your doctor for a culture.”
Acid Reflux
“Acid reflux is a common cause of burning tongue due to the acidity from the stomach which can irritate the tongue and the oral cavity.
“Consider seeing your physician or trying an over the counter reflux treatment to see if the symptoms resolve.”
Menopause
Dr. Silvers says, “If you are experiencing menopause then see your GYN. Hormone replacement therapy may be helpful.”
Of course, the burning can also be caused by having recently eaten something hot, or taken a hot drink.
Another cause of the burning sensation is a cut, usually caused by a sharp piece of food, such as a bit of potato chip or cracker.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ilaria burlini
Why Does Blowing My Nose Cause a Bad Stink?
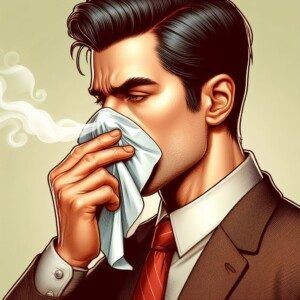
An E.N.T. doctor explains what can cause a bad odor after you blow your nose.
So what on earth can be causing that foul odor coming from your nose after you blow it?
“Bad odor after blowing the nose is usually caused by old mucous in the sinuses or a sinus infection,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology.
“Occasionally acid from the stomach has been seen in the back of the nose,” continues Dr. Silvers.
“This alone can cause a bad odor from the nose, but can also lead to higher incidences of sinus infections.”
“Chronic sinus problems don’t present with fever or congestion, but may simply present with fatigue, pressure over the cheeks and forehead, and a bad odor in the nose after blowing.”
If you ever feel a burning sensation in your nose, this is probably refluxed acid.
Is there a remedy ?
Dr. Silvers explains, “A natural sinus wash like a neti pot [see image below] can be very helpful if the sinuses are the cause.”

Aikhan, CC BY-SA 3.0
Your local drug store carries neti pots (sinus rinse device), and you can also buy sinus rinse solutions that come in a packet. If this doesn’t solve the problem, Dr. Silvers says:
“…then see your doctor or your ENT for a nasal/sinus exam and a culture.
“A child with a bad nasal odor may have a chronic adenoid infection or a foreign body in the nose (especially if there is mucous draining from only one side).”
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Chest Pain’s Many Causes & Which Mean Heart Trouble
Here is a sampling of chest pain articles.
- If doctor says your chest pain is from acid reflux or GERD, how do you know he’s not misdiagnosing an imminent heart attack?
This happened to my mother. The ER doctor sent her home with a prescription to an acid reflux drug. Two days later she was on the operating table for quintuple bypass surgery.
My sister, a doctor, said that this happens all the time: An ER doctor mistakes a pending heart attack for a digestive problem, and then days later, the patient is dead from a heart attack.
This potentially fatal mistake by a doctor, which happens frequently, can be stopped dead in its tracks if you know how to recognize it. Read more…
- Chest pain and shortness of breath? When to visit the ER…
If you have chest pain and labored breathing, even if you’ve been diagnosed with GERD, this can still mean a heart attack is looming or is actually in progress. Read more…
- Chest pain caused by acid reflux (GERD)
Severe coronary artery blockage is often misdiagnosed as gastroesophageal reflux disease.
However, GERD or acid reflux really CAN cause quite a bit of chest discomfort. Go to article.
- Does angina always cause chest pain?
You can have angina and not experience any chest pain, but you’ll certainly experience at least one of several other possible symptoms. Go to article…
- Chest pain with cough: several possible causes
Never ignore the pairing of pain in the chest with a cough, because three of the possible causes can kill you within minutes.
One of the possible causes is a bulge in the aorta, the big vessel that originates in the heart.
If the bulge is big enough, it can burst and cause death within minutes. Find out the other two causes.
- Can chest pain be the only symptom of a heart rhythm disorder?
An abnormal heart rhythm (arrhythmia) can cause faintness, dizziness and shortness of breath, along with chest pain.
What if all you have is chest pain? Any possibility this can be a heart rhythm problem? Read more…
Rushing to the ER for Chest Pain
Chest pain is one of the top reasons people rush to the emergency room.
Because it can signal serious conditions like a heart attack, blood clot or lung problem, doctors take it very seriously.
It should be taken very seriously even when the patient is a young adult athlete.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/haynepplstockphoto
HEART BYPASS SURGERY (CABG): RISKS, COMPLICATIONS, RECOVERY
Top image: Shutterstock/ChaNaWiT
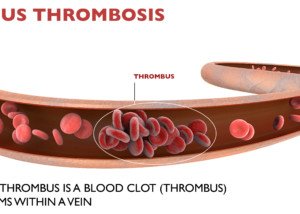
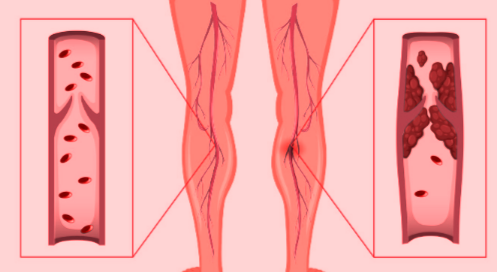
Post-Surgical DVT Treatment without a Blood Thinner?

How is a post-surgical DVT treated if giving the patient a blood thinner can cause dangerous internal bleeding?
If a DVT develops during or after surgery, how is it treated if giving the patient a blood thinner (anticoagulant) can cause life-threatening internal hemorrhaging?
I was alarmed when the doctor ordered no treatment for my mother’s post-surgical DVT in her neck.
There was the risk that it would break loose and go to her lungs and become a pulmonary embolus — a blood clot blocking a vein leading to the lungs, which can kill in minutes.
Instead, the “big DVT” was just left to sit there while she was in ICU following her quintuple bypass surgery.
I asked, “Why can’t you give her coumadin or heparin?” I was told that these blood thinning drugs could very well spark a very serious internal bleeding somewhere, putting her life at immediate risk.
I was also told that the blood thinners would not break up the DVT, only prevent it from proliferating further.
I then asked why not give her tPA (a clot-busting drug)?
I was given the same reason about the internal bleeding. I was also told that the chances were small that the DVT would go to her heart.
Well gee, how could they know that?
“Generally, DVTs are treated with anticoagulation (blood thinners), except when there is a contraindication for this,” explains Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“Along with recent surgery, there is a long list of other reasons why one would not want to systemically anticoagulate a patient (trauma, head injury, brain tumors, frequent falls, etc.).
“In these cases we would place what is called a ‘filter’ in either the IVC (in case of DVT in legs) or SVC (if DVT is in arms/neck veins).”
Inferior vena cava and superior vena cava are known as IVC and SVC, respectively.

IVC filter. BrusBlaus/CreativeCommons
“These devices take 15 to 20 minutes to insert percutaneously and are meant to prevent pulmonary embolism, not formation of DVT.”
Nobody at the hospital mentioned anything about any filter.
The IVC and SVC are “the two largest veins that return the venous blood back to the heart,” says Dr. Gashti.
The filter in these locations would prevent a dislodged DVT from traveling deep enough into the lungs or heart to cause a catastrophic event.
If a loved one is fresh out of surgery, recovering in the ICU or regular hospital room, and it’s discovered they have a DVT (an ultrasound should be ordered if there is swelling in a leg or arm), ask about an IVC or SVC filter!

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How Does Surgery Cause a DVT?
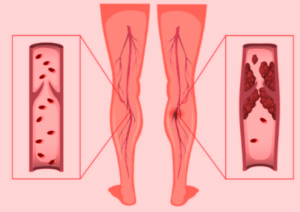
A vascular surgeon explains why most DVTs form during surgery rather than during the immobility after the surgery.
The estimate for annual U.S. deaths from pulmonary embolism (which begin as a deep vein thrombosis) ranges from 50,000 to 200,000.
When a pulmonary embolism is fatal, it’s often a sudden, unexpected death, often attributed to heart attack.
“The difficulty is that you will never know the exact numbers unless you did an autopsy on everyone with sudden death, which is not a practical thing,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“So most of these numbers are estimates, and in my opinion are very conservative.”
Immobility is a major risk factor for a DVT.
This is why after knee replacement surgery, for example, the patient wears surgical stockings and their legs are wrapped in a special device that encourages increased blood circulation at varying intervals.
I was surprised to learn, though, that most DVTs form at the time of surgery. My mother had a DVT in her neck following bypass surgery.
People who take long airline flights in which their legs are crammed immobile in a small space are warned to guard against DVT.
Dr. Gashti explains, “During surgery, especially when you are under general anesthesia, you are completely paralyzed, so you not only are immobile, but also not have any of your muscle tone (muscle pump) that would help with movement of the venous blood from the extremities, thus causing stasis which can lead to DVT.”
When I told my mother this (long after she had recovered from the bypass), she asked why, then, don’t people develop DVT overnight during sleep.
Well, I’m not a doctor, but my response was based on common sense:
We are not perfectly immobile during sleep. When under general anesthesia, yes, we are perfectly immobile because of a chemically induced, very deep unconsciousness—an unnatural state that can mess with blood circulation.
Though some people claim they don’t move at all while asleep, and even awaken seemingly in the same position that they were in when they went to bed, there are still many minute muscle movements and minute shifting while they are asleep.
There may also be myoclonus incidents – sudden jerking of a muscle.
If you’ve ever seen time lapses of people sleeping overnight, they indeed change positions many times. I’ve observed my parents while they were fast asleep.
It’s never long before a foot twitches or a hand or whole arm moves, even though they are asleep.
Sleep is a natural, necessary process, and nature would not have engineered it to cause a DVT.
Symptoms of a Deep Vein Thrombosis
• Swelling where the blood clot is (lower leg, upper leg, pelvic region)
• Cramping or pain in the area (particularly the lower leg, but can also be in the foot)
• The pain does not go away with resting the leg or lying down.
• The suspect area is tender to the touch.
• Redness and/or extra warmth in the affected area
• The color may also be bluish or pale

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Plantar Fasciitis Cause Foot Pain on Outer Side?

A foot care specialist addresses pain on the outer side of the foot being caused by plantar fasciitis.
“Most pain associated with plantar fasciitis originates near the point of insertion of the plantar fascia in the medial area of the calcaneus,” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (www.ipfh.org).
A pedorthist is a medical professional who designs footwear and devices to alleviate foot pain.
The medial side of the calcaneus means inner side of the foot, near the ankle.
When I had plantar fasciitis years ago, I had burning pain along the outer side of my foot, as well as at the medial calcaneus and smack bottom of the heel.
Thompson explains that the plantar fascia consists of inner, central and lateral (outside of the foot) bands of tissue, so that, yes, it is also possible to have inflammation in the lateral (outside) band.
“But if you read the literature, this is unusual,” adds Thompson.
“Plantar fasciitis is most likely to occur in the central band and manifest in pain in the center or medial aspects of the foot in the heel area.”
Whether plantar fasciitis causes pain on the outer side of the foot or the central or heel areas, conservative therapy is the first line of treatment.
This approach typically includes rest to avoid activities that aggravate the condition, along with applying ice to reduce swelling.
Over-the-counter anti-inflammatory medications may help manage pain.
Stretching exercises for the calf muscles and the plantar fascia can improve flexibility and reduce tension.
Orthotic devices, such as custom or over-the-counter arch supports, are used to provide better foot alignment and reduce stress on the heel.
Overnight splints (shown below), which keep the ligament bands stretched, can help immensely.
They come in a variety of styles and are sold online as well as at footcare retailers.

 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Seasontime
6 Causes of Pain on the Outside of Your Foot

A foot pain expert describes the seven possible causes of pain on the outside (lateral) part of the foot.
Pain along the outside or lateral part of the foot can have one (or more) of six possible causes, according to Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (www.ipfh.org).
A pedorthist is a medical professional who designs devices and footwear to alleviate foot pain.
Arthritis
“There are three main joints on the lateral side of the foot – the calcaneal/cuboid, the cuboid/fifth metatarsal, and the fifth metatarsal/proximal phalange joint where the little toe begins,” says Thompson.
“In addition, closer to the center line of the foot are the cuboid/lateral cuneiform, cuboid/navicular and cuboid/fourth metatarsal joints.
“Lateral foot pain can be caused by inflammation (arthritis) in any of these.”
Cuboid Syndrome
“Where the cuboid bone articulates with the calcaneus it forms the calcaneocuboid joint,” says Thompson.
“This joint functions to lock the foot for stability on toe-off. Cuboid syndrome happens when the cuboid gets displaced or dislocated relative to the calcaneus, causing pain when walking or running.
“In cuboid syndrome the joint does not function properly, causing pain and weakness on the lateral side of the foot.”
Tendonitis
Thompson says that several major tendons run through the side of the foot. If any are inflamed, the side of your foot will hurt.
Muscle Strain
“The major muscles on the lateral side of the foot are the flexor digiti minimi and abductor digiti minimi, along with their tendons,” says Thompson.

Shutterstock/Seasontime
“Also, a larger and important tendon, that of the peroneus longus muscle, runs through the lateral side of the foot on its way to be joined to the lateral side of the first cuneiform and proximal end of the first metatarsal.”
Yes, sounds fancy, but a muscle strain indeed can cause pain along the outer side of the foot.
Fracture
“A broken bone in the foot, especially if it is one in the fifth phalanges, the fifth metatarsal or the cuboid will certainly cause lateral foot discomfort!
“The fifth metatarsal is especially prone to avulsion and Jones fractures.
“In an avulsion fracture, a small piece of bone is pulled off the main portion of the bone by a tendon or ligament.
“This type of fracture is the result of an injury in which the ankle ‘rolls’ (common among athletes).
“Avulsion fractures are often overlooked when they occur with an ankle sprain.”
Many years ago I had an avulsion fracture. I sprained my ankle playing volleyball.
In the ER the doctor said that the ligament tear took a small piece of bone with it.
I heard him behind the curtain tell somebody (presumably a nurse), “It doesn’t look good.”
I had pain on the outer side of my foot, but of course, I knew why; the pain on the outer side of my foot wasn’t a mystery. I fully recovered from this sprain.
“Jones fractures occur in a small area of the fifth metatarsal that receives less blood and is therefore more difficult to heal,” says Thompson.
“A Jones fracture can be either a stress fracture (a tiny hairline break that occurs over time) or an acute (sudden) break.
“Jones fractures are caused by overuse, repetitive stress or trauma.
“Pain, swelling, tenderness on the outside of the foot, difficulty walking and bruising may all be symptoms of these fractures.”
Ankle Sprain
I’ve had more than one ankle sprain as an athlete, and they do cause pain along the outer side of the foot.
But at least when an ankle sprain occurs, you know why you have the pain.
“Pain can radiate throughout the lateral side of the foot,” says Thompson.
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/KlaraBstock
Hoarse Voice, Trouble Swallowing: Causes
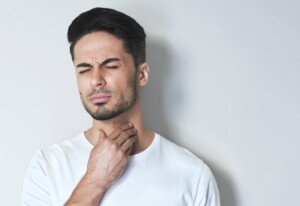
Two doctors explain the possible causes of a hoarse voice coupled with trouble swallowing
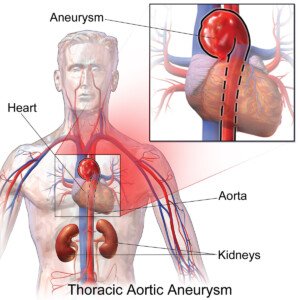
The first expert source for this article about the causes of the symptom duo of hoarse voice and swallowing difficulties is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
You’re probably wondering why a consulting physician for hoarse voice and trouble swallowing would be an aorta specialist, being that the aorta is the largest blood vessel in the body, and arises out of the heart.
“An aortic aneurysm can, rarely, put pressure on the esophagus by virtue of its size,” explains Dr. Elefteriades, “and cause the symptom complex described.”
An aneurysm is a ballooned portion of a blood vessel. When a portion of the aorta is abnormally enlarged, this is an aneurysm.
Think of what a snake looks like after it just swallowed a big egg — the snake’s body is long and tube-like, and the egg inside bulges at some point along the snake’s body.
BruceBlaus/CreativeCommons
That’s kind of what an aneurysm looks like (but not always, as there are different kinds of aneurysms). But you get the picture.
Plus, if the aneurysm is located on the arch or descending portion of the aorta, it can cause compression of the nerve that controls the vocal cords, as this nerve passes along the aorta,” adds Dr. Elefteriades.
This disrupts signals to the vocal cords and will result in a hoarse voice.
If you have trouble swallowing, plus a hoarse voice, chances are that this is NOT from an aortic aneurysm.
Dr. Elefteriades says that these symptoms more commonly arise from “problems with the esophagus,” as well as “benign conditions, like reflux disease.”
Difficulty swallowing and a hoarse voice occurring together can also be caused by tumors, says Dr. Elefteriades.
What does an ear, nose and throat doctor have to say about causes of a hoarse voice?
Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology, says that acid reflux is a common cause of hoarse voice.
But she also includes in the list the following: “Laryngitis, vocal cord polyps or nodules, long-term smoking irritates the vocal cords causing chronic swelling, vocal cancer.”
But what if trouble swallowing is tossed in?
“The most common cause of a choking sensation,” says Dr. Silvers, “is acid reflux, ‘silent reflux’ with our indigestion or heartburn symptoms,” when a foreign object in the throat has been ruled out.
Stomach acid comes up into the back of the throat, making it swell, says Dr. Silvers.
“This makes it hard to swallow. Patients may describe choking sensation or trouble swallowing.” A cough may also be present.
Believe it or not, stress can cause difficulty swallowing and a hoarse voice, because, as Dr. Silvers explains, stress can cause stomach acid to rise up into the back of the throat.
Trouble swallowing, though not necessarily with a hoarse voice, can also be caused by a hiatal hernia.
Both of these symptoms can also be a sign of esophageal cancer.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.