How Many People in Their Mid 30s Get Colon Cancer?

People in their mid 30s get colon cancer.
Many doctors don’t first suspect this in a symptomatic 30ish person, and the disease thus progresses until it’s finally diagnosed.
At the age of 35, the last thing Dr. Stan Frager was worried about was colon cancer.
On family vacation, Stan’s dad noticed that Stan had bleeding in his urine, and recommended that he see a doctor.
Upon returning from vacation, his father called Stan every day until he got screened.
35 too Young?
Stan says, “I only agreed to be examined to get him off my back.” Up until that point, he had been ignoring the bleeding in his urine, figuring it would go away.
But following a biopsy, a doctor informed Stan he had stage three colon cancer; his colon wall was penetrated, and he had a 90% morbidity rate.
“My father saved my life,” says Stan. Following a surgery, he went into stage 5 radiation treatments — the highest treatment available.
Before his diagnosis at age 35 for the colon cancer, Stan was an athlete and the baseball coach at the University of Louisville, Kentucky, where he was also a professor of psychology.
He had spent years in a medical environment and knew his way around the hospital, but never thought to get screened for colon cancer.
After his surgery he spent the rest of the baseball season coaching the team from the dugout, where he sat on a doughnut while he healed.
Despite the grim diagnosis, Stan has been a survivor for 38 years as of March 6, his surgery date.
He now has two full grown children, one of whom is a 28-year-old male who has already had a colonoscopy.
Stan hopes that audiences will take two simple messages away from his story:
- Know the symptoms and signs of colon cancer.
- Get checked out if something doesn’t seem right.
Age 35 is not too young to develop colon cancer.
“I spent 12 years in academia, and I was stupid. My, and many others, most common thoughts are ‘Why me? Maybe it’ll go away. I won’t get cancer.’ Then I did,” says Stan.
“This could have been prevented if I just took my head out of the sand.”
To learn more about this unforgiving disease, visit the Colon Cancer Prevention Project.
How often do people in their 30s get colon cancer?
Of all the cases in the U.S., the percentage of colon cancer patients between 20 and 34 is 1.4 percent; and between 35 and 44 is 4.2 percent.
There are no statistics that precisely define how many people in their 30s each year are diagnosed with colon cancer.
 Update: Stan Frager passed in 2021.
Update: Stan Frager passed in 2021.
Top image: Shutterstock/Antonio Guillem
Source: seer.cancer.gov/statfacts/html/colorect.html
How Often Women with Dense Breasts Should Get Mammogram
Women with dense breasts have a significantly increased risk of breast cancer. Is the yearly mammogram often enough for adequate for tumor detection?
Because dense tissue increases the risk of breast cancer, one may wonder if a woman with dense breasts should have mammograms more often than women without this feature.
“Annual mammogram starting at the age of 40 saves the most lives and is appropriate for women of all breast densities,” says Anjali Malik, MD, a board certified diagnostic radiologist with Washington Radiology in Washington, DC. She interprets mammograms, breast MRIs and ultrasounds, and performs biopsies.
“Breast tomosynthesis [3D mammogram] has improved the detection of small, invasive breast cancers and decreased the ‘false positive’ call-backs,” continues Dr. Malik.
A report in JAMA Internal Medicine (March 2013) says that a study involving over 900,000 women concludes that mammograms once every two years are just as beneficial as annual screenings—even for patients with dense breasts.
The every-two-year screening results in fewer false positives, meaning, fewer indications of malignancy that turn out to be benign.
The researchers (UC San Francisco and Seattle-based Group Health Research Institute) say these recommendations apply to women 50 to 74.
Dr. Malik explains, “In 2013 (the time of the JAMA report), breast tomosynthesis (3D mammography) was not in routine use.
“The 2013 JAMA report was based on 2D analog mammography and prospective data from 1994-2008.
“Currently, 3D digital mammography is in use, and most centers use fellowship trained breast imaging radiologists, where this was not as widespread in the ‘90s and early 2000s. Therefore, this data is near obsolete in 2019.”
What about women in their 40s with dense breasts?
“For women, particularly for those women ages 40-49, who are also more likely to have dense breast parenchyma, nine per 10,000 breast cancer deaths are prevented by annual screening mammograms,” says Dr. Malik.
This data comes from a study by Nelson et al (Annals of Internal Medicine, 164(4):244-55, 2016).
A woman with dense breasts may wonder if more of an important screening tool means better: twice a year mammograms, whether they’re 3D or 2D.
But here’s the problem (other than the extra radiation exposure): Biannual screening increases the call-back rate and the rate of false positives.
This creates tremendous anxiety and sometimes unnecessary biopsies.
Though biannual screening via mammogram has been shown by limited research to result in more cancers detected, it has not been shown to increase survival rates.
Women with dense breasts (as determined mammographically) should ask their doctor about annual 3D mammograms supplemented with annual ultrasounds.
 Dr. Malik is a frequent public speaker and advocate for breast health awareness. She has lectured on the latest advances in breast cancer screening including 3D Mammography™. Follow her on Instagram: @AnjaliMalikMD
Dr. Malik is a frequent public speaker and advocate for breast health awareness. She has lectured on the latest advances in breast cancer screening including 3D Mammography™. Follow her on Instagram: @AnjaliMalikMD
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2013/03/130319144537.htm
Does Back Pain with Chest Pain Mean a Heart Attack?

What are the odds that if you uexplainably feel pain in both your back and your chest that it’s a heart attack?
Perhaps you’ve read that back pain can signal an oncoming heart attack, or occur with the actual heart attack.
Maybe you’ve heard that both back and chest pain can occur with a heart attack.
However, does pain in the back, plus chest, automatically mean that there is something wrong with your heart?
“Not necessarily, but possibly,” says Robert M. Davidson, MD, a cardiologist with SignatureMD.
“If it is associated with exertion or stress, it might be heart related. If it is affected by movement or position, it is more likely to be muscular-skeletal.”
A condition that can cause back and chest pain, upon body position or movement, is costochondritis, an injury to the cartilage in the ribcage. This can hurt pretty bad, but it is benign.
Dr. Davidson continues, “Severe back pain, sometimes radiating to the chest, can be a sign of a leaking or ruptured aortic aneurysm, which is a medical emergency, and should be considered if someone has risk factors such as high blood pressure, older age, or known arteriosclerosis. The type of pain associated with this is often described as tearing.”
A tear in the inner lining of the aorta. Shutterstock
People who have survived a ruptured aortic aneurysm, or aortic dissection, have also described the feeling as “ripping.”
An aneurysm is an abnormally dilated or enlarged section of an artery.
Usually there are no symptoms until the aneurysm tears. Most aortic aneurysms are discovered by accident via imaging for another issue.
Most non-leaking or non-rupturing aneurysms don’t cause symptoms, but when they do, they may consist of chest, back, neck and jaw pain, a hoarse voice, abnormal stethoscope sounds, coughing and shortness of breath.
An esophageal spasm is another possible cause of chest pain that radiates to the back (including between the shoulder blades).
This is a benign (though sometimes very painful) non-cardiac issue and has no known cause.
Keep in mind that you can have both a musculoskeletal problem and a heart problem — both causing chest and back pain!

Dr. Davidson is with the Division of Cardiology at Cedars-Sinai Medical Center, Los Angeles, and has been practicing for 30+ years. Areas of specialty include coronary artery disease, heart attack and palpitations.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ArtFamily
Source: webmd.com/digestive-disorders/tc/esophageal-spasm-topic-overview
How Are Kids and Teens Treated for Blood Clots?

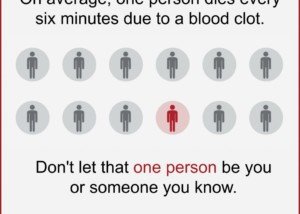
Yes, children, teens and young adults can develop a potentially fatal blood clot, also known as a deep vein thrombosis (DVT).
Even fit kids, under the wrong circumstances, can end up with this serious condition that demands immediate treatment.
Blood clots in kids, as well as in adults, pose a serious risk because they can break loose and travel to the lungs, resulting in a potentially life-threatening condition known as a pulmonary embolism.
When a blood clot lodges in the lungs, it obstructs blood flow, which can lead to sudden and severe symptoms such as difficulty breathing and chest pain.
A pulmonary embolism may cause rapid onset of shortness of breath, sharp or stabbing chest pain, and in some cases, even coughing up blood.
Immediate medical attention is crucial for managing a pulmonary embolism, as prompt treatment can significantly impact the outcome and reduce the risk of severe complications or death.
Young adults and children are not immune to DVT , which is a blood clot in a vein.
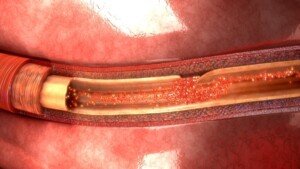
DVT stands for deep vein thrombosis. It’s a clump of blood — a sticky thick network of blood cells — attached to the inner wall of a vein, obstructing blood flow.
“Kids and teens are treated for blood clots according by identifying the underlying cause of the blood clot,” says Dr. Lisa Lewis, MD, a board certified pediatrician in Fort Worth, Texas, and author of “Feed the Baby Hummus, Pediatrician-Backed Secrets from Cultures Around the World.”
“Typically, blood clots are treated with an anticoagulant [blood thinner] and sometimes aspirin.”
Blood thinners would include heparin, or its low molecular weight version, given with warfarin (Coumadin), or just warfarin alone.
The INR blood work is taken on a scheduled basis so that the effect of the anticoagulant drug can be monitored to ensure it stays within therapeutic range.
“Although uncommon, a large percentage of blood clots in children and teens are inherited,” says Dr. Lewis.
What if a child or young adult has an acute, large DVT?
A large deep vein thrombosis can completely obstruct flow of blood from a limb.
In this case, other medications may be used early on, such as a thrombolytic (clot-busting) agent. This would be followed by anticoagulant medications.
Long-term management of deep vein thrombosis (and pulmonary embolism) in kids:
1) The safe prevention of additional DVTs is emphasized
2) Management is designed to enable the young patient to function as normally as possible.
Having 25+ years’ experience, Dr. Lewis completed her pediatrics residency at Texas A&M University Health Science Center, Scott and White Memorial Hospital. For two years afterward she was assistant professor in the department of pediatrics at Texas A&M University Health Science Center.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: The National Alliance for Thrombosis and Thrombophilia newsletter at stoptheclot.org/Newsletters/NATT_Spring_07_Nwsl__web.pdf
12 Causes of Blood Clots and DVTs in Children

There are at least 12 causes of blood clots or deep vein thromboses in children. No age is immune.
Blood clots can occur anywhere in the body, but when they occur in larger vessels, they can become a serious problem.
When it comes to any kind of blood clot anywhere in the body of a child, the list of causes grows.
Not all blood clots are a deep vein thrombosis.
For example, a blood clot can occur in the brain due to head trauma.
There are causes of blood clots and deep vein thrombosis in the pediatric population.
“Genetic clotting disorders are very common,” begins Dr. Lisa Lewis, MD, a board certified pediatrician in Fort Worth, Texas, and author of “Feed the Baby Hummus, Pediatrician-Backed Secrets from Cultures Around the World.”
“Other causes include certain medications, surgery, anomalies of the blood vessels (for example a blood vessel that is not developed properly), immune system disorders, heart disease, immobility due to a medical condition or hospitalization, injuries, infection and cancer.”
Poor Blood Circulation
This can result from excessive inertia or constriction of a vein. Excessive inertia can easily be remedied by imposing limitations on how much time is spent watching TV and sitting around with a smartphone or computer game.
Turn the TV off and tell your child to go outside and play. HOWEVER, the directive of “go outside and play” is often not enough to encourage physical activity in a sedentary child.
But at least squatting down and making mud patties engages more muscles than does slumping on a couch staring at a screen.
Make sure your child has ready access to items that encourage movement: various balls, skates and other implements.
This can even include an air-filled striking bag for kids to have fun punching and kicking at.
A mini trampoline is also an option for older kids to offset inertia — and hence, reduce the risk of blood clots.
Damage to a Vein’s Inner Lining
Catheter placement into a vein can damage the inner lining of the vessel. Certain medications can also have this effect.
When children present with a DVT or pulmonary embolus, a combination of the above potential causes is often present.
Birth Control Pills
“Adolescents on birth control pills are more at risk of clotting disorders,” says Dr. Lewis.
“This is enhanced by smoking. Smoking is an independent risk factor for the formation of a deep vein thrombosis. So is obesity.
“At times a blood clot forms in a child for no apparent reason,” adds Dr. Lewis.
“A blood clot forms for various reasons depending on the cause. In general, a clot forms because of a cause that activates the components of clotting.
“For example, children with genetic clotting disorders may be missing a protein necessary for normal blood flow.”
Having 25+ years’ experience, Dr. Lewis completed her pediatrics residency at Texas A&M University Health Science Center, Scott and White Memorial Hospital. For two years afterward she was assistant professor in the department of pediatrics at Texas A&M University Health Science Center.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
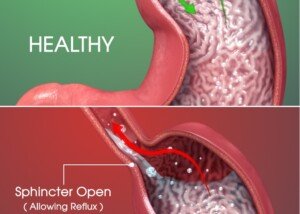
Who Should Have Upper Endoscopy to Diagnose Heartburn?

Too many upper endoscopies are being done unnecessarily, so if you have heartburn (GERD), take notice of this information.
If you’ve been diagnosed with heartburn secondary to GERD, but you have not had an upper endoscopy, have you ever wondered if you need this procedure?
A person may also find themselves tinkering with the idea of an upper endoscopy after learning that years of heartburn can lead to precancerous changes in the esophagus (Barrett’s esophagus).
“GERD or gastroesophageal reflux disease is a very common condition, with heartburn being the most common symptom of GERD — and seen in up to 50% people with GERD,” says Alan Gingold, DO, a board certified gastroenterologist with Central Jersey Ambulatory Surgical Center.
“Not everyone with heartburn needs to get an upper endoscopy,” continues Dr. Gingold.
“Typically an EGD is recommended for anyone who has heartburn that is longstanding (more than five years), symptoms not responding to medication, anyone aged 45 or over who has new symptoms or anyone with alarm symptoms: nausea/vomiting, dysphagia, anemia, blood on stool, weight loss.”
Dysphagia is difficulty swallowing.
Nevertheless, there may still be too many unnecessary endoscopies being done. In 2012, the Annals of Internal Medicine reported this.
Though that was years ago, it’s quite possible that people with heartburn are continuing to get unneeded upper endoscopies.
- After all, ads for heartburn relief continue to regularly air on TV and appear in print media.
- Furthermore, Barrett’s esophagus has received increased publicity.
However, if you seem to have heartburn or even if you were recently diagnosed with this condition, the next step is NOT to gun for the upper endoscopy.
Other Reasons for an Upper Endoscopy
If one’s heartburn doesn’t respond to medication after 4-8 weeks, this may call for an upper endoscopy.
Another reason for this exam is if the patient’s esophagus has a history of tightening or narrowing.
If the patient is over 50, male, has had diagnosed heartburn for at least five years, AND has other risk factors for Barrett’s esophagus – then he’s a candidate for an upper endoscopy.
Other Risk Factors for Barrett’s Esophagus
- Overnight reflux symptoms
- Excess body fat, especially in the belly
- Hiatal hernia
- Tobacco use
This patient may undergo an initial screening test for Barrett’s esophagus or esophageal cancer. If the result is negative, then periodic upper endoscopy is not needed.
What if you have Barrett’s esophagus?
Upper endoscopy should be done every three to five years.
If the patient has dysplasia, the upper endoscopy should be more frequent.
Overuse of upper endoscopy has not been found to improve the health or survival of patients suffering from heartburn.
 Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
Dr. Gingold attributes his success to the extra time he spends with his patients. His areas of expertise include reflux disease, Barrett’s esophagus, capsule endoscopy, chronic liver disease and inflammatory bowel disease. Dr. Alan Gingold is board certified by the American Board of Internal Medicine in Gastroenterology
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/airdone
Source: sciencedaily.com/releases/2012/12/121203183341.htm
What’s the Strongest Risk Factor for a Deep Vein Thrombosis?
You’ll be shocked at what the greatest risk factor is for a DVT (deep vein thrombosis).
If you’re thinking that obesity is the strongest risk factor for a DVT — you’re on the right track as far as the seriousness of this risk factor.
But there’s another one that trumps obesity, says a study.
And that biggest risk factor is the non-O ABO blood type, according to a study that’s published in the Canadian Medical Association Journal.
The report says that this blood type comprises up to 20 percent of risks for VTE (venous thromboembolism).
Data on over 66,000 people, who’d been tracked for 33 years, was analyzed.
But could the ABO blood type be linked to a higher risk of DVT in the general population?
The study authors determined that DVT risk grew when the ABO blood type was combined with the factor V Leiden R506Q or prothrombin G20210A, which are genetic mutations that increase venous thromboembolism risk.
The researchers add that ABO blood type was indeed the most important risk factor in the general population for DVT/PE.
Other Big Risk Factors for Deep Vein Thrombosis
Obesity. “There are probably multiple factors relating to obesity and DVT risk,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.

Freepik.com
Dr. Besser explains, “It is theorized that significant obesity increases the hyper-coagulability of the blood (tendency to clot), especially if the person has a genetic predisposition to clotting (certain blood factors that are inherited can affect a person’s clotting ability).
“Additionally, physical factors, such as immobility (common in the obese) is another factor.”
Smoking. Quit. Just quit. Find another way to deal with stress or boredom.
Excessive sitting. Do you have a sit-down job? Every hour, get up and walk somewhere briskly, or do stationary lunges, squats or high knee marches for several minutes.
No exercise program. Start lifting weights and using cardio equipment, or join a cardio class. Go on hikes, bike rides, etc.
Though the greatest risk factor for a deep vein thrombosis is a blood type that you may not even have, this doesn’t mean that the other risk factors are insignificant. They count big-time.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2013/02/130204130034.htm
sscpywrt26
Low Back Pain Cure with Simple Walking on a Treadmill

A consistent walking program using a treadmill can dramatically reduce or even eliminate low back pain. But if you use a treadmill, there’s a catch.
A report in Clinical Rehabilitation presents conclusions of a walking-study done with participants who had low back pain.
Frequency and Duration of Walking to Effectively Treat Low Back Pain
The program in this study, headed by Dr. Michal Katz-Leurer from Tel Aviv University’s Stanley Steyer School of Health Professions (Sackler Faculty of Medicine), consisted of walking two or three times a week for 20 to 40 minutes at a time.
This walking protocol turned out to be as effective for relieving low back pain as are the typical muscle strengthening exercises that require equipment and often supervision by rehab specialists.
How does walking cure or relieve low back pain?
Few people actually realize that the “core” is involved in walking. I’m a former certified personal trainer, and I’ve told my clients that the core—which is primarily the abdominals and low back—is engaged when one walks.
This is why when some very sedentary people suddenly do a lot of walking, their low back starts aching. These muscles have worked in a way they’re not used to.
Your body doesn’t have to bend in order to engage the core.
However, don’t let the possibility of backache stop you from a regular walking program if you suffer from low back pain.
You may feel some achiness at first, but it will subside sooner than you think as you stick with the program.
It’s like any new exercise to the body; the muscles are adjusting to the new stimulus, and in the process, develop benign aching or soreness. As the muscles get stronger or adapt, they will no longer get sore.
How the Study Was Done
Twenty-six people completed a muscle exercise program, and 26 others completed a walking program.
All participants had low back pain, and both programs lasted six weeks.
At the end of six weeks, both groups had great improvement in their condition.
How to Properly Use a Treadmill to Alleviate Back Pain
In order for walking to effectively treat low back pain, it must be done with correct biomechanics.
This means if you use a treadmill, DO NOT HOLD ON — other than for momentary steadying such as when drinking water.

Shutterstock/Khakimullin Aleksandr
Otherwise, when your hands are latched onto the sides or front, even lightly, this disrupts the natural gait pattern and can make low back pain worse, as well as cause new pains elsewhere in the body, such as in the hips, knees and feet.
If your back hurts more upon walking on a treadmill, this is because your lumbar muscles are being engaged. This achiness will especially occur if you use an incline without holding on.
This is because when you walk on a slope or incline, without holding on, your lower back muscles work to prevent you from falling backwards!
If you hold on, this will relieve the soreness or aching, but holding onto the treadmill is WRONG!
Keep walking without holding on, and that aching in your low back will vanish. Give those weak, out of shape muscles a chance to get strong and reliable!
Use a SLOW pace and medium to low incline. There is no need to crank the machine up to 15 percent and run the tread at 4 mph, which is too difficult to sustain a walk without holding on.
But holding onto a treadmill at ANY setting will cheat your low back from the work it needs to help prevent or eliminate pains and aches.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com/shayne_ch13
Source: sciencedaily.com/releases/2013/03/130305131404.htm
How Long Can “Stool Beeturia” Last?

Here is what a GI doctor says about how long beet juice in one’s stools can last.
Beet juice in the stools, to some, is “cool,” but to others, is very frightening, as this can masquerade as blood in the stools.
In medicine, “beeturia” refers to the unabsorbed crimson pigment of this vegetable, called betanin, in a person’s urine, not their bowel movements.
If you’re seeing red in your stools three or four days after eating whole beets or beet juice, it might be tempting to start thinking that this is blood.
The betanin comes out in the urine, which comes out with your poops, creating the illusion that your BMs themselves are reddish.
What’s actually happening is that your stools are surrounded by the urine that has the beet pigment in it.
Of course it’s going to get on your bowel movements.
But can this “stool beeturia” still occur five days after you ate the beets or drank beet juice?
Yes — because I myself have had it five days out.
I might also add that I had the beeturia five days in a row, rather than skipping the first four days and then seeing it on day 5.
“In the stool it’s also generally two days, but maybe three or four,” says Jonathan Zinberg, MD, chief of gastroenterology at South Nassau Communities Hospital, Oceanside, NY.
“It is more likely to occur in those who have increased iron absorption, such as those with iron deficiency.
“But remember, not all biologic specimens (i.e., people) follow the rules, so there can be variability.”
For a more in-depth — and reassuring look at this phenomen, read my other article:
Red Stools from Beets vs. from Blood: How to Tell the Difference
 Jonathan Zinberg, MD
Jonathan Zinberg, MD
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Volosina
Sharp Sudden Pain in Upper Arm: Non-Cardiac Cause

Find out what can likely cause a sudden sharp pain in the upper arm that’s not related to your heart.
If you’ve been experiencing episodes of a sudden and sharp pain located in your upper arm, this may very possibly be a condition called long head biceps tendonopathy.
This is when the tendon of the long head of the biceps is torn; it may or may not cause pain.
If you have LHB tendonopathy, you may also have a shoulder problem, namely, a rotator cuff tear.
A torn rotator cuff, as well, can cause a sudden sharp pain in the upper arm.
However, these aren’t the only musculoskeletal causes of a sudden sharp pain in the upper arm; hence, a thorough examination, which includes radiographic imaging, will be necessary for precise diagnosis.
The treatment for long head biceps tendonopathy may be surgical or nonsurgical, says Shane Nho, MD, a Chicago-based orthopedic surgeon.
His report appears in the Nov. 2010 Journal of the American Academy of Orthopaedic Surgeons.
Statistics & Trends
-There’s no big difference in patient satisfaction or function between the two main surgical options, which are biceps tenotomy and tenodesis.
-The complication rate from surgery is less than 1 percent.
-Both surgeries can be performed via arthroscopy.
-The JAAOS report urges the pursuit of nonsurgical treatment at first, as this may suffice for ending the upper arm sudden pain and other related issues.
-Younger, active patients should undergo the biceps tenodesis if surgery is warranted.
Conservative Treatment for Long Head Biceps Tendonopathy
Rest, avoiding and/or modifying the offending activity, taking anti-inflammatory drugs, and physical therapy.

Shutterstock/Photographee.eu
If these don’t work, then corticosteroid injections may be done, though these may put a patient at risk for tendon rupture, depending on site of injection.
Besides sudden sharp upper arm pain, long head biceps tendonopathy can also cause the following symptoms:
-Audible snapping or popping in the elbow or shoulder
-Biceps cramping resulting from strenuous use
-Bruising from the middle of upper arm down towards elbow
-Tenderness, pain and/or weakness at elbow or shoulder
-Difficulty turning palm up or down
-Funny bulge above the elbow (from flaccid muscle)