Amitriptyline for IBS: Pros & Cons

A GI doctor discusses the effectiveness of amitriptyline for IBS, how it works and possible drawbacks.
Amitriptyline and Irritable Bowel Syndrome
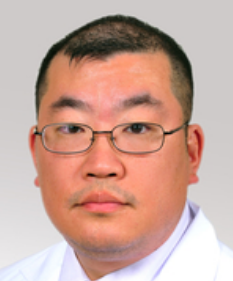
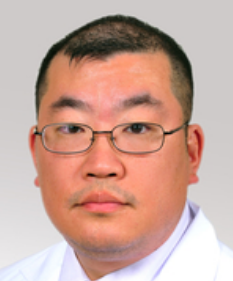
“Amitriptyline is a very common drug used to treat IBS, and can be very effective,” says Michael Blume, MD, a gastroenterologist at MedStar Good Samaritan Hospital, Baltimore.
He says that amitriptyline is usually taken at bedtime and in low doses.
“If you do get prescribed this drug, be aware that it has been used as an antidepressant (as well as for other symptoms, such as migraines, etc.), so the package insert may state that it is an antidepressant drug.
“Do not be alarmed; this is a different use of the drug, and in usually in a much lower dosage than what was used for depression.”
For IBS, amitriptyline works in multiple ways, says Dr. Blume.

Amitriptyline
“It is a very good gastrointestinal analgesic, and it also may decrease spasm in your GI tract, which may help your symptoms.
“Like any drug, there is no drug that does not have side effects, so when one makes a decision to take any medication, one needs to weigh benefits and risks, i.e., what the risk is of taking the drug vs. the risks of not taking the drug.”
Side Effects of Amitriptyline
“The more common side effects include drowsiness, as well as possible palpitations,” says Dr. Blume.
“It should be used with caution in older people and should be avoided in patients with cardiac rhythm problems.”
Remember, IBS is a diagnosis of exclusion, meaning, you should have a colonoscopy (among other important tests) before you’re definitively diagnosed with IBS.
If you’ve been diagnosed with IBS, but it has not responded to treatment, and you have not had a colonoscopy, it’s possible that you actually have microscopic colitis.
The treatment for microscopic colitis is very different than it is for IBS, and that means no amitriptyline.
 In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
In practice for 25+ years, Dr. Blume treats over 65 conditions including abdominal pain, appetite loss, blood in stool, celiac disease, colon cancer, esophageal and liver disease, gas and IBS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Dragana Gordic
Do Pacemakers Prevent Atrial Fibrillation?

Do you have a pacemaker and are wondering if it can also prevent atrial fibrillation?
A-fib is a common heart rhythm disorder that puts a person at considerably increased risk of a blood clot — which could lead to a heart attack or a stroke.
“Pacemakers do not prevent atrial fibrillation, or at least that is not an accepted clinical indication for implantation of a pacemaker,” says Lawrence Kanner, MD, Director, Electrophysiology/Arrhythmia Services, South Nassau Communities Hospital.
He further explains, “Pacemakers are devices that prevent slow heart rhythms. They will allow the heart to go as fast as it wants.
“If your heart wants to go 200 beats a minute (either top or bottom chamber — atrium or ventricle), a pacemaker for the most part just watches.
“But a pacemaker will never let the heart go slower than its programmed lower rate.
“However, modern pacemakers will detect episodes of atrial fibrillation, as long as there is a lead (wire) in the atrium.”
Thus, don’t ever assume that somebody can’t possibly experience an episode of atrial fibrillation just because they have a pacemaker.
A doctor who suspects that a patient has an abnormal heart rhythm will want that patient to wear a portable EKG.
With this portable EKG, every time the patient feels a suspicious symptom (such as a sudden pounding in the chest), they press a button and the device will record the electrical activity of their heart at that moment.
This data is then eventually printed out and interpreted by a cardiologist.
More on Atrial Fibrillation
A-fib. BruceBlaus
The patient may feel what they describe as palpitations: an erratic heartbeat, or the sensation of the heart “flip flopping.”
The patient may also report a reduced capacity for exercise, or an unexplained fatigue.
Feeling lightheaded or dizzy are two more symptoms of atrial fibrillation.
This heart rhythm disorder can also cause pain in the chest.
These symptoms have many other possible causes, and not always heart related.
Atrial fibrillation is a risk factor for ischemic stroke, so if you’re having any of these symptoms — see a cardiologist.
Dr. Kanner cares for patients with a variety of cardiac rhythm disorders plus congestive heart failure, with medications, pacemakers, defibrillators and the latest in advanced cardiac ablation techniques.
cares for patients with a variety of cardiac rhythm disorders plus congestive heart failure, with medications, pacemakers, defibrillators and the latest in advanced cardiac ablation techniques.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Steven Fruitsmaak
TIAs: Why Aren’t More Family Doctors Vigilant on Follow-ups?
Why don’t more doctors take seriously a transient ischemic attack (TIA)?
A TIA (transient ischemic attack) is very serious – it’s your body’s way of warning you that a stroke may be imminent.
A suspected TIA should be treated as an emergency — because it’s a harbinger of a stroke in the near future for many TIA patients.
Among other permanent disabilities, a stroke can cause paralysis on one side of the body.
Amazingly, it is not all that uncommon for a person to report to his general doctor recent symptoms that sound very suspiciously like a transient ischemic attack.
The doctor sends the patient home with no treatment plan, and instead, tells the patient that he’ll get back to him after consulting with a neurologist.
So what’s this patient supposed to do in the meantime to minimize another TIA or even stroke? Cross his fingers?
Seems to me that if a patient reports TIA like symptoms to a doctor, and the doctor suspects a transient ischemic attack, this doctor should be hopping on the case, immediately putting in an order for a brain, heart and carotid artery scan to explore confirming evidence and location of the transient ischemic attack.
But some physicians won’t get hopping like this.
Instead, they make the patient wait until the physician has heard back from the neurologist. There is alarming laxity here.
“This speaks to the systemic flaw that pervades all healthcare: more attention to the acute problem rather than addressing or preventing the underlying cause,” explains William R. Davis, MD, cardiologist and author of “Wheat Belly.”
So what’s behind a TIA, then?
“The underlying cause is usually atherosclerosis,” says Dr. Davis.
“The standard response to atherosclerosis of the carotid artery, for instance, is aspirin, other platelet-blocking drugs like Plavix, and cholesterol reducing drugs.
However, there are plenty of other strategies that can be pursued that can substantially reduce or eliminate the risk of future TIAs.”
Symptoms of a transient ischemic attack are pretty much identical to symptoms of a stroke.
In fact, another name for TIA or transient ischemic attack is “mini-stroke.”
A TIA is a temporary obstruction of a blood vessel in the brain, formed by either a clot of blood, or plaque debris originating from the carotid or aortic artery.
TIA symptoms: sudden onset of numbness, weakness, heaviness or paralysis on one side of the body; loss of balance; cognitive change or confusion; double or blurred vision, or the sensation of a curtain coming over the eye or blindness; dizziness; headache; slurred speech or difficulty talking.
If you suspect you just had a transient ischemic attack, head straight to the ER. The risk of stroke following a TIA is greatest within three days of the TIA.

Dr. Davis is founder of the Track Your Plaque program for heart disease prevention and reversal.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
sscpywrt26
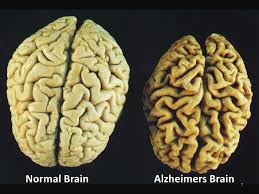
Do Migraine Headaches Increase Alzheimer’s Risk?
Migraine headache sufferers may be fearful that this condition raises Alzheimer’s disease risk, because migraine headaches are associated with a higher incidence of small lesions within the brain that are picked up by MRI.
Interestingly, according to a study involving 780 people over the age of 65, having repetitive and significant headaches, or migraines, does not increase the risk of this disease.
In fact, migraines were shown not even to increase the odds of cognitive decline (cognitive decline doesn’t necessarily mean Alzheimer’s or eventual Alzheimer’s).
This research conclusion comes from Inserm and Université Pierre et Marie Curie, Paris.
It is a fact that in people with a migraine headache history, more of these people, when compared to the general population, have lesions in the microvessels of their brains.
However, such lesions are a universal finding in the elderly population.
The severity, though, varies quite a bit from one person to the next, and they are more severe among people with a history of migraine headaches.
Do you suffer from headaches?
“As an Alzheimer’s specialist, I can say that I have never seen any relationship between headaches or head pain and the development of Alzheimer’s,” says Dr. Robert Williams, MD is a family medicine doctor and geriatrician in Lakewood, Colorado and is a medical advisor for eMediHealth.
Dr. Williams explains, “One should be more concerned about a sedentary lifestyle, smoking, obesity and social seclusion.
“For the most part, activities that increase the risk for heart disease and hypertension also increase the risk for dementia.
“One type of dementia is specifically due to having multiple small strokes over a lifetime which is typically due to poorly controlled cardiovascular disease.”
Lower the Risk of Alzheimer’s
- Stop smoking or don’t start.
- Lose weight if you have excess body fat.
- Limit drinking.
- Maintain a normal blood pressure.
- Avoid excess dietary sodium.
- Work out regularly.
- Limit processed foods.
- Get annual heart checkups after age 50.
- Keep intellectually active.
Based in Lakewood, CO, Dr. Williams has been in practice for over 19 years. In addition to Alzheimer’s disease, Dr. Williams’ areas of expertise include neurology, pulmonology and autoimmune disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Source: sciencedaily.com/releases/2011/01/110119120400.htm
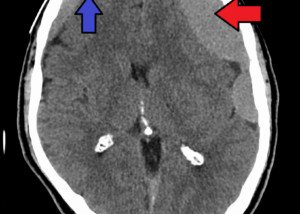
Can Daily Aspirin Cause Chronic Subdural Hematoma in Elderly?

Since aspirin is a blood thinner, how likely could this drug trigger a chronic subdural hematoma in an older person who’se on a daily aspirin regimen?
The issue becomes mighty tricky when an elderly person must take aspirin every day, and at the same time, is at risk for chronic subdural hematoma.
Being elderly, in and of itself, is a risk factor for chronic subdural hematoma.
“As a blood thinner, daily aspirin use can increase the risk for subdural hematoma formation in the elderly,” says Kangmin Daniel Lee, MD, a neurosurgeon with New Jersey Brain and Spine.
“Commonly, chronic subdural hematomas start out as small acute subdural hematomas,” continues Dr. Lee.
“Over time, they become chronic.” They can also slowly bleed over time, versus the kind that a boxer or skier might suffer, in which the bleeding is rapid and deterioration comes quickly.
“As people age, brain atrophy occurs and brain volume decreases. Since the elderly are at increased risk for falls or other minor traumas, there is an increased risk that such traumas could tear a small bridging vein and result in a hemorrhage,” explains Dr. Lee.
Atrophy means shrinkage; the brain has a tendency to shrink as a person gets older.
Dr. Lee continues, “Because aspirin is such a common and often necessary medication for those with a history of stroke or cardiac disease ( i.e., a cardiac stent), the immediate or near immediate risk of a bad event such as a repeat stroke or stent occlusion will often outweigh the remote risk of a subdural hematoma.”
The reason aspirin increases risk of chronic subdural hematoma is because aspirin thins the blood; thin blood is more likely to bleed (less likely to clot).
Blood thinners are a godsend for people at risk for clotting disorders, which can be life-threatening if not treated promptly.
But to prevent clotting (i.e., stroke, heart attack, deep vein thrombosis), the risk then goes up for chronic subdural hematoma, which translates to slow, gradual formation of a mass of blood beneath the dura of the brain.
“I believe that the risk of subdural hematoma is probably under-emphasized with the elderly patient who takes aspirin, and should be more widely discussed.
“Certainly when a neurosurgeon sees an elderly patient who has been on aspirin and has developed a chronic subdural hematoma, there is a thorough discussion of the risk of a repeat hemorrhage.”
How true.
The possibility of chronic subdural hematoma was never mentioned to my elderly mother after it became clear to hospital staff that she was at risk for falling due to orthostatic hypotension; she was recovering from coronary bypass surgery and was on daily aspirin … and also on the king of blood thinners, Coumadin!
Six and a half weeks after surgery, she blacked out while standing in the bathroom, fell dead-weight and hit her head on the bathtub.
No symptoms…until six weeks later when she awakened with the worst headache she’d ever had, and compromised function of her legs.
Diagnosis in the ER later that day: chronic subdural hematoma!
“Also, chronic subdural hematomas can often go unrecognized, as patients can often be minimally symptomatic,” says Dr. Lee (who was not my mother’s neurosurgeon).
“With the general population living longer and getting more medical attention, the reported incidence of chronic subdural hematoma will likely increase, and greater scrutiny will likely be placed on the routine use of antiplatelet agents (like aspirin).”
Dr. Lee focuses on minimally invasive techniques to treat traumatic and degenerative diseases of the spine and brain tumors. He’s been invited to speak at the regional and national levels on his research areas.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Masha Petrakova
Spontaneous Subdural Hematoma in the Elderly: Incidence?

Chronic subdural hematoma can occur spontaneously and being elderly is perhaps the No. 1 risk factor for developing this condition.
It is not to be confused with acute subdural hematoma from a car accident, skiing accident or other significant blunt force trauma to the head.
My mother developed a chronic subdural hematoma as a result of striking her head on the bathtub after passing out while standing at the sink – from a drop in blood pressure.
Her neurosurgeon informed me that chronic subdural hematoma was “not uncommon in the elderly,” and that it can occur “spontaneously” due to weakened bridging veins, and brain atrophy.
If elderly people take daily aspirin or other anticoagulants, this increases risk even more.
So based on my conversation with my mother’s neurosurgeon, spontaneous chronic subdural hematoma in the elderly is far from a rare occurrence, and this made me wonder why there’s no media attention to this.
I never heard of this condition until my mother developed it, and I write medical articles for a living.
I receive Kaiser Permanente’s monthly magazine which highlights common conditions of the elderly (diabetes, heart disease, osteoporosis, osteoarthritis, dementia), but never have I seen anything on spontaneous (or otherwise) chronic subdural hematoma.
Kangmin Lee, MD, says that the occurrence rate of spontaneous subdural hematoma, compared to non-spontaneous causes such as getting hit in the head or heavy drinking, in the elderly is 30 percent.
This sounds like a lot.
“Thirty percent seems like it would be fairly common,” continues Dr. Lee, a neurosurgeon with New Jersey Brain and Spine.
“However, the overall incidence of chronic subdural hematoma in the entire population is approximately one to five per 100,000.
“So it would be 30 percent of that number (the one to five) that would fall into the spontaneous cSDH number.
“With respect to other medical issues such as heart disease and cancer — it is less common. However, as our elderly population continues to grow in number, we will likely see the incidence numbers start to rise.”
The elderly are particularly prone to falling, either due to weakened hip bones, general leg weakness, transient ischemic attacks, and miscellaneous factors such as orthostatic hypotension (plummets in blood pressure after standing from a seated position that can cause a blackout).
The elderly are also more likely to be on anticoagulant therapy, like my mother was (daily aspirin and Coumadin at the time she fell), after undergoing coronary bypass surgery (as did my mother).
And then there’s the age-related brain shrinkage.
Combine these factors, and it would not be accurate to say that chronic subdural hematoma is rare in the elderly population, but more accurate to say that spontaneous chronic subdural hematoma in the elderly (patient has no risk factors other than old age) isn’t particularly prevalent.
Dr. Lee focuses on minimally invasive techniques to treat traumatic and degenerative diseases of the spine and brain tumors. He’s been invited to speak at the regional and national levels on his research areas.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Does Benign Multiple Sclerosis Actually Exist?

“While it is true that many people with multiple sclerosis have a ‘benign’ course, it is difficult to predict who will be in this lucky group,” says Dr. Kantor.
“There is a lot of controversy surrounding the classification of benign multiple sclerosis,” says Daniel Kantor, MD, director of the Neurology Residency Program, Florida Atlantic University.
Dr. Kantor explains, “While it is true that many people with multiple sclerosis have a ‘benign’ course, it is difficult to predict who will be in this lucky group.
“This is why many of us MS specialists see ‘benign multiple sclerosis’ as an after-the-fact diagnosis that can only be made retrospectively.”
MS occurs when the immune system turns against itself, and attacks the sheath that covers nerves and the nerves themselves. This disorder can come and go, yet also rarely leave people bedridden.
I’m a certified personal trainer and one of my clients had multiple sclerosis in remission; she was able to perform all sorts of workout routines.
Sometime after our sessions ended, I heard she had a relapse and was temporarily bedridden.
“There are probably many more people with multiple sclerosis than the 450,000 in the U.S. (and 2.5 million worldwide) commonly quoted,” says Dr. Kantor.
“Firstly, this is an old number from a study years ago; multiple sclerosis remains under-recognized and most people with MS live and die (after a normal life) with multiple sclerosis and don’t even know it.
“Most people with multiple sclerosis do extremely well and respond dramatically to the disease modifying agents (mostly injectables).”
Many famous people have MS, and perhaps the most famous contemporary person who has it is talk show host Montel Williams. Other famous people with MS include:
Neil Cavuto, Fox News Channel anchor; Lena Horne, actress/singer; Alan Osmond, one of the Osmond brothers; and Richard Pryor, comedian.
“There is another problem with the ‘benign’ multiple sclerosis category,” continues Dr. Kantor.
“Even if someone has no problem walking or feeling, they may have invisible symptoms that others don’t recognize or acknowledge.
“This can be very frustrating for the person with multiple sclerosis and they certainly wouldn’t call it ‘benign.’”
Symptoms of MS include: numbness or weakness in a leg or arm, usually beginning on one side of the body or both legs or both arms at the same time; vision problems (though rarely complete loss); pain; tremors and balance/gait problems; fatigue and dizziness.
When someone speaks of benign multiple sclerosis, perhaps they’re thinking in terms of mortality; MS rarely is fatal, and has been called the “best” nerve disease to have, since many other nerve diseases are terminal.
Dr. Kantor is also President Emeritus, Florida Society of Neurology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Does Teen Obesity Cause Migraine Headaches?

Are you an overeight or obese teen who suffers with migraine headaches? Ever wonder if your size might be contributing to this painful condition?
If you’ve been struggling to manage your food portions or choices of food in an effort to lose weight, you now have an added incentive.
And that is this: Excess body fat is clearly associated with migraine headaches.
And as if that weren’t enough, teens who smoke and don’t get much exercise also happen to be more likely to get migraine headaches.
So how much, then, are teens more likely to have migraine headaches when compared to peers who are of a normal weight, exercise and don’t smoke?
They are 3.4 times more likely to have frequent headaches.
Three Variables
1) Overweight, 2) Lack of exercise, and 3) Smoking.
The study showed that in teens with all three of these variables, 55 percent had frequent headaches.
Of teenagers without these negative factors, 25 percent had frequent headaches.
Teens who were only overweight were 40 percent more apt to get frequent headaches than teens without the negative factors.
Smoking teens were 50 percent more likely to experience frequent migraines..
Teens who exercised fewer than two days per week were 20 percent more likely to get frequent headaches than those who exercised a minimum of twice weekly and who were not overweight nor smokers.
These study results come from interviews of 5,847 teens age 13 through 18, part of the Nord-Trøndelag Health Study in Nord-Trøndelag county in Norway.
Nurses interviewed the teens about headaches, exercise and smoking, and took weight and height measurements.
Obesity and Headaches
“Obesity is a risk factor for migraine headaches because of the link with adiponectin,” says Dr. Tiff Jumaily, MD, a board certified pediatrician with Integrative Pediatrics and Medicine.
“Adiponectin is a hormone released from fat cells which modulates inflammatory mediators in migraines.
“Adiponectin is protective against dyslipidemia, insulin resistance and atherosclerosis.
“It releases IL-10, an anti-inflammatory cytokine, and inhibits pro-inflammatory cytokines.
“Greater concentrations of fat cells will inhibit the release of adiponectin which can increase the risk for migraine.
“Paradoxically, a sudden increase in adiponectin levels can also trigger migraine.”
Basic Weight Loss Tips for Overweight Teens
Increasing your exercise is a lot easier than quitting an addiction to smoking or cutting back on your favorite foods, though exceptions do exist.
A smoker may find it easier to just quit smoking than to take up exercise.
Nevertheless, exercising more will inspire healthier eating habits and suppress the craving for a smoke. The result will be weight loss.
Don’t worry that quitting smoking will cause weight gain. If you exercise and eat less junk food and more healthy food, you should not gain fat.
Spend less time sitting before the TV and computer if you’re concerned that quitting smoking will put on weight or increase your appetite.
Remind yourself that giving up smoking can mean no longer suffering from so many migraines.
Teens should remind themselves that exercise might be just the very trick to end migraines…or at least cut down the frequency.
Tips on Exercise if You’re a Teen Who Needs to Lose a Lot of Weight
You should find an aerobic type of exercise that you can stick to. This can be walking, inline skating, using a stationary bike, going up and down a staircase, doing step drills on just the bottom step of a staircase, or following along to exercise videos.
Keep well-hydrated to prevent the so-called dehydration headache.
And add in extra activity every chance you can get. For instance, walk the dog more frequently, for longer distances and at a faster pace.
Ask your parents to buy you some exercise devices such as a heavy ball, a few pairs of dumbbells and/or a set of resistance bands. There’s a ton of very portable exercise equipment sold online.
Ask your parents to get you a gym membership. Then start picking up some weights, jogging around the track if there’s one, and taking some group fitness classes.
If you can’t join a gym, you can still do home exercises such as the ones depicted below.

Lunge. Do it in one spot as well as walking.

Squat. Go up and down up to 20 times.
Yoga. You can start off with beginner poses and hold them for up to a minute.
Additional exercises at home: marching in place, jogging in place, leg kicks and swings, jumping jacks, knee pushups.
Losing weight is not about feeling imperfect.
It’s about improving your health and fitness, as well as reducing your experiences with migraine headaches.
The full report is in the online Neurology (August 18, 2010).
 Dr. Jumaily is a board certified pediatrician and fellow of the American Academy of Pediatrics. She has a thriving pediatric practice in Los Angeles, where she integrates allopathic medicine with integrative and holistic options to treat the whole child and help them thrive.
Dr. Jumaily is a board certified pediatrician and fellow of the American Academy of Pediatrics. She has a thriving pediatric practice in Los Angeles, where she integrates allopathic medicine with integrative and holistic options to treat the whole child and help them thrive.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos.com
Source: sciencedaily.com/releases/2010/08/100818161445.htm
Can Left Side Neglect Be Temporary?

Once a person develops left side neglect, will this usually be permanent or can it be a temporary condition?
Left side neglect is a fascinating neurological problem in which the patient lacks full awareness of his left side or part of the left side, as well as diminished awareness of inanimate objects that are leftward relative to wherever the person is in space at the moment.
My mother had left side neglect as a result of a chronic subdural hematoma on the right region of her brain that had resulted from hitting her head from a fall (in combination with being senior-aged and, most likely, the blood thinner she was on at the time).
Left neglect is more commonly the result of a stroke to the right area of the brain.
In the case of my mother, the problem was temporary.
But it had us unnerved when we realized the extent of it, after she was moved to a skilled nursing facility, a less-controlled, less-restricted environment than a hospital room where she spent just about all her time in bed.
If you clicked on this article, you already know what “left neglect” is, and most likely have been diagnosed with it, or know someone who has.
In the case of a stroke, left side neglect can be permanent, because a stroke is caused by oxygen depletion to brain cells, and once brain cells are starved long enough from oxygen, they cannot be brought back to life.
In my mother’s case, blood and cerebrospinal fluid were on the surface of her brain; the cells were still getting oxygen, but this fluid was creating a veil or fog over the cells, impairing neurological functioning.
As her body resorbed the fluid, the symptoms of the spatial neglect began disappearing.
The spatial neglect, at its worst, affected my mother’s ability to use a walker, maintain a linear walking path, and make turns without bumping the left side of the walker into baseboards.
Her left hand was orthopedically able to hold onto the walker, but it would keep slipping off because she lacked sufficient awareness of that side.
She’d end up trying to use the walker with one hand. But even when both hands were on it, she’d accidentally bump the walker into walls on the left side.
She was off the walker by evening; it was an impediment, actually, yet when she walked down the corridor, she had a tendency to veer to the right, and had no interest in anything to the left.
At the hospital in her room, seating for visitors was to her left, and often, she “ignored” me when I spoke to her when to her left, unless I raised my voice to call her name, and then she’d look at me as though suddenly hearing me.
I’d also get her attention by moving closer and more in front of her, though at the time, I didn’t know that this was the spatial neglect at work.
Currently, there is no sign of left side neglect in my mother, and the physical therapist who visited her home recently for an assessment, said that my mother didn’t need any home visits with a physical therapist, even.
Her left neglect did not disappear overnight, but there was a spike in improvement about 10 days after she was diagnosed with it.
When she came home from the nursing facility, she still had a tendency to drop things occasionally with the hand, but that problem soon disappeared.
At present, you’d never know that my mother once had a bizarre neurological phenomenon known as left neglect, also called spatial neglect.
In hindsight, I realize that left side neglect was at work prior to her second burr hole drain for the hematoma; at home she stated she wanted to lie on the futon in the dining room. From the kitchen this requires a left turn.
She exited the kitchen and began entering the living room, which is right. I had to physically steer her left into the dining room; classic left side neglect, fascinating phenomenon.
Left side neglect can be mild, moderate or severe. If you know someone with this condition, or have it yourself, there is hope, as there are multitudes of therapies to help overcome this condition.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: ncbi.nlm.nih.gov/pubmed/16408519
Top image: Shutterstock/Blue Planet Studio
Can Exercise Prevent Chronic Subdural Hematoma in Elderly?
Is it possible for exercise to prevent an elderly person from ever getting a chronic subdural hematoma?
“As we get older our brains shrink,” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
“This happens to everyone, but happens quicker in some people than others.
“When the brain becomes smaller this leaves more space between the brain and the bones of the skull.
“This leads to stretching of the bridging veins and greater movement of the brain within the skull vault.
“To give an analogy. Think of a poorly packed box in the trunk of your car. The contents will rattle around more and be more likely to get damaged than if they were well-packed.
“Cerebral atrophy is not thought to be a reversible process, so it is crucial to prevent it where possible and to minimize its progression.”
Risk factors for chronic subdural hematoma include brain shrinkage (atrophy), old age, getting bumped in the head and daily use of blood thinners.
But one need not get bumped in the head, or be on blood thinners, to suffer a spontaneous chronic subdural hematoma.
The aging brain has a tendency to shrink, and so does the brain in people who never exercise.
An atrophied brain creates more space between the brain and the skull, which provides more room for a chronic subdural hematoma’s fluid to take up space – and hence create symptoms which require surgery to remedy.
To keep the brain healthy, Dr. Beatty recommends healthy lifestyle choices to reduce the risk of ailments that lead to brain atrophy.
These include avoiding smoking, minimizing alcohol intake, avoiding high blood pressure, and taking measures to prevent or remedy obesity.
“Exercise is another weapon in the fight to prevent cerebral atrophy,” says Dr. Beatty.
“It’s been shown that exercise increases blood circulation to the brain and slows the rate of cerebral atrophy.
“I think exercise may well have another benefit with regard to subdural hematoma prevention.
“Someone who is physically fitter is less likely to have the falls that cause the head injury which causes the subdural.”
Exercise and Brain Shrinkage
It’s been well-established that exercise prevents brain shrinkage in animal studies, and even human studies have demonstrated this.
There is a study that shows that moderate exercise over one year can increase the size of the hippocampus of the brain in older people.
This study, however, didn’t look at chronic subdural hematoma; it looked at spatial memory.
But the fact remains that exercise increased brain size, albeit only a particular portion of the brain.
The hippocampus study was carried out by researchers at the University of Illinois, University of Pittsburgh, Ohio State University and Rice University, and focused on older people who already had hippocampus shrinkage (atrophy).
The hippocampus is responsible for memory.
The study involved 120 inactive older subjects who did not have dementia.
They were placed in two groups: One group walked for exercise (40 minutes daily, 3x/week), and the other group simply did toning and stretching exercises.
Prior to the study, MRIs were taken of the subjects’ brains. MRIs were then taken six months into the study, and at the end of one year.
The group who exercised had a volume increase of the right and left hippocampus.
And get this: In the second group, the hippocampus decreased in volume! I.e., lack of exercise = brain shrinkage.
Another study showed that exercise increases the number of small blood vessels in the brain. (Radiological Society of North America [Dec. 2, 2008]; “Exercise Helps Prevent Age-related Brain Changes In Older Adults”)
If a brain has more small blood vessels, perhaps this can have a protective effect against a slow brain bleed, though there have been no studies specifically investigating this.
The bottom line, though, is that exercise is crucial for optimal brain function and integrity, and these benefits will extend into old age.




























 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for 




































