Lose 100 Pounds with a Treadmill: No Jogging

Here are instructions on how to lose 100 pounds using a treadmill without running.
One reason you have not lost weight despite spending a lot of time on a treadmill is because you’ve been holding onto the device.
This is a very common way that people of all sizes use a treadmill, but it’s almost universal among obese users.
And it begets MINIMAL results. Minimal. Do you know what “minimal” means when you’re trying to lose 100 pounds? You cannot afford minimal!
Now, if you walk without holding onto the treadmill, but continue to eat far more calories than your body can burn off…you will not lose the weight you want to get rid of.
However, if you’ve been faithfully sticking to portion control and to treadmill workouts…without seeing much of a change in your body, I’ll bet the entire farm that you’ve been holding onto the machine this whole time.

So very wrong.
Losing 100 Pounds with a Treadmill Requires More than Letting Go
In addition to swinging your arms, you must also employ a technique called high intensity interval training if you want to drop a hundred pounds.
You can do this by walking.
Jogging is not necessary.
But you must embrace keeping your hands off of the machine (unless you want to temporarily steady yourself while sipping water).
Treadmill Formula for Shedding 100 Pounds
Always swing your arms. The next rule is to employ high intensity interval training (HIIT).
The basic formula is to set the machine so that 30 seconds of walking is exceptionally difficult.

Shutterstock/ Ljupco Smokovski
At the end of 30 seconds, you change the settings to an easy pace, and walk this for two minutes. So it’s 30 seconds on, two minutes off.
Yes, you will repeatedly have to change the settings. Though treadmills come with “programs,” none fit the template that I’m describing here, even the ones that are called “interval” or “fat burn.”
The template is 30 seconds on, two minutes off. But the “off” is very easy.
If you feel fully recovered after only one minute, than your 30-second work interval wasn’t intense enough. How do you know it IS intense enough?
At the end of it, you’re nearly completely out of breath. You can’t talk. You need the full two minutes to recover and repeat the work interval.
The setting for the work interval will vary from person to person. A 25-year-old who wants to lose 100 pounds is, in general, fitter than a 50-year-old with the same goal.
On the other hand, that 50-year-old maybe does a lot of walking outside, even some hiking.
And maybe the 25-year-old doesn’t do any form of exercise and sits at a computer 10 hours a day. There are all sorts of variables.
So thus, there is no specific setting for the work interval. It’s whatever you cannot do longer than 30 seconds. And remember, there is NO holding on.
If you’ve been holding on for a long time, you’ll find that letting go makes you discover muscles you never thought you had.
You’ll need to get used to this before truly going all-out effort with the work intervals.
Example of a HIIT Session on a Treadmill
Warm up for 10 minutes with 30-second intervals of escalating effort and sub-two-minute recoveries.
After 10 minutes or so, you’re ready to begin the first hard work interval. It might be 4 mph at zero incline. It might be 0.8 mph at 15 percent incline.
Remember, you must NOT hold on. So if you’ve previously (while holding on) have been doing 15 percent incline at 2.5 mph, you will have to significantly slow the speed to be able to walk without holding on.
Remember the rule: The setting must enable you to walk, but be too difficult to exceed about 30 seconds.
After which, you reduce the settings so that you can catch your breath and recover for two minutes.
If you’re using a high incline, the reduction will require a zero incline or close to it.
If you’re already at zero or close to zero grade during your work interval, you’ll need to slow the speed quite a bit.
So if 4 mph at zero, one or two percent incline has you panting very heavily after 30 seconds, unable to talk, then slow the speed to 1.5 mph, maybe even one mph, for two minutes.
Then reset the machine to whatever the work interval was (e.g., 4 mph at one percent incline).
If it was 0.8 mph at 15 or 14 percent incline…then your recovery interval might be 1.5 mph at zero grade.
The point is to simply get the setting down to what comprises an easy, casual pace to recover with.
If you find you feel you can walk longer than 30 seconds at your work interval, guess what:
You must INCREASE the speed and/or incline. If you’re already at 15 percent, jump the speed up a bit and see how you do.
If after 12 seconds you must hold onto the treadmill…then you bumped up the speed too much.
If you’re using a zero or low incline, and feel after 30 seconds you can actually continue at that speed…but you can’t mechanically walk faster (due to your size or a knee condition), then increase the incline.
Yes, HIIT requires some experimenting with…at first. But once you become acquainted with it, you’ll know precisely what setting ranges get the job done.
Do eight cycles: eight work intervals and eight easy-pacing periods. Then warm down for 10 minutes with de-escalating work intervals.
When this treadmill plan is coupled with sensible eating habits (plant based diet with portion control), and done three times a week, you will lose 100 pounds. It will take a while.
After all, we’re talking a hundred pounds, not 20. To expedite progress, you must incorporate intense strength training.


Shutterstock/Reshetnikov_art

Shutterstock/Aleksey Boyko
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Can Thirst REALLY Be Mistaken for Hunger?

After reading this you’ll never again be convinced that thirst can be mistaken for hunger.
What a crock!
That thirst can be mistaken for hunger is absolutely one of the most ridiculous myths out there.
When I was a personal trainer at a health club, I made sure my clients knew that thirst is not the same as hunger, even though many women (and men) struggling to lose weight will fall victim to this myth.
Think about it: How can thirst be mistaken for hunger? These are two entirely different physical sensations.
It’s been said that a glass of water can often subdue a growling stomach.
Okay, how many of you, upon experiencing that empty feeling in your stomach, actually felt satiation after having a glass of water?
And if so, for how long did that satiation last? Did that water feel as though you just ate a sandwich?
After realizing that a large glass of water failed to induce satiation, did you spend the next 30 minutes trying to drink a few more glasses of water, trying to convince yourself that you were no longer hungry?
And if thirst can be mistaken for hunger, then what’s thirst supposed to feel like in the first place?
A thirsty animal will seek out water. A dog will drink out of a toilet bowl or dirty puddle outside to quench thirst and will not confuse this with the desire to eat a steak.
When a lion is thirsty it will drink out of a river, not try to kill a zebra. The cue for fluid intake is hardwired in all animals, including humans.
To say that this signal can be mistaken for hunger is to say that the hardwiring is seriously flawed.
After all, humans can survive a few weeks without food, but only several days without water. You’d better believe that this hardwiring is spot-on in the name of keeping us alive.
To those who still fall for the myth that thirst can be mistaken for hunger, ask yourself why this would be?
If a person is thirsty, why wouldn’t he or she simply feel thirsty? Are the wires in their brain crossed? This is almost like saying that feeling chilly can be misinterpreted for feeling roasting hot.
Hunger is not caused by a state of mind.
Don’t confuse the desire to eat with true hunger. The desire for food isn’t always driven by actual hunger.
Compulsive overeaters will eat well-past the point of satiation. Having a craving for cheese or lemon meringue pie doesn’t require hunger, either.
But when’s the last time your craving for cheese crackers, pie or chocolate chip cookies was suppressed by drinking water?
And if you’re actually hungry and know that Grandma’s home-baked bread is on the kitchen counter…try killing that drive with a glass of water.
An emotional craving for food cannot make a person mistake thirst for hunger. A situational urge to eat, such as being offered food or settling in front of a football game on TV, will not make you mistake thirst for hunger.
And of course, true hunger doesn’t mean you’re simply thirsty, even though you may be thirsty and hungry at the same time.
Cause of True Hunger Is Not Thirst
Hunger may be caused by low blood sugar or insufficient food intake. A strenuous exercise session may induce deep hunger afterwards.
The side effects of some medications can induce hunger.
Drinking a lot of water will make you feel bloated, but you can feel bloated and still feel hunger.
You can be hungry but not thirsty. You can be hungry and quite parched, drink a tall glass of water, and no longer feel parched, but still have a growling, empty feeling in your stomach.
If you’re hungry, you can try to talk yourself into believing that it’s just thirst, and drink your water or zero-calorie beverage.
But you won’t be fooled for long.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
How a Young, Fit Person Has a Heart Attack

Here is a careful explanation of how a young, fit athlete could drop from a heart attack.
Assume the athlete is not on any drugs or medications, and does not have a congenital heart defect.
Assume he or she is very physically fit and may be competitive, even elite, or just a passionate gym rat, mountain biker or runner.
They then suffer a heart attack. HOW?
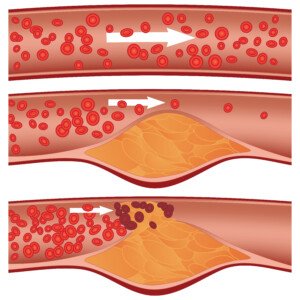
Dr. Cynthia Thaik, MD, says that “most acute coronary artery syndrome or events occur in arteries that have 30 percent plaque or less until the time of the coronary event.” Dr. Thaik is a cardiologist and author of “Your Vibrant Heart.”
In other words, these heart attacks occur in people whose coronary arteries are equal to or less than 30 percent clogged with plaque.
This is difficult to digest, because you’ve probably always associated heart attacks with completely blocked arteries or “very clogged” arteries that have only a tiny inside diameter for blood to flow through.
And these heavily clogged arteries, sludged up with plaque, are not what’s usually going on inside the hearts of younger, fit adults.
How a Heart Attack Happens in a Young, Fit Athlete
Dr. Thaik explains, “The mechanism is plaque instability and plaque rupture leading to platelet aggregation and acute thrombosis, such that the 30% stenosis progresses to 100% stenosis in a matter of minutes.”
Okay, let’s reword that in a language closer to English, according to Dr. Alvaro Waissbluth, MD, a cardiologist with Alameda Health System in CA.
“When a rupture occurs, your body tries to fix it by creating a plug,” begins Dr. Waissbluth, “just like if you cut your arm you will develop a clot and a scab.” This happens with a plaque rupture.
Shutterstock/Diamond_Images
“Most of the time the plug seals the tear and then the plaque is fixed and nothing happens,” continues Dr. Waissbluth.
“BUT if the plug grows and grows it can get very large and shut down the entire artery, and this is how a major heart attack happens.”
Recall that Dr. Thaik points out that this phenomenon occurs in seemingly fit, younger people who have a 30% or less blockage.
However, Dr. Waissbluth says, “Most heart attacks occur when a plaque blockage is in the 30-50% range and the outer layer of the plaque gets a small tear in it – a rupture.”
Well, this isn’t an issue of which is closer to the reality: under 30% or between 30 and 50%.
The issue is that these cardiac events occur via a mechanism “by which someone young and fit without any prior symptoms or knowledge of disease can suffer a massive heart attack and even suffer sudden death as their initial presentation,” explains Dr. Thaik.
“Athletes are particularly at risk if they are dehydrated during their physical activities.”
All of this may still not make much sense — until you realize that there are two kinds of plaques inside coronary arteries: soft (unstable) and hard (stable, calcified).
“The longer a plaque has existed and the bigger the plaque,” says Dr. Waissbluth, “the more stable its surface tends to be.”
Dr. Waissbluth goes on to point out that more major heart attacks result from blockages in the 30-50% range versus blockages filling up 80% of an artery.
So though not all cardiologists agree on the exact percentage range that’s the highest risk for plaque rupture, the common denominator is that newer plaques—those that have not been around that long in terms of cardiac time—are soft and can break apart (rupture).
Meanwhile, old plaque that has grown over time (80% blockage) is hard and not prone to breaking apart.
All of this contradicts the idea that exercising and preventing your arteries from clogging up is how to lower the risk of heart attack. However, you must step back and view the big picture.
In the grand scheme of things, people who don’t keep fit, who let their bodies turn to mush, who avoid working out, and especially those who smoke and develop diabetes, are asking for some very serious cardiac trouble down the road.
You can even have a heart attack without blocked arteries.
Keep working out. Keep running, biking, climbing, jumping and lifting. BUT…realize that what you eat is an enormous factor in whether or not you accumulate risky levels of soft plaque.
The fewer processed foods you eat, the healthier your heart will be.

Dr. Thaik’s clinical interests include congestive heart failure and women’s heart disease, and is affiliated with the American Heart Association.

Dr. Waissbluth has been in practice for 25+ years and is board certified in interventional cardiology and cardiovascular diseases. He is founder of Eat Tank, an educational nutrition initiative that provides simple tools and practical knowledge for better understanding food.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Oranges in the Nutribullet: Must You Add Water?

Here is why you do NOT need to add water when you grind oranges in the Nutribullet.
If you peel oranges (seedless) and load them in sections into your Nutribullet, you will not have to add water unless you want a thin consistency that’s similar to what you’d buy in a carton.
But outside of a texture preference, you’ll find that there is no need to add water to the oranges for the Nutribullet to pulverize.
Oranges contain enough natural juice and water that this is already built in.
Just make sure not to pack the sections too tightly, Just drop them in there and let them fill up to the line naturally.
I’ve never put an un-sectioned orange into the Nutribullet.
I cut the already-peeled fruit into quarters so that I can further scrape off the whitish thick stuff that’s between the rind and the fruit.
Scraping the fruit down to as “clean” as possible is not necessary, but right now, I’m not ready to include all that white stuff in my drink.
If you pull an orange apart, you’ll see that running down its center is a cord of this white stuff.
I just don’t like it in my juice. So with quarter sections, I’m able to cut it out more easily.
The end result is a juice that’s lighter in color than typical store-bought orange juice, kind of like a pale orange or an orange-whitish, and it has the consistency of a milkshake.
Your kids will love this and think they’re getting a treat or a reward.
They don’t have to know that it’s loaded with fiber, pulp and natural enzymes.
In store-bought juice, whether it’s in a carton, bottle or frozen in a can, the product is pasteurized before it gets packaged.
Pasteurization kills enzymes—and enzymes are very health-giving.
Among their benefits is that of aiding the digestive process and de-stressing the GI tract.
So in summary, no water is necessary for “juicing” oranges in your Nutribullet.
I just recommend that you chill the peeled sections in the freezer for 20-30 minutes before pulverizing them, as this will give the finished product the same kind of inviting chill that a milkshake has.
Extra Spike of Nutrition
For an added burst of nutrients, add beets to the oranges in your Nutribullet.
Beets provide essential vitamins, minerals and antioxidants, complementing the vitamin C and natural sugars of oranges.
This combination enhances the nutritional value of your smoothie, supporting overall health and providing a vibrant, flavorful drink with a super dazzling color.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, Racool_studio
Lifting Heavy Weights with High Blood Pressure for Mass Building

High blood pressure doesn’t mean that you can’t lift weights for building mass. I cite a fascinating study out of McMaster University.
This study showed that lifting lighter weights to muscle failure is sufficient to build mass – however, this article will describe to you how to maximize this process. “Lift lighter weights to failure” is rather ambiguous.
First of all, “Rather than grunting and straining to lift heavy weights, you can grab something much lighter, but you have to lift it until you can’t lift it anymore,” says associate professor of kinesiology at MU, Stuart Phillips.
“Muscle failure” is exactly that: You cannot lift the weight anymore. The limitation isn’t the perception that the weight has become too heavy to mechanically handle.
The limitation is the intense “burning” in your muscles, the “pain” or “hurting” in the muscles. This can occur even with very light weight.
To maximize the light weight protocol, I, as a former personal trainer for a health club, strongly recommend drop sets with relatively short rests in between.
The muscle burn will be significant after several cycles of drop sets. As for what constitutes “light” or “lighter” weights, this depends on the person doing the lifting.
One person’s “light” weight is another person’s heavy weight for lifting.
Here is an example of the protocol, using the shoulder press machine in which you insert a pin into a stack of weights.
This concept, however, can be applied to any lifting venue, such as pulleys, dumbbells and compound moves with barbells.
Find the load that is heavy enough to challenge you for eight reps, but that is not — I repeat — is not an 8-rep max.
An 8-rep max requires straining, which one with high blood pressure will not want to do.
So find the load that challenges you at eight reps, yet makes you feel that you can do several more reps, even five more reps. But stop at eight. This will avoid a spike in blood pressure.
Immediately lower the load by one plate worth (which on some machines is 10 pounds; other machines it’s 15 pounds). Then quickly resume lifting.
By quickly resuming, you are keeping the muscles activated and firing, yet you are also avoiding the straining zone, since the resistance is now lowered by 10-15 pounds.
Because this load is much lighter, you may be able to achieve muscle failure without straining and spiking blood pressure.
This depends on the routine, but the more it isolates muscles (as opposed to routines like deadlifts or free barbell squats), the easier it is to achieve muscle failure without straining and significantly raising blood pressure.
In other words, you will most likely reach a point where you cannot do another repetition, even though you are not straining, grunting or breaking form.
When you cannot lift any more, repeat the drop set with the next lightest weight increment.
Go to failure. At such a light weight, again, this should be achievable (an intense, nasty burn), well-before you reach the straining/grunting zone – avoiding a big raise in blood pressure.
Now, at this point, you can stop for a rest; or, you can do yet another drop set. So it may be a three- or four-drop-set routine.
The higher the weight that you start out with, the more descending sets that you can do, which means a greater potential for taxing muscle fibers without significantly raising blood pressure.
Take only 60 seconds in between cycles and do six cycles. The burning in your muscles will be significant, and you will walk away from this regimen feeling worked over.
Another tip for avoiding spikes in blood pressure, while performing this regimen, is to lift the weights fairly fast, but complete the range of motion for each repetition. Slower movements will raise blood pressure more.
“We’re convinced that growing muscle means stimulating your muscle to make new muscle proteins, a process in the body that over time accumulates into bigger muscles,” states Phillips.
This is doable with the regimen just described, while preserving reasonable blood pressure readings.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2010/08/100811125943.htm
Can Lumbar Scoliosis Be Corrected Without Surgery?
Do you really need surgery to correct lumbar scoliosis? Could there be a conservative way to deal with this problem?
“Research is inconclusive on whether nonsurgical care truly corrects [lumbar] scoliosis by reducing the curvature of the spine,” begins Dr. Jeff Langmaid, DC, Founder/owner of The Evidence Based Chiropractor, LLC, in Tampa, FLA, a research-based marketing and practice growth company that serves thousands of chiropractors across the world.
“However, many patients have received significant symptomatic relief from scoliosis through nonsurgical and conservative measures,” continues Dr. Langmaid.
“The primary conservative care options are physical therapy and/or chiropractic care.”
When might surgery be necessary for scoliosis including lumbar?
“The conversation for surgical intervention typically starts when the patient’s spine has a curvature of 45 to 50 degrees,” explains Dr. Langmaid.
“A vast majority of patients fall under the 45-degree threshold and can benefit from conservative care.
“Nonsurgical, conservative care may not always straighten the spine, but it often provides significant relief and functional improvement for patients with scoliosis.”
Keep in mind that a person may have scoliosis but also be asymptomatic—and thus not needing any treatment.
“Because of this, surgeons will typically wait until conservative care is exhausted before surgical intervention is discussed.”
Treatment and Management of Scoliosis Including Lumbar without Surgery
Dr. Langmaid explains, “Physical therapists will primarily work with a patient for strengthening and stretching muscles that support the spine.
“Strengthening and stretching the muscles around the spine may help reduce pain and prevent functional loss associated with scoliosis.
“Physical therapists may also use passive modalities, such as electric stimulation, heat or ice to reduce pain and inflammation around the unwanted curve.”
Chiropractic Medicine
“Chiropractors typically focus on the segmental motion of each vertebra,” says Dr. Langmaid.
“Patients often receive relief from the challenges of scoliosis with improved range of motion. Chiropractors may also choose to use passive modalities and/or strengthening or stretching to support their care.”
Causes of Scoliosis
The most common form of scoliosis has no known cause, but it does tend to run in families.
Less common forms may be caused by a neuromuscular condition such as cerebral palsy (which can be present at birth or acquired due to head trauma later in childhood).
An injury or infection to the spine is another possible cause of scoliosis.
 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Lucien Monfils
URINE: Cancer Fear over Colors, Odor, Burning

Here’s complete information about urine colors, smell, burning when you “go” and other excrement-related issues for cancer-phobes.
If you can’t get through the day without urinating into a plastic cup to inspect your excrement, even going as far as putting a color chart up against the fluid, then the articles below are for you.
However, even if you’re health conscious at a tamer level, you will learn a lot by reading these articles about all sorts of issues relating to urine.
CANCER
– Blood in urine can come from other conditions, not just cancer
– Causes of cloudy urine, how to examine your pee
COLOR
– Why your urine is the color of a blood orange

Orange, Freepik.com, rawpixel.com
– “Is my urine orange or just a dark yellow? How can I tell?”
– Over 12 causes of urine that’s the color of tea or cola
ODOR
– Does your urine suddenly smell really bad?
– Does your urine smell like rotten fish?
MISC
– Having to pee a lot can be caused by anxiety, but how?
– Why jogging can make you feel like you have to “go”
– Is your urine looking foamy lately? This needs attention.
What is pee made of anyways?
Urine is mostly water, about 95%, actually. This is surprising, yes, being that it can smell really bad at times.
The purpose of pee is to expel waste.
That remaining 5% contains urea, a byproduct of protein metabolism.
In addition there are salts, electrolytes and small amounts of creatinine, ammonia and other waste compounds.
It may also contain trace hormones, vitamins and medications the body is eliminating.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/omicsonline
Will Vet Treat Injured Cat if Owner Cannot Pay Bill?

If you’re reluctant to bring an injured cat in for emergency treatment because you can’t pay the bill, here’s encouraging information from a veterinarian.
It’s one thing when a cat gets sick (ongoing diarrhea, starts limping, fur is falling out) and you’re broke and thus, don’t take your pet in to see the vet.
After all, you hope that the symptoms will go away on their own.
But what if your cat suddenly gets injured?
You’re thinking that if you bring it in for emergency treatment, you won’t be able to pay the bill.
Hold on – this situation is not as dismal as you might be thinking.
You “should know that in case of severe trauma, most states require a veterinarian to provide basic first aid, whether or not they are paid,” explains Jean Hofve, DVM, who has 20+ years’ experience in both conventional and alternative veterinary medicine, and author of the eBook, “What Cats Should Eat.”
Dr. Hofve further explains, “This is important, for example, if you see an animal that isn’t yours get injured; for instance, hit by a car.
“But if you authorize any further treatment beyond immediate stabilization, you will be expected to pay for it.”
So if your cat is hit by a car and suffers a broken leg, take it in for emergency treatment including X-rays and setting the leg — and you won’t have to pay for it.
The cat is stabilized once the broken bone is set, and at that point, any additional medical care (such as an infection a few days later) will be charged to you.
Same with surgery for organ damage sustained in a vehicular accident.
Or if your cat is gashed by a dog, again, you will not have to pay the bill for basic wound clean-up, stitching and bandaging.
The cat is stabilized at this point and you can take it home. Follow-up care, however, will be on your tab.
 Now retired from veterinary medicine, Dr. Hofve has researched pet nutrition and the pet food industry since the early 1990s. She has written dozens of articles and has been interviewed for print, radio and television around the world. She is author of the eBook, “What Cats Should Eat.”
Now retired from veterinary medicine, Dr. Hofve has researched pet nutrition and the pet food industry since the early 1990s. She has written dozens of articles and has been interviewed for print, radio and television around the world. She is author of the eBook, “What Cats Should Eat.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/New Africa
Kitten’s Swollen, Irritated Anus: Causes & Solutions
A vet explains why your kitten’s anus is swollen and irritated: MANY possible causes.
This could be due to quite a few possible causes that then indirectly lead to anal irritation and swelling.
The most likely cause is “scooting.” This is when a cat (or kitten) drags its behind along the floor or ground.
Of course, the anus will become irritated and swollen because of the repeated contact.
But the big question is: Why is your kitten scooting in the first place?
“Excessive scooting for any reason will cause swelling and redness,” says Jean Hofve, DVM, who has 20+ years’ experience in both conventional and alternative veterinary medicine, and author of the eBook, “What Cats Should Eat.”
Dr. Hofve says that scooting in a kitten may be caused by the following conditions (no particular order):
– Anal sac inflammation, infection or impaction
– Pyoderma (bacterial skin infection)
– Yeast infection
– Urinary tract infection
– Ringworm (a fungal skin infection)
– Tapeworms/coccidian/pinworms/other intestinal parasites
– Changes in gut flora (may occur after antibiotic treatment)
– Urethritis/vaginitis
– Proctitis (inflammation of the anus/rectum)
– Diarrhea or constipation
– Vaginal hairball/foreign body
– Low back pain
– Displacement behavior (cat continues scooting after the primary cause is resolved)
There are additional causes of scooting — which then could cause the anus to become swollen and irritated — but these additional causes are not as likely to occur in a kitten, but rather, a cat:
– Fleabite allergy
– Food allergy
– Atopy (inhalant allergy)
– Environmental allergy
– Inflammatory bowel disease
– Obesity
And One More Possible Reason for a Kitten’s Swollen, Irritated Anus
Dr. Hofve says that an additional cause could be “rectal prolapse and irritation from suckling by littermates (more common than you would think!). Depends to a large extent on age of kitten.”
 Now retired from veterinary medicine, Dr. Hofve has researched pet nutrition and the pet food industry since the early 1990s. She has written dozens of articles and has been interviewed for print, radio and television around the world. She is author of the eBook, “What Cats Should Eat.”
Now retired from veterinary medicine, Dr. Hofve has researched pet nutrition and the pet food industry since the early 1990s. She has written dozens of articles and has been interviewed for print, radio and television around the world. She is author of the eBook, “What Cats Should Eat.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Will Yogurt Make Your Cat Sick?
Will yogurt make your cat sick? Will yogurt — considered healthy for people — cause your cat to vomit?
Many people will give their cat milk without a second thought, and milk is a dairy product as much as yogurt is.
So it’s always interesting when people wonder if yogurt can harm their cat.
The answer to the question?
“No. Too many carbohydrates, and not enough probiotics to make a difference,” says Jean Hofve, DVM, who has 20+ years’ experience in both conventional and alternative veterinary medicine, and author of the eBook, “What Cats Should Eat.”
Dr. Hofve continues, “If your cat needs probiotics, use a good quality human probiotic supplement.”
These can be found in the supplement section of a conventional grocery store, as well as in a health food store.
They can also be ordered online.
To get your cat to consume the supplement, you can opt for chewable flavored tablets or mix the supplement in your cat’s food.
If your cat loves yogurt, however, there is no harm in feeding your pet unsweetened plain. Your pet does not need the added sugars.
An alternative is to mix the yogurt with the milk that you normally give to your cat.
You may also want to consider kefir, which is a dairy product that can accurately be described as a cross between yogurt and milk.
It’s thick like a shake. Pour this into your cat’s bowl and see what happens.
Make sure you give your pet unsweetened plain rather than fruit flavored.














































