Moles & Melanoma Guide to Changes, Colors, Size & More

Every question you can have about moles and melanoma is answered right here, because I was fed up with years of seeing the same generic and vague information about moles and melanoma.
My questions were directed to Jason R. Lupton, MD, board certified dermatologist practicing in the San Diego, CA area.
A mole that is melanoma can sometimes itch.
Can it itch and still look the same as it always has? Or will an itching cancerous mole always look like it’s changing?
Dr. Lupton: A mole that itches may not always look like it’s changing.
Is mole itching from melanoma subtle and/or really annoying? Is it necessarily every day?
Itching associated with a melanoma can vary — it will not necessarily itch all the time. It may be subtle itching or may be quite pronounced.
It’s said that a risk factor for melanoma is a mole that stands out or looks different from others.

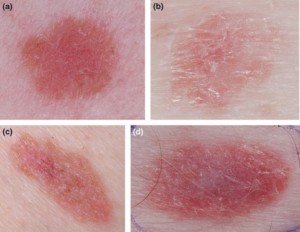
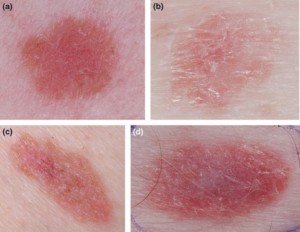
Atypical moles. Shutterstock/Mikel Ugarte Gil
But what if it has always been this way? Does the relative “differentness” in and of itself mean the mole is more likely to become malignant?
If a mole looks very different from others then I usually biopsy that one.
If a patient comes in for a skin check and one mole looks very different or atypical than the others, then often I will biopsy that mole to see how it looks microscopically.
A different-appearing mole may not necessarily be a bad mole — but it should be evaluated.
What makes a mole look “different” is the comparison of it to others.
Suppose a mole on someone’s calf looks different than all his others, but the calf mole has always looked the same.
What would be the significance if, in a parallel universe, this same person had only one mole on his entire body, on the calf, and thus, the concept of this mole looking different from others wouldn’t be applicable?
Often people have the same types of moles. That is, some people have many moles that have some redness to them, or that are all very dark, or that are brown and black, etc.
When doing a skin exam it is important to assess the types of moles someone has and what differences, if any, there are among them.
It is all done on a case by case basis – unfortunately, there are no rules to follow regarding this. If a mole looks different than the others then it may need a biopsy.
It all depends on whether that mole just looks different or if it also looks irregular or atypical — meaning irregular colors, border, size, recent changes, etc.

Is a certain type of mole more likely to become melanoma, other than ones bigger than 5 millimeters?
That is, dark moles, light moles, raised moles, oblong moles, ones with a hair, two-toned moles?
No — not really. Any mole can become a melanoma. Larger moles may have an increased risk — especially very large lesions.
Other than that, any spot on the skin can become cancerous — whether it is dark or light.
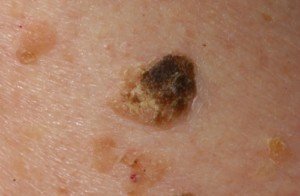
There is a type of melanoma — the amelanotic melanoma — that is particularly scary because it does not have the classic dark, changing colors most people associate with a “bad” mole.
amelanotic melanoma
These can look like pink or light red or even flesh colored skin lesions — often patients are not worried or concerned about these.
We always read about changes to look for in moles.
But most melanoma occurs absent moles, so what else should we look for on skin in general, that might mean the deadliest skin cancer?
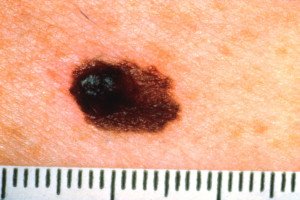
Over the past 25 years, the same handful of melanoma photos have appeared in magazines, pamphlets and the Internet.
They appear to have sprung from pre-existing moles, rather than just plain skin.
Any new lesion should be evaluated. A melanoma may arise anywhere on the skin — even the palms or soles of the feet or in the groin area. Any new lesion that is changing in any way should be evaluated by a dermatologist.
A melanoma will not remain static — it will continue to change and grow over time.
Why does melanoma get past so many people? 1) They don’t see it due to its location, 2) They see it changing but are in denial? Or 3) They don’t know about the warning signs of skin cancer despite all the media attention, and, though they are aware of the changing lesion, don’t think anything of it.
I think all three! Many people are not in tune with their moles and do not get regular screening exams.

Shutterstock/Image Point Fr
Also, if someone sees something changing they often have an alternate explanation for it — there is sometimes that element of denial — that a melanoma cannot happen to them.
Does a melanoma in a pre-existing mole always look suspicious? I realize that the first day the mole becomes melanoma, there is no way the naked eye could detect this.
But for how long can a mole have this deadly cancer before a person can see something suspicious?
This is unknown — some are more aggressive than others. A lesion may progress to a cancerous lesion and not be detectable for months or longer. It is really unknown.
If a mole changes colors from melanoma, will it necessarily also be getting bigger simultaneously, or changing in some other way concurrently?
Or if it gets bigger from melanoma, will it also necessarily be changing color?
A melanoma will often have changes — color and size. The initial changes may be subtle, so only one may be noticed at first, but if left over time, then a change in size is almost always seen.
How often can melanoma arise out of a very tiny mole, i.e., a birthmark?
After all, every skin cancer warning list mentions moles the size of a pencil eraser as being possible signs of melanoma.
The rules regarding melanoma are certainly not absolutes. A melanoma can be very small — not always bigger than a pencil eraser (as an aside I just discovered a melanoma on one of my patients last week — on her arm … it was only about 3 mm in diameter but was half brown and half red, so I biopsied it and it turned out to be a melanoma).
I think the important thing here is the guidelines are helpful, but you can’t be too tied to them.
If a lesion looks suspicious it should be biopsied — and everyone should have a yearly skin exam by a dermatologist to be safe.
Suppose a person magically knows that soon, he’ll develop a melanoma on a non-mole area of skin. He watches that area every day.
At some point, a malignant spot will become visible, when the day prior, it was not detectable.
So if this person watches his skin every day in that exact spot, how big will the melanoma be when he first sees it?
That is, could a malignant spot appear over night that’s 2 millimeters?
Or how big would it be from one non-detectable day to the next detectable day?
This is unknown — but my guess would be it would be a very small spot at first and then develop a more prominent lesion over time depending upon how long it’s left.
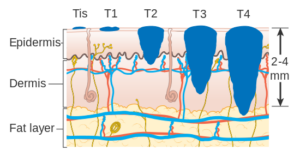
Stages of melanoma. Cancer Research UK
Can melanoma change visibly from month to month?
Week to week? What is the fastest a mole can change visibly to the naked eye?
In other words, suppose a person suspects skin cancer and thus watched the spot carefully.
If after two months, it looks the same, can the person assume it can’t be malignant? How about one month?
Good question. I usually tell my patients to watch their moles about every three months or so — to take an all-over look then … if you look too often you won’t notice subtle changes, but if you wait too long you may miss something.
There is no ideal rule — a melanoma can develop at any time and if something CONTINUES to change then it should be looked at by a dermatologist.
It also depends upon the type of lesion, the age of the patient, the body location, etc. So I can’t give an absolute on this one.
What skin conditions can really look like melanoma?
Birthmarks, normal moles, seborrheic keratoses, pyogenic granulomas, vascular lesions, dermatofibromas, dysplastic nevi (atypical moles), etc.
Seborrheic keratosis
It’s said that if caught early, 95 percent, 97 percent, or “near 100 percent” of melanoma can be cured.
Why not 100 percent? What happens in those 5 percent of patients that they die despite an early catch?
The early catch may not really be early — there may be micro-metastases or microscopic lymph node involvement that cannot be detected by current technologies.
It makes absolutely no sense that the human body didn’t evolve to have a stronger defense against the sun’s damaging rays.
Early man, including pale-skinned ancient Europeans, spent tremendous amounts of time in the sun.
It only makes sense that we all should have a built-in guard against skin cancer.
So why all the skin cancer in modern man, who spends less time in the sun than ancient man? Even modern-day sunbathers aren’t in the sun as much as primitive man.
I think it also has a lot to do with the depletion in the ozone layer, and with modern man there is limited sun exposure at times coupled with more intense periods … these episodic sun exposures may be associated with increased risks of skin cancer development.
 Dr. Lupton specializes in skin cancer prevention and treatment plus minimally invasive cosmetic procedures including mole removal, skin rejuvenation, wrinkle reduction and acne treatment.
Dr. Lupton specializes in skin cancer prevention and treatment plus minimally invasive cosmetic procedures including mole removal, skin rejuvenation, wrinkle reduction and acne treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Pimples on Bald Head: Causes and Solutions

Pimples on your bald head driving you nuts?
There are several ways to prevent or get rid of annoying, unsightly pimples or blemishes, or what appear to be pimples, that have appeared on your bald head.
First of all, let’s get a dermatologist’s take on this common problem with men who are proud to be bald.
What is the most likely cause of pimples developing on a bald head?
This is “most likely to occur with men who shave their beards and head,” says Dr. Oanh Lauring, MD, founder of Lauring Dermatology in Nottingham, MD
“Normal skin bacteria gets into the nicked skin and inflames the hair follicles and promotes folliculitis.”
Solutions
Dr. Lauring advises not to shave against the grain of the hairs.
As for a solution to pimples or red bumps on the bald head, Dr. Lauring states, “Start out with over-the-counter benzoyl peroxide wash or salicylic acid wash; topical benzoyl peroxide to prevent flares, but some people may require topical antibiotics or steroids for flares of the bumps.
“Avoid using cocoa butter, Vaseline petroleum jelly to the scalp, as it may clog pores and promote folliculitis.”
Here are other solutions to pimples, blemish-like spots, or red bumps on your bald head, endorsed by members of the community for bald men, slybaldguys.com:
– Use a single blade to prevent razor burn. This is commonly done by bodybuilders to prepare for contests.
– Pimples can be caused by blocked pores, but pimple-like bumps, which aren’t technically pimples, can arise from shaving, so be alert to your shaving techniques.
So do not use any products on your head that can clog pores.
If you feel that the red “bumps” on your bald head are related to pores, rather than to shaving, apply an astringent or product that contains salicylic acid.
This might sting momentarily, but can diminish red areas, and in some men, can completely clear up trouble spots in a few days.
– Try exfoliation. You can exfoliate by gently (or more vigorously, according to some men) rubbing the exfoliation sponge along the irritated area. One man recommends the St. Ives apricot scrub.
Another man simply uses a brush; this can be either a facial or body brush.
Any store that sells bath products should have these. Natural bristles will probably work better than plastic ones, and are a bit softer to the touch.
– Ingrown hairs can cause “shaving bumps.” One man recommends Shave Secret, available at Walmart.
Another bald man reports that he tried just about everything for the pimples that kept appearing on his head; nothing worked.
Then he tried a 1 percent hydrocortisone cream and a 10 percent benzoyl peroxide product, and this worked.
Dr. Lauring explains, “African-American men are prone to ingrown hairs and subsequently unsightly scar bumps.
“People should avoid plucking or waxing, as this traumatizes the hair bulb and encourages the hairs to grow back into the skin.
“If an ingrown hair develops, it is best to use a needle to carefully loosen the hair from the skin, then clip the hair.
“When bumps occur and persist, they may require topical steroids or even steroid injections to stop the inflammation.”
Dr. Lauring adds, “Ointments absorb better than creams, but they tend to be more clogging to the pore if they are petrolatum-based.
“Topical steroids should always be used sparingly and for brief periods, as daily chronic use of topical steroids may promote more acne, folliculitis, skin thinning, skin lightening and stretch mark development.”
Sporting a bald head by choice isn’t as easy as it looks or seems.
The bald head requires continuous upkeep and is thus vulnerable to irritations such as pimples and other red bumps.
 Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/ArtOfPhotos
Source: slybaldguys.com/smf/index.php?topic=10847.0
What Those Tiny Red Dots on Your Skin Might Mean

Have you noticed red dots suddenly appearing on your skin?
Or maybe a single red dot, and you wonder how long it’s been there on your skin?
Could melanoma skin cancer first appear as a red dot, or is a red little spot on the skin usually harmless?
I have the answers, because I asked these questions to Dr. Oanh Lauring, MD, founder of Lauring Dermatology in Nottingham, MD.
Many people notice “dots” on their skin, and these skin dots or spots appear to be red.
This article is about red dots or spots (which may be elevated) on the skin, rather than red bumps or blemish-like spots.
“Red dots” on the skin can appear in many different ways.
One way is the appearance of pinpoint size specks. Let’s talk about these first.
The closer you examine your skin, the more of these tiny specks you may discover.
Some can be a little larger, like the size that a ball point pen would make, and then even larger yet, like 1-2 millimeters, even up to three mm.

A cherry angioma. Shutterstock/dba87
Upon close inspection, you realize that these “red dots” aren’t necessarily dot shaped, but can be erratically shaped, as small as they are.
They may also appear a dark red, a bit off-red or a dark pink.
Some people have loads of these all over their body (particularly the back and chest).
These are called cherry angiomas and are completely harmless (see the two images above of harmless angiomas, also known as hemangiomas).
They are blood vessels above the surface of the skin, come with age (though there’s an isolated version that’s present since birth and may be quite large), and will never become a problem.

More angiomas. Shutterstock/Timonina
Other causes of red dots or spots on the skin, says Dr. Lauring:
“Pinpoint red dots: causes include leukocyclastic vasculitis (usually benign inflammation of the capillaries that can be associated with infections, medications, autoimmune processes), Schamberg’s disease (benign disorder presenting as cayenne pepper like red dots on the lower legs of older people), extravasation of blood into the skin caused by scratching and damaging the capillaries.
Bigger red or swollen dots around the ankles: may be bug bite reactions (mosquitoes, bed bugs, scabies, chiggers).”
Extravasation
It’s easy to cause this without knowing it. If you notice a new reddish dot, spot or speck under your eyes, under your brows or near the bridge of your nose, don’t fear skin cancer.
This is most likely an extravasation caused by scratching there, or even by simply pressing a nail there to relieve an itch.
One little nail press is all it may take to damage tiny capillaries. This is harmless.
Extravasation is “leakage of red blood cells from after there is trauma to the blood vessel wall,” says Dr. Lauring.
This is what happens when a person plays volleyball for the first time or after a long absence, allowing the ball to smack repeatedly against the bare underside of their forearms.
Multitudes of red dots will appear later on.
Extravasation spots disappear in several days, often taking on an orange tinge as they fade.
You should get acquainted with what cherry angiomas look like, versus extravasation spots.
Both can be described as “little red dots on the skin,” yet both look completely different from each other.
Another cause is atopic dermatitis. Psoriasis, too, can create little red dots or spots on the skin.
Melanoma
Melanoma skin cancer can present as a tiny red dot.
Images of melanoma on the Web usually show brown, purplish and black blotches.
But melanoma can present as a small red spot on the skin.
Below are three images of what this can look like.

Melanoma. Cancertherapyadviso.com

Melanoma. Nejm.org

Melanoma. Nhs.uk
A man I know was diagnosed with melanoma at age 27. He showed me two melanoma spots near his wrist: two tiny red dots.
However, do not let this be reason to panic if you discover red dots on your skin.

A small eczema patch
The bottom line: If a “red dot” does not go away, then consult with a dermatologist to make sure it’s nothing concerning.
Angiomas will not disappear, but it’s important to know how to recognize these.
 Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
Dr. Lauring is former chief of dermatology at Mercy Medical Center. Lauring Dermatology provides medical and cosmetic services including for skin cancer, acne, psoriasis, hair and nail problems, and skin rejuvenation.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Top image: Shutterstock/Ocskay Bence
Rough Red Patch on Nose or Cheek: What This Might Be
Concerned or worried about that rough red patch on your nose or cheek?
Perhaps you also have some scaly reddish or pink patches on your forehead, maybe between your eyebrows or even beneath your eyebrows.
Do the rough, red areas on your nose or cheeks come and go?
Or do they persist?
Here’s a better question:
What are the chances that the rough, red patch on your cheek or nose could be skin cancer?
If you have rough red areas on your cheeks or nose, it’s smart to keep an eye on them.
This is because based on the generic description of “rough, reddish patch” or “dry, scaly pink or red area” on the nose or cheek, this can actually describe a type of skin cancer called squamous cell carcinoma.

Squamous cell carcinoma. Shutterstock/Dermatology11
But don’t panic – because this description can also very well fit a few benign skin conditions.
There are two benign skin conditions that classically present as rough and red patches:
Seborrheic dermatitis (top-most image)
Actinic keratosis
“Seborrheic dermatitis is a rash on the face that is pink with scale,” says Dr. Monica Halem, MD, a dermatologic surgeon who specializes in skin cancer surgery, laser and cosmetic surgery.
“This is usually present on the laugh lines, and between the eyebrows. It is usually present on both sides of the face.”
I have seborrheic dermatitis, and I can easily understand how the layman can mistake this as skin cancer.
After all, many descriptions of skin cancer are similar to that of seborrheic dermatitis:
“Rough, red patch on the nose or cheek.”
Or, “Rough, scaly dry red or pink patch on the skin.”
This is a generic description of how non-melanoma skin cancer can present, but it also fits the description of seborrheic dermatitis.
A more detailed description of seborrheic dermatitis is as follows:
Often accompanied by flaking, especially on the nose
May have a very subtle orange tinge to the “red” or pink color
May crust where the nose meets the top of the “laugh line” area
May itch and slightly sting.
Another hallmark sign of seborrheic dermatitis is that it comes and goes. It can appear virtually overnight.
Seborrheic dermatitis can never morph into skin cancer.
Actinic keratosis can also be described, generically, as rough red or pink patches or areas on the skin, particularly the nose and cheeks. It’s also called solar keratosis or “sun damage.”

Actinic keratosis. Shutterstock/Dermatology11
Dr. Halem says, “Actinic keratosis is usually much redder with thinner scale, and is in sun-exposed areas: top of the nose, sides of the cheeks, and forehead.”
For all practical purposes, actinic keratosis will NOT go away once it develops, even though medical literature cites that in rare instances, it can spontaneously disappear.
Actinic keratosis is when the keratocyte cells of the epidermis morph from typical to atypical.
The result is the classic rough, reddish patches that you one day discover on your nose, cheek or other part of the face.
Sometimes, the actinic keratosis can’t really be seen, but it can be felt; it has a distinct roughness to the fingers, kind of like sandpaper.
Dermatologists typically make a visible diagnosis that includes feeling the rough, red patches of skin with their fingertips.
If you’ve been diagnosed with actinic keratosis, don’t be alarmed, because your dermatologist will give you the other name that this skin condition commonly goes by: precancerous lesion.
Hearing this will trip a lot of people up, because their next thought will be, “Oh God, I’m gonna get skin cancer!”
However, the reason actinic keratosis is called a precancerous lesion is because its atypical cells are more likely to ever become cancerous, than are the typical cells right next door to the rough, reddish patch. That’s all that precancerous means.
Precancerous lesion does NOT mean predestined to become cancer.
It simply identifies that an atypical cell, more than a typical cell, is more likely to ever become malignant.
If actinic keratosis is left untreated, there is a 5-10 percent chance that it will morph into squamous cell carcinoma.

Squamous cell carcinoma. Shutterstock/Dermatology11
“Nobody really knows the time span for an AK to turn into an SCC,” says Dr. Halem.
“It can take anywhere from 2-10 years. It really depends on how much sun exposure you have had.
“More importantly to know is that 2 percent of all AK’s will turn into an SCC and there is no way of knowing which ones will do this.”
SCC skin cancer can metastasize, and kills about 3,500 to 10,000 Americans yearly.
However, in order for actinic keratosis to turn into the skin cancer, it must be left untreated.
And, believe it or not, there are people who ignore those rough, red patches or lesions on their face, chalking them up to age, harmless sun damage, stress, or who knows what.
Another reason that an actinic keratosis can go untreated is that a person can easily not even know they have these very gradually developing, red, rough patches on their skin — the skin on the top of their bald head, for instance.
This is a common site for actinic keratosis: A man’s bald head gets a lot of sun.
Finally, with 46 million Americans with no medical insurance, it’s easy to see why a person would not go to a doctor to have painless, rough red patches on their face checked out.
Actinic keratosis is very easily treated (removed) with a gentle spraying of liquid nitrogen; or the application of prescription creams.

Actinic keratosis on the cheek after a daily application of the topical cream Efudex for two weeks. The drug causes an inflammatory response that reddens the lesion before causing it to fall off. ©Lorra Garrick
Get it treated and keep an eye on your skin for the development of any new rough, red patches, and you won’t have to worry about squamous cell carcinoma.
 Dr. Halem, Founder and Medical Director of The New York Dermatologic Surgery Cosmetic Laser Center, has devoted a decade to clinical research, conducting trials that have advanced cosmetic and surgical dermatology.
Dr. Halem, Founder and Medical Director of The New York Dermatologic Surgery Cosmetic Laser Center, has devoted a decade to clinical research, conducting trials that have advanced cosmetic and surgical dermatology.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Top image: Shutterstock/sruilk
My Teen Has Tons of Moles: Should I Worry?
![]()
Skin cancer surgeon Dr. Monica Halem comments about teens with many moles.
Have you looked at your teen’s skin lately for moles? Are you even aware of how many moles your teen has?
My nephew at 14 had quite a few pigment spots all over his back, and some on his neck and arms.
He’s older now but they’re still there: not pinpoint moles, either. Many are almost pencil eraser diameter.
His parents were never concerned their teen had a lot of moles, and having many is a significant risk factor for deadly melanoma skin cancer.
But if your teen has a lot of moles, what could you possibly do?
After all, it’s not advisable to have the spots removed as a “just in case” measure.
But there IS something that parents can do if their teens have a ton of moles: Educate them about the dangers of excessive sun exposure. This can’t be said enough.
And the education should come early in life, long before kids hit their teen years, though in early life, they will most likely not have so many moles — most develop after birth and before age 20.
Waiting until a child is a sun-worshipping teen to educate about healthy skin is not a smart move. When my bronzed nephew was 14, I noticed his back while we were on a boat.
As a teen he’d spent every summer doing lake activities such as tubing, water skiing, wakeboarding and jet-skiing.
Furthermore, he spent a lot of time on the boat: a lot of sun exposure.
He also golfed: more sun galore. He obviously never wore much sunscreen, as he was very tanned whenever I saw him.
On the boat when he was 14, I got a close-up of all this teen boy’s back moles. I concluded that his well-meaning (and very tanned) parents didn’t feel concerned.
Though melanoma is extremely rare among teens, it is on the rise among teens.
Melanoma
Furthermore, the melanoma that a person gets in his 40s, 50s or 60s, might very well be the result of lots of sun tanning during the teen years!
It can take decades for melanoma to develop. The “seeds” for melanoma can be planted during childhood and teen sun exposure.
“Any teen who spends time in the sun is at risk for developing skin cancer, especially melanoma,” says Dr. Monica Halem, MD, a dermatologic surgeon who specializes in skin cancer surgery, laser and cosmetic surgery.
My nephew’s mother had always been on top of getting her son checkups during his teen years for his acne.
But she was out of the loop regarding all the sun that his many moles had gotten year after year.
Dr. Halem continues: “Teens with an increased number of moles are particularly susceptible. The presence of moles is alone an increased risk factor for skin cancer.
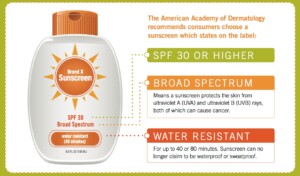
“To add sun exposure on top of that makes things worse. Anyone with several moles should get a yearly exam by a dermatologist and should wear sunscreen daily with an SPF of 30 or higher.”
 Dr. Halem, Founder and Medical Director of The New York Dermatologic Surgery Cosmetic Laser Center, has devoted a decade to clinical research, conducting trials that have advanced cosmetic and surgical dermatology.
Dr. Halem, Founder and Medical Director of The New York Dermatologic Surgery Cosmetic Laser Center, has devoted a decade to clinical research, conducting trials that have advanced cosmetic and surgical dermatology.
 Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and cybersecurity topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pixel-Shot
Red Dots on Skin: 19 Causes, Some Serious

Basal cell carcinoma. Source: cancer.gov
Red dots on the skin usually don’t mean cancer – usually.
But you should get acquainted with your skin and what is normal for it versus not normal, so that if you start seeing reddish dots, you’ll know whether to immediately see a doctor, or just relax and not worry.
Joshua L. Fox, MD, F.A.A.D., Director and Founding Physician of Advanced Dermatology, PC, explains.
What could possibly cause red dots on the skin?
Many things can cause this, and some of those causes are cancer.
Dr. Fox says that red dots have many causes from a variety of skin conditions. Here is a list of the most common:
– Red bumps – can be pus-filled over the face, chest and back: acne
– Reddish raised flat sores: allergic reaction, irritant or allergic contact dermatitis, herpes, malaria, heat rash
– Reddish dome-shaped bumps, appears sprinkled randomly and itchy: insect bites
– Small red dot, larger or bruise-like spots that appear after taking a medicine: allergic purpura
– Red, raised strawberry like appearance: hemangiomas (scary-sounding name, but very harmless; also called angiomas).

Angiomas. Shutterstock/Timonina
Other Causes
– Reddish & flushed appearance around cheeks, chin, forehead and nose: rosacea
– Red, itchy rash that affects the groin area: jock itch, yeast infection, diaper rash in infants
– Expanding, red and slightly itchy rashes over the chest and abdomen: pityriasis rosea
– Scattered pink and red dots when a patient is feeling under the weather: viral infection.
When It Means Skin Cancer…
– Red, scaly, crusted unusual growth on the lip, chin or anywhere on the face: basal or squamous cell carcinoma (below).

Basal cell carcinoma. Shutterstock/Dermatology11

Squamous cell carcinoma. Shutterstock/Dermatology11
– Reddish, irregular shape and colors: amelanotic melanoma (below)
Melanoma
– Reddish, purplish, dark or black raised spots anywhere that keep growing: Kaposi’s sarcoma
– Rarely a skin cancer can present as this: molluscum
If you are not sure what the red dots on your skin can mean, see a dermatologist immediately. Skin cancer needs to be treated immediately.
Don’t assume the growth is basal cell carcinoma, the “best” kind of cancer to have, since it never metastasizes.
To the layman, a single melanoma (deadliest skin cancer) speck can pass for a basal cell carcinoma.
To play safe, have a dermatologist examine you from head to toe once a year.

In 1987 Dr. Fox founded the AAD Melanoma and Skin Cancer Prevention Program in Queens, NY. He has been chief of dermatology of several major teaching hospitals including Mt. Sinai Hospital of Queens.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
How Does Anxiety Cause Dry Mouth?

Don’t confuse thirst with dry mouth, even if you suffer from anxiety.
Don’t confuse thirst with dry mouth, even if you suffer from anxiety. It’s easy to cast off a case of dry mouth to dehydration.
I have had two bouts of dry mouth and was interested in knowing what physiological mechanism triggered these events, especially since the second episode occurred soon after my mother was admitted to the cardiac wing after complaining of chest pains.
My first case of dry mouth happened spontaneously, with no undue anxiety present.
My dentist said that sometimes the condition develops because mineral deposits block the salivary glands.
On the third day of this annoyance, I placed a lemon rind bit in my mouth, stimulating salivation, and the increased salivation washed away the mineral deposits.
However, my second bout of dry mouth, which lasted only several hours, was obviously linked to extreme anxiety.
I doubt that mineral deposits would have blocked my salivary glands for only several hours.
This time I didn’t use a lemon rind; I was at the hospital. I wasn’t breathing with my mouth open, either. But the dry mouth developed. The anxiety was very pronounced.
Stacey Silvers, MD
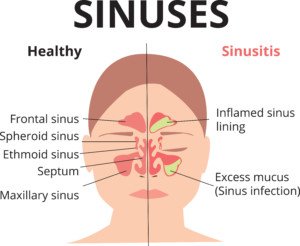
“Anxiety and stress wreak havoc on the body,” begins Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
“There is an increased amount of stomach acid as a result of stress and anxiety.
“Testing, including my own office tests, has shown acid reflux to make it as high as into the back of the nose.
“Stomach acid is a pH of 2 and can kill off some of the healthy bacteria that we count on to keep our oral cavity healthy and hydrated.”
True dry mouth does not feel like thirst or that “parched” feeling you get when working in the hot sun.
It feels like cotton is in your mouth, and you can drink all the chilled water you want, and your oral cavity will still feel dry, as though the inside of it is lined with cotton. It’s a weird sensation.
Nevertheless, Dr. Silvers explains, “Dehydration and poor nasal breathing are other contributing factors.
“I have many patients who have chronic nasal obstruction due to severe allergies or deviated septum.
“Oral breathing is common and often worse at night. It is easy to get dehydrated and suffer with oral complaints when not breathing well through the nose.”
Is there a way to tell the difference between true dry mouth and thirst?
I believe so. Just imagine a tall glass of your favorite icy cold beverage.
If it excites you, you’re thirsty. If it does nothing for you, you have dry mouth.
However, a person with true dry mouth can also become thirsty.
If after guzzling your favorite beverage, you still have that strange cottony feeling in your oral cavity, you probably have dry mouth, which can be a symptom of Sjogren’s syndrome, as well as a side effect from some medications, including, says Dr. Silvers, sleep aids, antihistamines, antidepressants/anti-anxiety, anti-convulsants, prescription painkillers and diuretics, among others.
 An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003. Dr. Silvers is an expert in the field of minimally invasive rhinology, resolving patients’ breathing and sinus problems with simple in-office procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sphenoid Sinusitis Headache Symptoms vs. Aneurysm Headache

A most severe headache can be caused by a ruptured aneurysm as well as from sinusitis, particularly the sphenoid type.
A ruptured aneurysm, and sinusitis, are unrelated medical conditions, though a person by sheer coincidence can suffer from both maladies at the same time.
A ruptured aneurysm will almost always cause a horrible headache.
But the “worst headache of your life” can also result from sphenoid sinusitis.
Does the leaking/ruptured aneurysm headache differ from one caused by sinusitis?
“An acute infection can cause a debilitating headache on the top of the head,” says Dr. Stacey Silvers, MD, of Madison ENT & Facial Plastic Surgery in NYC, who is board certified in otolaryngology; one of her specialties is sinus surgery.
This is the typical location of the sinusitis pain.
Shutterstock/Ekaterina Siubarova
Depending on the sinuses that are affected, the pain can also be over the cheeks, between the eyes and over the forehead.
Dr. Silvers continues, “Patients have been admitted to the emergency room and often observed in the hospital for testing to rule out an aneurysm” that has ruptured.
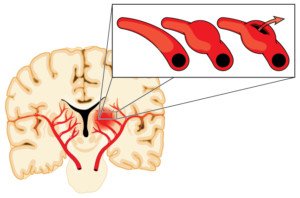
Depiction of an aneurysm. Shutterstock/Blamb
A head pain arising from a burst aneurysm is often described as “thunderclap,” and is usually sudden in onset.
I say usually, because a slowly leaking aneurysm can also cause a less severe headache.
“Patients will have an MRI and MRA, and while (ruptured) aneurysm is often ruled out, the only finding on the MRI may be inflammation of one or both of the sphenoid sinuses,” says Dr. Silvers.
So one thing to keep in mind, regarding a ruptured aneurysm headache, is that it is almost always sudden, hence the term “thunderclap.”
However, how often is a headache the only symptom of a ruptured or leaking aneurysm?
In the case of a ruptured aneurysm, the headache (which is typically of alarming proportions) may be “associated with change in mental status, loss of consciousness, seizures or other focal neurological deficits,” depending on location, explains Carol Redillas, MD, founder of Crescent City Headache and Neurology Center.
Depending on a leaking aneurysm’s location, a condition called ptosis (drooping eyelids) will occur. Sinusitis can also cause eyelid ptosis.
Ptosis: drooping eyelid
Another telltale sign of a possible (note: possible, not definite) ruptured aneurysm is if the headache suddenly slams you in the midst of physical exertion (especially while holding one’s breath).
But a physical exertion headache isn’t necessarily a ruptured aneurysm. Another condition of the eye, called miosis, can result from a leaking aneurysm.
Sinusitis will not cause this, however. An aneurysm will typically leak before it ruptures, says Dr. Redillas.
Dr. Redillas says that a ruptured aneurysm is suspected when a headache is sudden, severe, and unprecedented, and especially if it’s associated with ptosis, miosis and/or neck stiffness, along with cognitive impairment.
This life-threatening condition needs to be immediately ruled out by medical tests when a thunderclap headache occurs.
“If an MRA or a 4 vessel angiogram is negative for an aneurysm and the same headache recurs,” says Dr. Redillas, “then you can be rest assured that your headache is most likely benign.”
A telltale sign (but not always) of the sinusitis headache is that it moves with you as you change position; or, to put it another way, it worsens when you lean or stoop over, squat, do jumping jacks or even milder aerobics, trot down some steps, etc.
It may also be accompanied by nasal congestion or fever, but sometimes the pain stands alone.
Do Not Attempt to Self-Diagnose Headaches
… but do keep a detailed journal of when they occur, any precipitating factors, character of the pain, caliber of the pain, location, etc., so that you can present this information to a doctor.
In the event of sinusitis, Dr. Silvers explains that decongestants and antibiotics are used to relieve the symptoms.
She says, “When the medical management fails, it may be necessary to open the door of the sinus through endoscopes to improve the natural opening in the sinus, culture the sinus drainage, and flush out the infection.”

An NYC expert in ear, nose and throat care, Dr. Silvers has been named among America’s Top Physicians and Surgeons in facial plastic surgery and otolaryngology numerous times since 2003.
Dr. Redillas served as the head of the headache division at Ochsner Medical Center for over 10 years. In addition to headaches, she also treats a variety of other neurological conditions.
served as the head of the headache division at Ochsner Medical Center for over 10 years. In addition to headaches, she also treats a variety of other neurological conditions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Metal Taste in Mouth: Every Cause, Every Solution

Is a metal taste in your mouth driving you mad?
A metal taste in the mouth is no laughing matter, as it can sometimes seem as though you’ve been sucking on a block of iron.
Though a metallic taste in the mouth can sometimes easily be explained by a recent nosebleed, there are other instances of metal taste in the mouth that have no apparent cause, and thus, no apparent solution.
All the Possible Causes — and There Are Many — of a Metallic Taste in Your Mouth
Once you know what’s causing this very unpleasant situation with your mouth, you’ll know what the solutions are.
For starters, medications can cause a metallic taste in the mouth, says Steven Y. Park, MD, Clinical Assistant Professor of Otolaryngology (ear, nose and throat) at New York Medical College.
“One of the most common medications is azithromycin or clarithromycin, or any of the macrolide antibiotics,” says Dr. Park, author of the book, “Sleep, Interrupted: A physician reveals the #1 reason why so many of us are sick and tired.”
Dr. Park adds, “Chemotherapy and anesthesia medications can do this as well.”
Can nutritional supplements be a culprit?
“Certain vitamins, especially those containing calcium or iron, can cause a metallic taste.”
What is the most serious disease that a metal flavor in the mouth can be a symptom?
Dr. Park explains, “Any systemic medical condition that upsets your body’s state of balance can cause you to have a metallic taste, just like weakness, headache, or pain.
“Think of the bad taste as a form of mild pain or a distorted sensation of the taste buds.
“If your nerve endings are hypersensitive (due to stress or illness), then they’ll over-react or react inappropriately.
“The same goes with the tongue, since it has three types of nerve endings: taste, sensation, motor.
“There are theories that propose that the perception of a bad/metallic taste is actually your brain’s misperception, kind of like ringing in the ear.”
What is the most common cause for this most annoying situation?
“I’m not aware of any studies rank ordering this condition, as it’s not a very well studied condition.”
How long would the metallic taste in the mouth have to persist before you recommend the person see a physician?
Dr. Park says, “A few months, at most.”
Can metal taste in mouth be caused by cancer?

Shutterstock/pathdoc
Dr. Park explains, “Any type of growth or trauma can irritate, displace, distort or grow into the nerve bundle that supplies taste. Even benign growths can do this too.
“There also can be general medical issues such as neurologic conditions, either in the tongue or even the brain, that can cause these symptoms.
“Just like pain, fever, or nausea, a metallic taste is not indicative of any specific medical condition.
“It’s only a symptom that can arise from various medical conditions.
“Overall, the chances that it’s due to cancer is very small. This is why a thorough history and upper airway exam is very important.”
Can food allergies cause this?
“Nothing in particular, but anything that upsets the body’s balance can bring on this symptom.
“B type vitamin deficiency has also been implicated. In severe cases, the metallic taste can turn into pain.”
Atlantadentist.com lists the following as possible causes for a metal taste in the mouth:
Gingivitis
Periodontitis
Tooth infections
Peptic ulcer
Lead poisoning
Bleeding gums
Too much dietary iron
Kidney disease
Copper overdose
Selenium toxicity
Iodine intoxication
Mercury poisoning
Atlantadentist.com also states: “When two types of metals are used in two different dental fillings a battery can be created. Some believe that it’s due to the mercury leakage from dental silver/mercury fillings. High protein diets can cause benign dietary ketosis.
“This has also been associated with a metal taste. It has also been associated with B 12 deficiency, zinc deficiency, Bell’s palsy, Strep throat and Sjogren’s disease.”
A cranial cerebral spinal fluid leak can also cause a metal taste in the mouth.
If the cause of the metallic taste hasn’t been figured out, what should a person do?
Dr. Park explains, “There isn’t one reason for metallic taste. A number of different conditions (including dental) can cause it.
“In general, you need to look over your entire medical history and overall state of health.
“It’s also important to make sure you’re sleeping well, as poor sleep can aggravate these type of conditions.
“Checking for any nasal or sinus conditions is also important. Acid reflux is another common condition that can alter your sensation.”
Keep in mind that a metallic sensation in your mouth is not a permanent situation, and it will likely resolve within a few months, if not a few weeks or even several days, especially if you’ve pinpointed the cause.
More on cerebrospinal fluid leak.
 Dr. Park practices integrative medicine and surgery, and has helped thousands of people breathe better and sleep better.
Dr. Park practices integrative medicine and surgery, and has helped thousands of people breathe better and sleep better.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sources: atlantadentist.com; cedars-sinai.edu/Patients/Health-Conditions/Cerebrospinal-Fluid-CSF-Leak.aspx
Hoarse Voice in the Morning: Causes and Solutions

Is your voice hoarse when you wake up in the morning?
Why doesn’t drinking fluids get rid of the morning hoarseness?
Don’t believe what you see on TV: People speaking in a crisp, clear voice the moment they awaken.
Few people, if any, have this gift. Awakening with a hoarse voice is human nature and everyone’s voice sound crummy first thing in the morning.
There are several causes of a hoarse voice upon awakening from an extended sleep.
These include a very long “nap” or a sleep cycle that takes place during daylight for nightshift workers.
I asked two ear, nose and throat (ENT) doctors about this annoying phenomenon.
But first of all, we all know that the more you talk immediately after awakening, the quicker the hoarseness in your voice dissipates.
And if you don’t talk at all, the hoarseness will still eventually disappear — if your first words come a few hours later, the hoarseness will almost always be absent.
My question to both physicians applied to healthy people who do not have infections, colds, vocal cord nodules, reflux, other illness, and who are not heavy smokers or have some other medical condition that causes a hoarse voice.
Steven Y. Park, MD, explains that the hoarse morning voice is caused by stomach juices bathing the throat.
“The simplest way to prevent this or lessen the severity is to eat dinner early (go to bed no earlier than 3-4 hours after eating.),” says Dr. Park, author of the book, “Sleep, Interrupted: A Physician Reveals The #1 Reason Why So Many Of Us Are Sick And Tired.”
Dr. Park continues: “Residual stomach juices can leak up into the throat while sleeping.
“Also, the same applies to alcohol, since alcohol relaxes your muscles, and your juices can come up more easily.
“It also relaxes your tongue muscles, which can cause you to stop breathing and wake up, which not only causes poor sleep, but also forcefully suctions your stomach juices up into your throat.
“All humans are susceptible to this phenomenon to various degrees.”
And that’s not all when it comes to voice hoarseness.
“Morning hoarseness may be caused by mucus accumulation on the vocal cords, and drying of the mucosa (lining) of the vocal cords,” explains Mark Persky, MD, Professor and Chairman, Department of Otolaryngology-Head and Neck Surgery, Beth Israel Medical Center.
What’s ironic is that, before I even questioned the doctors, I had speculated that the chief cause of a morning hoarse voice was “mucus coating the vocal cords.” My mother is right: I should have been a doctor!
Dr. Persky adds that the situation “may be made worse by snoring and during dry weather conditions.”
Now, why doesn’t drinking fluids help ease the hoarse voice?
Many people may think this is an obvious solution, but it won’t have immediate effects “because the swallowing anatomy is separate from the airway where the vocal cords are located,” says Dr. Persky.
However, he continues, “Eventually, fluids absorbed by the body will help hoarseness if it is secondary to drying of the mucosa, although the response will be delayed.”
Can awakening with a hoarse voice be outright prevented?
No. But it can be minimized by using a humidifier in the room to help prevent vocal cords from drying.
Dr. Persky, like Dr. Park, agrees that alcohol should be avoided in the several hours preceding sleep, but also because alcohol is a diuretic and causes the body to lose fluids, which will promote drying.
Dr. Persky says this rule also applies to caffeine.
So upon awakening, what can a person do to get rid of the hoarse voice?
Dr. Persky explains, “Gently clearing the throat of any mucus accumulation will help and well as taking fluids, which will eventually ease vocal dryness.”
The reason fluid intake is still a good idea is that the liquids will get absorbed throughout the body, and this will moisten up the dried vocal cords.
But an immediate response from fluid intake will not happen: Remember, the airway for swallowing fluids does not include the vocal cords.
Finally, “Gargling with a mild saltwater solution will also sooth the throat and help to clear mucus.”




























 Dr. Persky’s
Dr. Persky’s






































