Why Does Ovarian Cancer Cause Appetite Loss?

A gynecological oncologist explains appetite suppression caused by ovarian cancer.
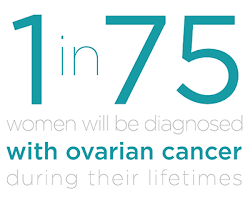
Ovarian cancer can suppress appetite; this is a hallmark feature of this disease, the deadliest of all gynecological malignancies.
I was wondering just what mechanisms are involved that make ovarian cancer lead to appetite suppression.
First of all, realize that if you’ve had a suppressed appetite lately, don’t torture yourself by jumping to the conclusion that you probably have ovarian cancer, which is very rare in premenopausal women.
“Advanced ovarian cancer can sit on the surface of the stomach or the intestines and this can make the patient feel full early,” says Diane Yamada, MD, Chief, Gynecologic Oncology, University of Chicago Medical Center.
“Tumors, extensively involving the omentum, known as an ‘omental cake,’ can also make the patient feel full all the time.”
The omentum is a fold in the abdominal cavity connecting the stomach to other organs.
Dr. Yamada continues, “This full sensation, called ‘early satiety,’ may suppress the patient’s appetite. Ascites fluid can also make the patient feel constantly full, which can suppress the appetite.”
In the case of ascites, which can result from ovarian cancer (and other malignancies such as pancreatic), and non-malignant disease processes such as cirrhosis of the liver, up to two liters of fluid may be present, suppressing appetite, causing a bloating feeling and creating visible distention or swelling of the abdomen.
“In advanced and recurrent ovarian cancer,” continues Dr. Yamada,
“Tumors can also cause a bowel blockage or obstruction, which may make the patient feel nauseous and not want to eat.”
Thus, once ovarian cancer begins causing suppression of appetite, the disease may very well have already spread beyond these walnut-sized organs, into the abdominal area.
Survival rates for ovarian cancer are dismal because usually, this disease is discovered after it has spread.
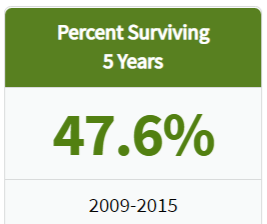
seer.cancer.gov/
This is because there are no screening methods for detection.
If you’re wondering about ultrasound, this tool cannot create an image definitive enough to differentiate between a malignant and a benign mass.
Neither can an MRI or CAT scan. A confirmed diagnosis is made via biopsy (tissue is removed surgically).
Only 19 percent of cases are discovered while the disease is still localized to the ovaries.
These discoveries are made incidentally from imaging tests that the patient receives for other reasons, such as a pregnancy checkup, or X ray of the pelvic area after a car accident.
A “suspicious” mass is detected, and diagnostic follow-up reveals malignancy.
However, such masses aren’t always malignant, either (e.g., benign cysts). Surgery (biopsy) confirms OC diagnosis.
- 68 percent of cases are discovered after the disease has spread to other organs.
- Five-year survival rate for localized disease is 93 percent, and for metastases to distant sites is 29 percent.
Again, if you have appetite suppression, don’t lose sleep thinking it might be ovarian cancer.
Appetite suppression has a myriad of causes, including the fear that you might have ovarian cancer!
You then read up about symptoms and discover that appetite suppression is one of them; suddenly, you can’t eat! Anxiety kills appetite.
 Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/piramidonforte
Source: ovarian-cancer.emedtv.com/ovarian-cancer/ovarian-cancer-survival-rate-p2.html
Ovarian Cyst vs. Ovarian Cancer Detection
A Harmless Ovarian Cyst Can Show Up on an Ultrasound and Masquerade as Cancer
Short of surgery, can a doctor tell the difference between an ovarian cyst and cancer?
Some time ago, I had an MRI for a suspected groin injury. I got a phone call and the exact words were: “You have an ovarian cyst.”
It was then recommended I have a follow-up ultrasound to get a better look at the finding. Right away I began wondering about cancer.
The ultrasound showed the “mass” alright, but the gynecologist was not able to determine with 100 percent conviction that this was just a harmless benign development.
He could not rule out ovarian cancer, but he also could not rule out a dermoid cyst, either, which is benign.
Another possibility (the most likely, according to him) was a “follicular cyst,” which was leftover from the menstrual cycle.
I was told to have a follow-up ultrasound in 30 days to track the image, to see if it was getting bigger or smaller. Size changes are suggestive of composition.
Ultrasound cannot definitively diagnose masses in ovaries, and this includes the corpus luteum cyst (different from the follicular), which is the empty “shell” of a follicle from which an egg is released every month.
“The quality of ultrasound interpretation also depends on the experience of the ultrasonographer,” says Diane Yamada, MD, Chief, Gynecologic Oncology, University of Chicago Medical Center.
Due to its unreliability, ultrasound has created many “false positive” results.
This has caused tremendous anxiety and even unnecessary exploratory surgery for patients who turned out to have nothing wrong.
Subsequent ultrasounds in my case revealed that the mass was “growing,” and this had me freaking.
The gynecologist told me that a follicular cyst will start shrinking, and that’s what we were looking for. So why was this thing getting bigger?
The doctor explained that if it was a follicular cyst, it had not yet reached its maximum size, but once it does, it will start shrinking.
He also held onto the possibility that it was dermoid in nature, which is much denser than the follicular.
I should have realized at the time that a tumor doesn’t grow as fast (in terms of millimeter measurements) as this “cyst” was growing. But I wasn’t thinking that way.
All I knew was that they couldn’t rule out ovarian cancer, but that it was most likely an ovarian cyst, and I had to keep having ultrasounds. Finally, the thing started shrinking. And shrinking.
I was cleared and the diagnosis was a follicular cyst. It’s interesting to note that several of these can show up on an ultrasound at the same time, in various stages.
 Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pixel-Shot
Sources:
mayoclinic.com/health/ovarian-cysts/DS00129/METHOD=print&DSECTION=all
ovarian-cancer.emedtv.com/ovarian-cancer/ovarian-cancer-survival-rate-p2.html
Why Does Ovarian Cancer Cause Bloating?
Ovarian cancer can cause bloating: not just a feeling of bloating, but a visible abdominal distention.
If you have unexplained bloating sensations or your stomach seems to be growing, even though you haven’t been eating more or are not pregnant, make an appointment with your gynecologist, as this could signal fluid buildup in the abdominal cavity.
Though bloating usually is not caused by ovarian cancer, one of this disease’s hallmark symptoms is bloating.
Ovarian cancer is rare, being diagnosed in about 20,000 U.S. women yearly, with 90 percent of them being over age 50.
However, about 70 percent, according to one study, indeed experience bloating as a symptom of their ovarian cancer.
How does ovarian cancer cause bloating?
“Advanced ovarian cancer, where the cancer has already spread to other organs, can cause bloating because a liquid, called ascites fluid, is produced,” explains Diane Yamada, MD, Chief, Gynecologic Oncology, University of Chicago Medical Center.
“This may result in a few extra liters of fluid in the abdominal cavity, which can make the patient feel bloated or pregnant.
“Presumably, bloating may also be caused by extensive cancer sitting on the surface of the intestines.”
Ovarian cancer is the deadliest of all gynecological malignancies (killing almost 15,000 U.S. women yearly), because there is no known reliable screening tool.
Even ultrasound is not reliable, as some ovarian tumors can appear benign, while a benign mass, such as a dermoid cyst, can be “viewed as worrisome for cancer,” says Dr. Yamada.
In fact, ultrasound can’t even definitively diagnose a corpus luteum cyst, which is the empty “shell” of an ovarian follicle from which an egg is released every month.
“The quality of ultrasound interpretation also depends on the experience of the ultrasonographer.”
Because of its unreliability, ultrasound has caused many “false positive” results, creating unspeakable anxiety and even unnecessary exploratory surgery for women who turned out to have nothing wrong.
Even the CA 125 blood test is unreliable for detecting this stealthy killer, in that a woman with the disease can have a normal CA 125, and one without the illness can have a high CA 125.
If you are experiencing bloating, don’t jump to the conclusion that it must be ovarian cancer.

Freepik.com
There are many medical conditions that cause bloating, including a benign cyst.
However, if after a few weeks, the bloating does not seem to be resolving, do schedule an appointment with your physician.
Ask your gynecologist if your ovaries are okay.
By the time symptoms of OC start appearing, many times the disease has spread beyond the ovaries, drastically reducing survival rates.
When malignancy is found on one ovary only, some women will elect to have both of the walnut-sized organs removed, while other women will choose to retain the healthy ovary so that they can become pregnant.
However, another option exists:
Harvesting eggs from the healthy ovary, and then having the organ removed.
“This should only be considered after extensive discussion with a cancer specialist, however,” says Dr. Yamada.
Ovarian Cancer Risk Factors
- Postmenopausal age
- Obesity
- Infertility
- Inherited gene mutation
- Family history of the disease
- Breast cancer
Symptoms Other than Bloating
- Digestive disturbances
- Pelvic pain
- Pelvic heaviness
- Nausea
- Fatigue
- Unexplained weight loss
- Feeling full after small meals
- Frequent urge to urinate
 Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
Dr. Yamada specializes in the diagnosis and treatment of gynecologic cancers including ovarian, uterine and cervical. She is also an editorial reviewer for numerous academic medical journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ShotPrime Studio
How to Tell if a Doctor Misses a Breast Cancer Diagnosis

How can you ever know if your breast cancer has been missed by your doctor?
There are potential tell-tale signs of a breast cancer misdiagnosis that every woman should know.
It is entirely possible for a physician to be in the process of mistaking a malignant breast lump for a harmless cyst.
The information in this article is from a medical malpractice case litigation transcript that I proofread page for page for its court reporter.
This particular case involved misdiagnosed breast cancer.
By the time it was diagnosed properly, the disease was at stage 3 and a poor prognosis.
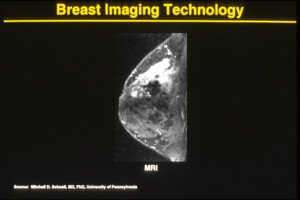
MRI showing a malignant tumor (white area). Cancer.gov
How Breast Cancer Might Be Missed
In this particular case, the plaintiff discovered a lump in her breast. Many women do feel lumps that they believe were never there before.
A mammogram was ordered by the general physician, but the mammogram results were negative.
Women should know that 2D mammograms can miss up to 20% of malignancies.
A needle biopsy of this patient was negative, the mass was drained, and it was assumed to be a cyst.
Several years later the doctor discovered a second lump in the same breast, but not quite in the same location.
For some reason, which was not disclosed in the doctor’s testimony, a mammogram wasn’t ordered.
However, several months later, a mammogram was then ordered. It came back negative.
This time, the doctor did not order a biopsy.
The doctor failed to point out to the radiology center (where the mammogram was performed) that he had felt a mass, yet the mammogram was negative.
He never questioned this conflict. Instead, he literally let it go, and testified that there was no need to follow up because the mammogram had been negative.
The attorney multiple times pointed out that it’s a well-documented fact that mammograms fail to detect 10-15 percent of breast cancers.
Nevertheless, the doctor kept stating that the mammogram was negative, and, to further support the defense, this defendant stated that the radiology center did not offer any recommendations, such as a follow-up ultrasound.
How Things Should Be Done
“Any lump that is felt on exam must be evaluated and explained as either a cyst or a solid,” begins Dr. Kimberly Langdon, MD, OBGYN, medical advisor at Medzino Health, an online doctor and pharmacy site.
“If the mammogram is negative, then an ultrasound will pick up a cyst in general. You can do a fluid aspiration of the breast cyst.
“A lump must be identified as either benign or malignant. It cannot be ignored.”
Testimony was that the physician had believed that the breast lump was probably another cyst, because (once again, here we go) the mammogram was negative, and that he let things go because the radiology lab offered no further recommendations.
Bombshell
The patient’s records indicated that her mother had died from cancer, but the doctor never asked his patient what kind of cancer had killed her mother.
The attorney revealed that it had been breast cancer!
The breast lump seemed to disappear, but then a year and a half later was palpable once more on clinical exam. Another mammogram was ordered. It showed nothing.
Due to miscommunication about this between patient and doctor, the patient was never again seen by this doctor, and shortly after, went to a new radiology center for another mammogram.
This time, the result was positive for breast cancer.
Ultrasound
All of this may be confusing to some women, but it really DOES make a difference when an ultrasound is immediately ordered. Women should push for this, even if a mammogram is negative.
Secondly, she should insist on a 3D mammogram, also known as tomosynthesis. The 3D is more sensitive to picking up suspicious radiographic findings.
Finally, the only way to know what a breast lump really is made of is with a biopsy.
 Dr. Langdon, who is now retired from clinical practice, has delivered over 2,000 babies. Besides obstetrics, she specialized in gynecologic situations such as menstrual disorders, vaginitis, menopause, contraception, pelvic pain and minimally-invasive surgeries.
Dr. Langdon, who is now retired from clinical practice, has delivered over 2,000 babies. Besides obstetrics, she specialized in gynecologic situations such as menstrual disorders, vaginitis, menopause, contraception, pelvic pain and minimally-invasive surgeries.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: mayoclinic.com/health/mammogram/MY00303/METHOD=print
Can Stress Cause Many Missed Periods in a Row?

How many periods in a row can you miss from stress?
Well in my case it looks like five.
“It has been known for years that the menstrual cycle can become dis-regulated when a great deal of stress is present,” says Marcelle Pick, MSN, OB/GYN, NP, in private practice and co-founder of Women to Women Health Center, and author of the book, “Is It Me or My Hormones?”
But ask yourself why ongoing stress would cause only one missed period. It’ll likely be several in a row.
Before I missed the five periods, I had predicted I’d miss at least two in a row. I made this prediction shortly after a stress bomb was dropped on me.
The previous year I had missed two periods in a row, courtesy of ongoing stress involving my mother’s illness. She recovered fully.
Almost a year later I took my mother to the ER, where I was told she needed quintuple bypass surgery with mitral valve replacement; a massive heart attack was imminent without the surgery; the surgery had a 15 to 20 percent mortality rate.
The first day of my last period had been Sept. 28. My mother’s surgery was overnight, October 9 through 10. I began moving my things into my parents’ house.
I just knew I’d be missing at least two periods due to this unspeakable stress. And sure enough, my next period never came.
“This happens because with increased stress, cortisol levels can become very high,” says Pick. Cortisol is the so-called stress hormone.
My mother was having fainting spells at the hospital but she was discharged. I took her to the ER several days later; she was readmitted.
After the second discharge, it was back to the ER; she was readmitted again. Discharged.
Then again to the ER, admitted once more, with a diagnosis of congestive heart failure. Meanwhile, she was blacking out several times a day due to orthostatic hypotension.
Because she was non-compliant with managing this condition, I couldn’t let her out of my sight or she’d black out while upright and risk a serious fall.
Where was my father in all this?
Nine days before my mother’s surgery, he had back surgery and was in no condition to oversee his wife. He was barred from driving for a month.
This meant while my mother was in the ICU (where she had atrial fibrillation and mild kidney failure), I drove to the hospital three times a day (to be present during all three “shifts” of visiting hours).
One-way to the hospital took 40 minutes. (I put my homebased work on hold).
In the weeks following the surgery there were complaints of chest pain and shortness of breath: stress, stress galore, enough to miss several periods over.
Pick explains, “With high cortisol can come thyroid dysfunction, as the cortisol can block T4 to T3 conversion, making the T3 an inactive form which in turn can affect the cycle — and also, continued stress causes adrenal dysfunction which can cause the hormone progesterone to be low — and the cycle can be missed altogether or become irregular.”
My father’s condition never improved (more stress), so the weight of never letting my mother out of my sight fell virtually all on me, which meant every time she got out of a chair, I had to promptly get right behind her.
Dozens of times she passed out and I had to lower her to the floor, including several times in public.
My mother refused to comply to doctors’ treatment recommendations, which caused me ongoing, relentless stress: fear of my mother suffering a life-threatening fall.
She eventually fell when I wasn’t present (after she talked my father into allowing her to resume sleeping with him; prior she had been sleeping downstairs where I was sleeping so that I could escort her overnight several times to the bathroom).
My father slept through her exiting the bed and she hit her head on the bathtub (visible head injury).
A CAT scan at the ER was normal, but I feared there’d be a slow blood leak over the next several weeks.
More battles ensued between my father and me about how my mother should sleep downstairs so I could escort her overnight, but my father again gave in to my mother’s insistence that she sleep with him.
Again she passed out in their bathroom and fell, but no trip to the ER (no visible head injury).
Six weeks after the first fall, my mother awakened with an alarming headache and stroke-like symptoms in her legs.
Another trip to the ER: The CAT scan revealed bleeding in the brain (chronic subdural hematoma).
By this point I had missed four periods in a row.
She had to have brain surgery to drain the blood. The symptoms cleared up after, but soon after discharge my mother began experiencing increasing headaches, then mental fogginess and dysfunction of her left hand.
Another CAT scan showed a recurrence of the chronic subdural hematoma: another hospital admission, another brain surgery. Meanwhile my father had had his coronary calcium score taken: 1,195!
Talk about unspeakable stress; it was no wonder I ultimately missed five periods in a row.
Furthermore, following the second brain surgery, my mother had cognitive impairment, slurred speech and a useless left hand — for eight days post-op. We thought the neurosurgeon botched the job. (She eventually recovered.)
About 145 days after the first day of my last period, I began flowing, after 14 days of spotting!
Yes, stress can definitely make you miss several periods — many periods — in a row.
 Marcelle Pick holds a BS in nursing from the University of New Hampshire School of Nursing and her MS in nursing from Boston College-Harvard Medical School. She is certified as an OBGYN nurse practitioner. Visit “Is It Me or My Hormones.”
Marcelle Pick holds a BS in nursing from the University of New Hampshire School of Nursing and her MS in nursing from Boston College-Harvard Medical School. She is certified as an OBGYN nurse practitioner. Visit “Is It Me or My Hormones.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why Is There Blood in Cervical Mucus after Period Ends?
![]()
An OB/GYN explains reasons for blood in cervical mucus after menstruation is over.
Have you noticed blood in your cervical mucus even though your period has ended?
Perhaps you’ve noticed the blood in the cervical mucus on Day 8 or 9 of your menstrual cycle, or even on Day 11 or 12.
This can be scary, wiping yourself and looking at the mucus on the tissue paper, and seeing a red tinge to it.
When blood appears in cervical mucus, it either gives the mucus a pinkish tinge, or, the tinge can be pinkish-brown, or light brown.
Sometimes, blood in cervical mucus can present as a thin red streak or red hair-thin strand.
Cervical mucus is normally yellowish, cream-colored or somewhat clear, like egg whites.
So to see blood in there, when your period has ended, can be unsettling – unless you know what’s really going on.
For this article questions were addressed by Dr. Christine E. O’Connor, MD, an OB/GYN with the Weinberg Center for Women’s Health and Medicine at Mercy, Baltimore, Maryland.
If you’ve never been concerned about trying to get pregnant, chances are that you do not know that red, pink or brown in the cervical mucus is a sign of fertility.
When a new egg is released by the ovary, the process can cause a minute amount of blood leakage that makes its way to the cervix, and then gets picked up by expelled cervical mucus.
This is called mid-cycle spotting, and women who are trying to get pregnant, who have studied up on the subject, welcome this fertility sign.
Two other causes for cervical mucus that has red, pink or brown in it is leftover, residual blood from your last period.
And also when a fertilized egg implants itself into the uterus – you are pregnant, and with this implantation spotting, the blood can end up in the cervical mucus.
But can other things explain when cervical mucus has a reddish, pink or brownish tinge?
This article is about blood in the cervical mucus, rather than general spotting or bleeding in between periods.
Spotting or bleeding in between periods doesn’t necessarily occur with the expulsion of cervical mucus.
For example, a symptom of uterine cancer is bleeding in between periods, but this blood can find its way through the cervix and onto toilet tissue in the absence of cervical mucus.
Certain forms of exercise can cause anal or vaginal fissures that release minute amounts of blood, that can find its way to toilet paper after you’ve wiped yourself.

Pressure on the anus and vagina. Shutterstock/Seasontime
This appears as tiny bright red specks or red hairline streaks (the brightness indicates it’s fresh), and there may not even be any sign of cervical mucus with it.
Blood in between periods can also signal a problem with the gastrointestinal tract.
But what about blood specifically in the cervical mucus, after your period has ended?
Can anything else cause it besides the already-mentioned?
Dr. O’Connor: Absolutely! This can be caused by hormonal fluctuations (i.e., from stress and weight changes), breakthrough bleeding if on hormonal birth control, any change in medications or over the counter supplements.
This can also be an early sign of cervical infections or vaginal infections, or an early sign of cervical or uterine polyps, fibroids, cancer, etc.
Any spotting or pinkish/brownish tinge in the cervical mucus that is new or a change from what has been previously noted is worth discussing with a gynecologist to determine if it is normal or may need additional attention.
Concerning blood specifically coming out with the cervical mucus, after a period has ended (Day 8-12 or 13), can this be caused by factors other than: a new egg released; implantation of fertilized egg; and residual blood from the ended period?
Residual menstrual blood would be seen just after a period ends. An implantation bleed would cause bleeding just before or when the next cycle would be due. Mid-cycle would be the timing for ovulation related spotting.
But again, especially if there is no predictable pattern or a change from what is normally noticed, there are many other potential causes.
Regarding blood in the CM that’s from, specifically, a newly released egg…can this blood appear in the CM two or three days in a row, or is it almost always a one-day thing?
Blood seen from ovulation is rare, usually a very small amount and for a very short amount of time.
For women who notice this phenomenon, the bleeding around ovulation or mid-cycle is thought to be due to the fall in estrogen levels that occurs just before ovulation.
This would be around Day 12 or 13 in a woman who has perfect 28 day cycles.
Once ovulation occurs, the estrogen and progesterone levels rise again quickly to stabilize the endometrium and ready it for a possible fertilized egg.
What if a woman has ovulation spotting (blood in cervical mucus) on Day 12, can subsequent high levels of stress trip up the cycle such that, instead of her period beginning 14 days later, it begins much later (a very late period caused by stress)?
Generally, menstruation occurs 14 days after ovulation. That is actually the only predictable part of a cycle.
Note: Some women, however, report that their menstruation occurs more than 14 days after ovulation.
 Dr. O’Connor is exceptionally skilled in minimally invasive/endoscopic and robotic surgeries.
Dr. O’Connor is exceptionally skilled in minimally invasive/endoscopic and robotic surgeries.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Pixel-Shot
Late Periods Causes and When to Worry

Can a late period be a sign of cancer? Are late periods really worrying you?
Menstruation normally occurs every 21 to 35 days. After 35 days is a truly late period, and your worry is understandable.
An occasional late period may start between 36 and 40-something days after the start of the last menstrual cycle.
This interval isn’t long enough to be considered a missed menstrual flow, but rather, a late or very delayed period.
A number of reasons can cause your period to be late, and I asked Mary Jane Minkin, MD, clinical professor of obstetrics and gynecology at Yale University School of Medicine, all about the causes.
Just what are the reasons that cause a period to be late?
This assumes that the woman knows she cannot be pregnant.
Dr. Minkin: Anovulation — not having ovulated. Now what can cause that? Perimenopause is certainly one.
As we approach menopause, the poor ovaries just cannot respond to all the FSH (follicle stimulating hormone) and the LH (luteinizing hormone) that the pituitary (gland) sends their way — ultimately, the ovaries will stop producing estrogen, but actually, it is the failure of ovulation that produces the late period.
I thought that you can’t menstruate if you don’t ovulate.
You can get a period from overflow; the lining of the uterus just builds up, and after it reaches a significant accumulation, it just flows out, and it can flow quite heavily.
Thyroid disease is also a common culprit (for late periods). Classically, overactivity (hyperthyroidism) does it; but hypothyroidism can do it, too.
Also, another endocrine disorder, namely elevated prolactin, secreted by the pituitary, can give you late periods.
These women also often have secretion of milk by the breasts.
Prolactin secretion can also be caused by many medications, particularly antipsychotics such as Risperdal.
Also, a medication for nausea like Reglan can elevate prolactin levels.
Of course, depression with stress in and of itself can cause late periods.
Hyper-exercise can screw up periods, even without weight loss.
Eating disorders of course can do it; anorectics seldom get periods. But significant weight gain can do it, too.
Polycystic ovarian syndrome is yet another cause of late periods. Dr. Minkin explains:
This is most often associated with obesity, and most PCOS ladies, because of being heavy, have chronically high estrogen and testosterone levels — so that they never get an LH surge to trigger ovulation, which then makes the progesterone which triggers the period.
Can delayed flow be a sign of serious disease, other than PCOS?
Rarely – they might be just a sign of stress. Something like anorexia is a serious disease, and it does produce amenorrhea, or at least late periods, but as far as something like cancer, no, not very likely.
Cancer of the uterus would more likely present with extra bleeding, not less bleeding.
How often do stress and anxiety cause late periods?
Extremely commonly, and since we really cannot measure stress exactly, stress gets blamed most of the time, when everything else we can measure (like pregnancy, menopause, prolactin, thyroid and PCOS) gets ruled out.
Is there a way a woman can tell if her delayed flow is caused by stress or just a premenopausal body?
The only way would be to measure her FSH level. If it were significantly elevated, you would assume she is in the perimenopausal timeframe.
However, even with a normal FSH, she could be perimenopausal, which we will often diagnose only retrospectively.
If a 40-something woman is experiencing some late periods (beginning on Day 39 or 40, for example, of her cycle), and she’s been suffering an extraordinary amount of stress in the weeks preceding, how likely is stress the cause of lateness, versus being perimenopausal?
Extremely difficult to assess. Perimenopause is often something which takes years, and is very difficult to quantitate.
We do know that the older ovary is less robust, which makes it more vulnerable to stress.
In a nutshell, here is how stress and anxiety trip up the menstrual cycle, causing late periods:
The cerebral cortex of the brain interprets stress in a woman’s life.
This suppresses the cerebral cortex’s efficiency at signaling to the brain’s hypothalamus gland to send instructions to the pituitary gland.
The instructions to the pituitary are supposed to direct it to send a message to the ovaries to ovulate.
This chain reaction gets bungled beginning when the “thinking” part of your brain, the cerebral cortex, feels a lot of stress.
 Dr. Minkin is nationally known in the field of gynecology and is often interviewed and quoted in print and broadcast media, including the New York Times, Wall Street Journal and Time Magazine.
Dr. Minkin is nationally known in the field of gynecology and is often interviewed and quoted in print and broadcast media, including the New York Times, Wall Street Journal and Time Magazine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Roman Samborskyi
Why Does PMS Cause Swollen Ankles?

PMS (premenstrual syndrome) can cause swollen ankles.
Sometimes this is merely a cosmetic issue, appearing unsightly.
But other times, the swollen ankles caused by PMS can be very tender to the touch, even somewhat painful.
Getting swollen ankles from PMS is nothing to worry about, other than the inconvenience.
It certainly doesn’t mean that anything is wrong with your body. There are over 150 symptoms associated with PMS, and swollen ankles is certainly one of them.
I asked Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL, why the swelling results from premenstrual syndrome.
Dr. Fink explaines: “Bloating and water retention are common symptoms ascribed to PMS.
“The exact mechanisms of PMS are unfortunately not known; if we knew, we could much more effectively treat and prevent it.
“PMS certainly has a hormonal connection, as by definition it occurs during a particular time of the cycle.
“‘Retaining water’ tends to cause excess fluid to accumulate in the lowest, most gravity-dependent areas, i.e., the feet (and ankles) from standing, the finger tips, or even in the lower back or coccyx bone in those who sit or lie down for extended periods.”
Is there anything a woman can do to treat the pain in the ankles/feet that may accompany this swelling? (Other than take a pill).
Dr. Fink says, “A natural diuretic may help. Make a tea from apple cider vinegar, or make some homemade lemonade (squeeze a lemon into water – especially warm water. Do NOT over-sweeten. Use minimal sugar or honey).
“This may help mobilize some excess fluid and take the pain/pressure off swelling.”
Having swollen ankles from PMS is no reason to cease exercising.
You can continue exercising as you normally do, though the tighter fit in your footwear may be uncomfortable.
But all exercise is a go, including step aerobics, running and kickboxing.

Shutterstock/bg_knight
Don’t be alarmed if your ankles are tender or sore to the touch; this comes along with the phenomenon.
The swelling in the ankles from PMS will not necessarily disappear overnight.
The condition may persist for up to two weeks, and you may never even get it ever again.
The infrequency of swollen ankles caused by PMS is no cause for alarm, nor is any frequency of it.
Continue treating your body right as usual: exercising every day, drinking plenty of water, restricting processed foods and eating several servings a day of both fruits and vegetables.
Creating an environment where the very best of medicine and gentle gynecology are practiced and where patients come first has always been Dr. Fink’s goal.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/cunaplus
Mid-Cycle Joint Aches or Pain in Women: Causes and Solutions

Mid-cycle joint aches or pain can affect some women.
Mid-cycle joint pain or aches are when a woman experiences a discomfort in her joints that feels just like the joint aching she gets in the days leading up to her period (PMS discomfort).
However, these joint aches occur about mid-cycle, out of the PMS range.
If a woman experiences mid-cycle discomfort in her joints, she can assume it’s related to the increased production of hormones called prostaglandins.
These are the same hormones that cause joint pain during PMS and even during her period.
“Prostaglandin is a chemical released in the body designed to cause a particular response,” says Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL.
“Prostaglandin is released in response to trauma, for instance, and it leads to activation of the immune system and inflammation.
“It is a cause of pain, as the body releases it to try to protect itself in some way – even though the result may be unpleasant and unhelpful.
“It causes headaches. It causes fever. It causes smooth muscle contractions, such as cramps.”
The joints in the neck, wrists, lower back and ankles can be affected.
The aching is not the same kind of discomfort felt if you’ve over-exercised or have arthritis.
“When the ovary releases its egg at mid-cycle (ovulation), the body may perceive this as a type of trauma,” says Dr. Fink.
“Many women feel cramps at the time of ovulation, and some have severe pain (known as ‘mittleschmirtz,’ or painful ovulation).
“These are caused by prostaglandin. In fact, sometimes a small amount of fluid is released into the abdominal cavity at the time of ovulation that may indeed cause a great deal of inflammation.”
So if a woman gets joint pain or aches at around mid-cycle (and the discomfort may persist for several days), this suggests that there’s either larger amounts of prostaglandins being secreted when she ovulates, or, her joints are sensitive to changes in her body’s metabolic processes.
However, despite the annoying nature of mid-cycle joint aches, this problem, when caused by the monthly cycle, does not indicate a medical problem.
Solutions for Mid-Cycle Joint Aching or Pain
Dr. Fink recommends taking a medication that inhibits prostaglandin production: namely, ibuprofen (Motrin, Advil), or Tylenol.
For best results, take the drug before the onset of discomfort.
“If your pain level is 10 out of 10 and you take a pain med, the best you will do is to bring it down to a 7 or 8.
Prostaglandin levels are already high, and they are hard to bring down.
“However, if you can stop the process before it gets out of control, you will be much more effective in managing this discomfort.
“If the pain level is a 2 or 3 because prostaglandin levels are rising and you take the medication, you can prevent the prostaglandin levels from maxing out and thus prevent the discomfort from escalating.”
Prostaglandins cause mid-cycle pain as well as ovulation discomfort and the classic menstrual cramps.
Dr. Fink emphasizes, “Take your medicine from the first moment you know the time is starting. Don’t be a hero and try to wait until it is bad!
“Preventing pain is much more effective than trying to make it go away.”
Creating an environment where the very best of medicine and gentle gynecology are practiced and where patients come first has always been Dr. Fink’s goal.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Nipple & Breast Burning from Breastfeeding: Causes, Treatments

Experiencing burning in the breasts during breastfeeding or shortly after is not uncommon.
But don’t confuse this with actual pain in the breast. It’s also not the same as soreness.
So what causes burning in the breasts and nipples while you’re breastfeeding your baby?
“I believe you are referring to what is known as the ‘milk letdown reflex,’ or simply ‘letdown,'” says Randy Fink, MD, Director of the Center of Excellence for Obstetrics & Gynecology in Miami, FL, what causes a woman’s breasts to have a burning sensation as a result of breastfeeding.
“Suckling, or nipple stimulation, or even just the sound of the baby crying, may stimulate the hormone that causes milk production (prolactin).
“This hormone causes the breast glands to produce milk, and can sometimes be described as a burning deep within.”
Is there anything a woman can do to relieve this very benign reason for burning in the breasts related to breastfeeding?
Dr. Fink explains: “One soothing act for the burning sensation to apply a cool or cold cabbage leaf to the breast.
“There is a natural component absorbed through the skin which has an anti-inflammatory property, and the cool temperature of the leaf is soothing.
“We also use this remedy for those who suffer with frequent blocked ducts and general breast pain from breastfeeding.”
“Letdown” isn’t the only cause, however, of burning breasts/nipples related to breastfeeding. Another culprit to keep an eye out for is a fungal infection caused by candida albacans.
In addition to the burning, other symptoms might be nipples that are itchy, pink or crusty.
This fungal infection may also be referred to as “thrush,” and can affect your baby as well.
The candida albacans fungus loves to make a home in warm, dark, moist areas, and the nipples of a breastfeeding woman can become attractive to this fungus. So can the dark, warm, moist insides of a baby’s mouth.
Treatment for this involves medications or antifungal creams. However, a woman need not cease breastfeeding during candida albacans treatment.
To help prevent burning in the breasts/nipples during breastfeeding:
You should keep your breasts dry and exposed to the air after feeding.
Make a point of exposing them to the sun several minutes per day, one or two times per day.
Do not use plastic-lined breast pads, as these can trap leaked milk. After each feeding, change the pads.
Always wear clean bras that are 100 percent cotton, and they are to be washed in hot water every day.
Boil the milk pump parts in water every day for five minutes, after using a bleach solution to wash them – every day.
Nipple and breast burning do not have to be a part of breastfeeding your baby.