Do Barbell Squats Hurt Your Shoulders? Pain Prevention Tips

Here are several simple things you can do to help prevent or eliminate shoulder pain from barbell squats.
“Shoulder pain while barbell squatting is a common problem in people with shoulder pathology,” says Joseph Ciccone, DPT, CSCS, a doctor of physical therapy and certified strength and conditioning coach with ColumbiaDoctors in New York, NY.
What causes pain in the shoulders while squatting with a barbell across the upper back?
“Squatting with a flat barbell causes the shoulders to assume an abducted and externally rotated position, which is a high-risk position (not to mention you are applying a large force with a bar and attached weights),” says Ciccone.
Abduction means that the shoulder joints are moved away from the midline of the body.
Those whose shoulders hurt during barbell squats, says Ciccone, will likely have at least one of the following going on:
- Instability in the joint
- Rotator cuff tears or strains
- Labral tears
- Reduced mobility in the thorax and/or glenohumeral joint
- Decreased scapular mobility.
What can you do to prevent pain from barbell squats?
Ciccone says to use a different kind of bar such as a buffalo bar, cambered squat bar or safety squat bar.

Buffalo or bison bar

Cambered bar
“These types of bars allow the shoulder to be in a much safer position while still maintaining proper form during the squat exercise.”
The next preventive approach is to perform front squats, that is, holding the barbell at your front.
This isn’t a practical approach if you normally use very heavy weight loads unless you use a Smith machine.
Nevertheless, give it a try, making sure to master this version before piling on the resistance.

Front squat. Shutterstock/Syda Productions
For those who intend on sticking to light resistance, they can use different implements such as kettlebells, dumbbells and weighted vests.
Another alternative is to do single-leg squats, which can be done with body weight only, or while holding dumbbells. These can also be performed using a Smith machine.

Shutterstock/Artsplav
Shoulder Stretch
Finally, stretching the shoulder prior to barbell squats will go a long way in helping reduce or even prevent pain, depending on what’s going on in the joint in the first place, which may simply be a case of stiffness.
A most useful stretching technique is to position yourself under the bar of a Smith machine or a bar at a squat rack (as you would to prepare for squats behind the neck).
Next, place hands lightly on the bar — but very far apart — and simultaneously externally rotate the shoulders as you maintain your position, leaning forward to get in a good stretch.
Lean forward for reps, meaning, hold this position for 1-2 seconds, then release, 20 times (take your time!), for three sets prior to lifting.
 Joseph Ciccone’s practice focuses on numerous musculoskeletal conditions, including management of chronic and acute injuries, and surgical rehabilitation. He has a strong interest in adolescents, weekend warriors and professional athletes.
Joseph Ciccone’s practice focuses on numerous musculoskeletal conditions, including management of chronic and acute injuries, and surgical rehabilitation. He has a strong interest in adolescents, weekend warriors and professional athletes.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Burning Heel Pain: Five Harmless Causes

Top 5 Causes of a Burning Type of Pain in the Heels
“Burning pain in the heel can be an array of problems,” says Joseph Ciccone DPT, CSCS, a doctor of physical therapy and certified strength and conditioning coach with ColumbiaDoctors in New York, NY.
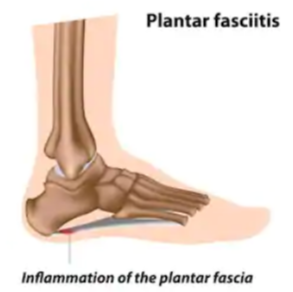
1 Plantar Fasciitis
The first up is, not surprisingly, plantar fasciitis, a more common cause of burning in the heel, says Ciccone.
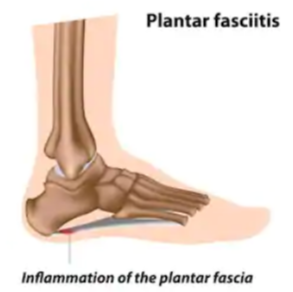
Shutterstock/Alila Medical Media
He adds that plantar fasciitis can be caused by “running on hard surfaces, not changing running path/route frequently, not changing shoe wear when it is appropriate, changing running pattern, i.e., switching to a forefoot runner without proper staged progressions, not having appropriate shoe wear or support.”
2 Obesity

Shutterstock/Motortion Films
Obesity is another cause of plantar fasciitis, along with “playing sports where you need a lot of foot push-off — example basketball, racquet sports, runners — starting an exercise program without proper guidance; example: starting too aggressively.”
3 Achilles Problems
The third possible cause of burning heel pain is Achilles tendonitis/tendonopathy.
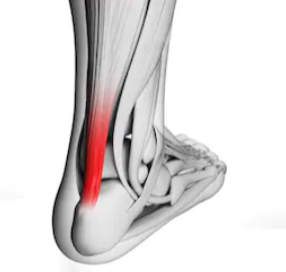
Shutterstock/Sebastian Kaulitzki
Ciccone explains, “Many people are over-pronators and need support to correct foot abnormalities, which can cause stress on plantar fascia and/or Achilles tendon — an example of this would be someone with forefoot varus (bone alignment abnormality in the toes).”
Over-pronation refers to rolling the inside part of the foot inward as you walk or run.
4 Haglund’s Deformity
The fourth possible cause of burning pain in the heels is that of Haglund’s deformity, a protruding or enlarged area on the back of the heel bone.
This growth can cause irritation and pain where the Achilles tendon attaches to the heel.
Wearing shoes with high heels, plus foot mechanics and genetics may contribute to this condition.
5 Arch Problems
No.5 is a pes planus (flat foot) or pes cavus (high arch).
Flat feet: Instead of the usual curve in the middle of the foot, the entire sole may touch the ground. This can be a condition from birth or develop over time.
High arch: This often means that only the heel and ball of the foot make contact with the ground, while the rest of the foot is elevated.
Bonus Cause: Tight Calves

Shutterstock/Shaynepplstockphoto
The sixth likely cause of a burning sensation in the heel would be tight calf muscles — those of the gastrocnemius and soleus muscles.
Tightness in these muscles can actually lead to plantar fasciitis, which is notorious for a sensation of burning in the heel.
To perform an effective calf stretch, face a wall with your hands pressed against it for support.
Position one foot forward and extend the other leg back, keeping the heel of the back foot firmly on the ground and the toes pointing straight ahead.
Gently lean into the wall while bending your front knee and keeping the back leg straight.
You should feel a stretch along the calf of your back leg.

Freepik/katemangostar
Hold this position for 15-30 seconds, then switch legs.
This stretch helps lengthen the calf muscles and can help relieve burning in the heel.
 Joseph Ciccone’s practice focuses on numerous musculoskeletal conditions, including management of chronic and acute injuries, and surgical rehabilitation.
Joseph Ciccone’s practice focuses on numerous musculoskeletal conditions, including management of chronic and acute injuries, and surgical rehabilitation.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/catinsyrup
Does a Blue Mole Mean Possible Melanoma?

A dermatologist weighs in about what a blue mole most likely means and if this can signal melanoma.
“Yes, some moles will appear blue in a clinical exam and they are called blue nevus moles,” says Ben Behnam, MD, is a board certified dermatologist from Dermatology & Hair Restoration Specialists in Santa Monica, Calif.
A nevus (pronounced knee-vus) is the medical name for a mole.
Dr. Behnam continues, “In reality its not really blue, but instead the way the light hits, combined with the person’s skin tone, makes it looks blue.
These blue moles are typically noncancerous but might be malignant.
“They can look suspicious and I would recommend getting it checked out by a board certified dermatologist, as it is possible for some melanomas to appear as dark blue.”
Ask yourself, has the mole always been blue?
If not, get it biopsied immediately.
This means that a dermatologist excises the entire blue mole, or, at least a portion of it, for analysis under a microscope by a dermapathologist.
If you’ve been aware of the blue mole for some time, and it appears not to have changed in any way, it probably isn’t melanoma, but the only way to be sure is to get a biopsy.
It’s never too early to begin examining your skin on a monthly basis to get familiar with what all the various spots, dots and lesions on your skin look like.
This way, you can monitor for any changes of pre-existing spots, or the appearance of new spots.
Be sure the examination includes more obscure areas such as the outer ear folds, behind the ears, the eyelids, the groin, the soles of your feet and between your toes.
A new spot isn’t necessarily concerning; it could be a mere blemish.
But if it doesn’t go away after a few weeks, it would be a wise decision to have a dermatologist look at it with a handheld tool called a dermatoscope.

In addition to skin cancer treatment, Dr. Behnam provides laser, cosmetic and acne treatments, among many others.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can an Age Spot Turn into Melanoma? Yes, Says Doctor
“In a small number of cases, melanoma can start out as an age spot, but typically a melanoma looks darker, is more asymmetrical, has more variation in brown color, making it look darker, and is generally more raised,” says Ben Behnam, MD, is a board certified dermatologist from Dermatology & Hair RestorationSpecialists in Santa Monica, Calif.
It’s best to keep track of your age spots, though this will be difficult if you have a lot of them.
Make a note of how your age spots look, on an individual basis, if you don’t have that many. Examine your face up close every month.
If you’re worried about an age spot turning into melanoma, you should have a dermatologist (not a primary care physician) inspect your age marks on an annual basis.

Melanoma. Omar Bari, Philip R. Cohen/CreativeCommons
In fact, for extra reassurance, have a twice a year examination — in addition to your monthly self-exams.
But don’t obsess about this. As the years continue to march on, you can expect new benign age spots to appear.
You’ll see plenty of these just on the hands of elderly people.
Just keep track of those as you do with the other ones.
In fact, you can expect them to appear over time if you’re at least 40.
Again, do not panic if you notice a new age spot. They’re called “age spots” for a reason: They come with age!
Do not jump to the conclusion that it might be melanoma just because it wasn’t there a month ago.

In addition to skin cancer treatment, Dr. Behnam provides laser, cosmetic and acne treatments, among many others.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
How to Check if Your Moles Are Getting Bigger

Here is a really simple way to tell if one of your moles is getting bigger — even a very tiny dot of a mole.
No apps required! You need only two simple items.
The first is a 3 x 5 index card.
Making Reference Dots for Mole Size Comparison
With a pencil, create a dot on the very edge of the long side of the index card. The size of the dot should be as close as possible to the mole.
This is the baseline dot that should replicate the size of the spot on your skin.
Use an index card, rather than regular paper, because the stiffness makes it easier to handle.
Place the edge of the card, that has the dot, against your skin as close to the mole as possible.
This is how you can compare the size of the dot to the mole, to see if you need to make it a tad bigger to match, or, start over and create the dot again to match the size.
The objective is to make a dot that’s the exact size (and shape, if applicable) to the mole. A bigger mole is less likely to appear as a perfect circle.
Duplicating the shape of a non-circular skin lesion will be challenging to the less-artistically inclined. If you can’t draw, do your best, as this is still a great home test.
Next, draw a second dot that’s a tiny bit smaller than the skin spot (or smaller than the baseline-drawn dot), on the edge of the card, near the baseline dot.
Finally, make a third dot, on the other side of the baseline dot, that’s a bit bigger.
Compare the Dots to See if Mole Is Bigger
You now have three dots. The middle dot is the same size as your mole. If you suspect it’s changing in size, all you need to do, to verify this, is place the edge of the card against your skin near the mole.
The closer the dot is to the edge of the card, the easier it will be to make a side by side comparison between mole and dot.
Without this reference point, it will be difficult to determine if your perception that a mole is changing in size is just your imagination. The index card method is objective and leaves nothing to imagination.
If the size of what’s on your skin begins matching the dot that’s bigger than the baseline dot, you know you’re not imagining that your mole has gotten bigger.
If after a week, the mole then matches the size of the baseline dot, this means that it has returned to its original size.
This is exactly what happened to me when I became concerned over a tiny brown spot. Because I was using the dot method, I knew it wasn’t my imagination that the mole had gotten bigger.
After several days of this, it then began matching the baseline dot that I had drawn, which reassured me that the increase in size must have been due to irritation. A biopsy later confirmed this.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Plantar Fasciitis Pain vs. Heel Spur: Symptom Comparison
“Plantar fasciitis is also commonly called ‘heel spur.’ but the two conditions are not the same,” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health.
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
“A true heel spur typically does not produce a high level of pain unless it presses on the soft tissue in the heel,” says Thompson.
“While plantar fasciitis and heel spurs can occur together, plantar fasciitis is usually the condition that produces the pain.”
The pain of plantar fasciitis can often be described as burning, or as “my feet are on fire.”
I’ve had plantar fasciitis, and it’s not the same kind of pain you might feel as part of a sprained ankle (which I’ve also had) or from getting hit in the ankle from something falling on it like a gym weight plate.
What’s a heel spur?
“Heel spurs are calcifications forming on the bone, that are typically caused by unusual or abnormal motion in the joints over time, excessive tension on the bone from a tendon, severe or repetitive trauma (everyday wear and tear), the aging process, conditions such as osteomyelitis (bone infection) and Charcot foot, and general inflammation (as in plantar fasciitis).”
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Can a Stress Fracture Cause Heel Pain?

That heel pain that’s been bothering you lately just may indeed be caused by a stress fracture.
“Fractures and bruises can create pain in the heel,” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (IPFH.org).
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
What Is a Stress Fracture?
Quite simply, it is a tiny crack in a bone. The injured part of the bone is not severe enough to displace the bone; a cast is not required for healing.
However, a walking boot or brace may be needed to provide support, reduce pressure on the bone and limit movement.
This helps the fracture heal properly by preventing further stress or injury.
It also reduces pain and allows for safer, more comfortable mobility during recovery.
The bones of the lower leg and foot are the most vulnerable to a stress fracture. These, of course, include the heel area.
Physical activities that, in particular, can give rise to this kind of injury include jumping, running, basketball, volleyball, gymnastics and figure skating, among others.
But ANYONE can get a stress fracture in the foot.
Thompson explains, “The calcaneus is the primary bone in the heel. Although an actual fracture of the calcaneus is relatively rare, it can be very painful.
“A fracture occurs most often as a result of a severe blow to the heel area, such as a fall from a height or some other serious trauma.
“Calcaneus fractures are often serious and need to be attended to quickly.”
Thompson further explains, “Less severe stress fractures can also be responsible for heel pain, but are typically not as painful as more serious fractures.
“Bruises can also occur as the result of blows to the heel area, and while they can be painful, they are not as serious as fractures.
“Those who are particularly vulnerable to heel bruises are participants in sports that require repetitive jumping and landing on the feet.
“This includes volleyball, basketball and distance running.”
Other sports that include jumping are that of track field events, high intensity interval training involving workout boxes or stools, and parkour, which is a form of running that involves leaping over obstacles.
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/KlaraBstock
Why Your Heels Hurt Like Mad Stepping Out of Bed

Do you dread getting out of bed every morning due to really nasty heel pain?
Does it almost feel like you’re stepping on hot coals?
“A sharp burning pain in the heel area is one of the most telltale signs of plantar fasciitis,” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (IPFH.org).
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
“Plantar fasciitis is inflammation of the plantar fascia, the dense band of fibrous tissue that functions as the main support for the arch of the foot,” continues Thompson.
Shutterstock/By Alila Medical Media
“Plantar fasciitis is most frequently caused by a sudden increase in the level or intensity of activities, overuse, faulty biomechanics (for example overpronation, high-arched feet or other gait-related issues), being overweight, extended periods of standing on hard surfaces and poorly designed footwear.”
I used to have plantar fasciitis in both feet, having developed at the same time.
The trigger was walking on my heels, on a treadmill, wearing hiking boots.
I wanted to break in the boots for extended hikes, and perhaps I got bored just walking on the machine.
So I decided to walk on my heels to target more of the anterior tibialis muscle in the front of the lower leg.
Though I was really into fitness, the risk of plantar fasciitis from walking on my heels didn’t occur to me.
“The sudden pain one experiences when first stepping out of bed in the morning is typically a result of the affected foot’s having been in a relaxed, plantarflexed position (pointing downward) during the night,” says Thompson.
“When the foot is tensed and stretched into a dorsiflexed position (heel down, toes up) to bear weight when the person gets out of bed, it stretches and tears the already inflamed plantar fascia away from its attachment point on the calcaneus (heel bone), causing the sudden and intense pain.”
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/catinsyrup
Why Feet Hurt After Sitting: Circulation Problem, Solution

There is a cause of hurting feet after sitting that may surprise you.
Are your feet in pain or sore after you’ve been sitting for a while, such as while using a computer, at the workplace or relaxing in front of the TV?
“If your feet don’t normally hurt when you are walking or moving about, the most likely cause is that the blood in your feet and legs has not been circulating vigorously while you were sitting,” says Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (IPFH.org).
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot pain.
“The human body is designed for movement; and periods of prolonged standing or sitting have a negative effect on circulation in the legs,” says Thompson.
Prolonged sitting also has a negative effect on the heart, according to research that was reported in Current Cardiovascular Risk Reports, 2008
“The veins in the feet and legs that carry deoxygenated blood back to the heart have to work against gravitational pull,” says Thompson.
“These veins have valves that help the blood flow upward, and there is a ‘pump’ mechanism in the calf muscles of the legs that assists in that upward flow.”
So if you sit for prolonged periods, such as at work, driving long distances, in an airplane or just reading a book, “the lack of muscle activity in your legs may cause insufficient return flow of the blood, causing it to ‘pool’ in your feet and legs,” continues Thompson.
“When you stand up, the extra blood in the feet and legs has to be circulated back up the legs, which may create higher than normal blood pressure in the area, which in turn may cause you to feel pain.”
How can one avoid this?
“The best way is to stand up frequently if you can, and to flex the feet, move the legs and in general avoid sitting still for prolonged periods.
“This is especially difficult on long plane flights, and is especially important to avoid if possible due to the potential danger of blood clots related to prolonged sitting and varying air pressure in airliner cabins.”
Heel or Arch Pain After Sitting
This will almost always be caused by plantar fasciitis, an inflammation of the ligaments that run the length on the underside of the foot.
However, if you have this condition, you’ll also very likely experience it when up and about, not just when sitting, and particularly during exercise or sport.
You’ll also probably feel pain or burning under your feet the moment you get out of bed in the morning.
Plantar fasciitis has nothing to do with poor circulation.
 Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
Robert Thompson is a nationally recognized speaker on the topics of preventive foot health and soft tissue injury prevention.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Top image: Shutterstock/Robert Kneschke
Pain in Feet After Sitting May Be Arthritis or Fibromyalgia

Don’t dismiss arthritis or fibromyalgia as possible reasons your feet hurt after sitting, even though you may have read that a likely cause is plantar fasciitis.
Here is what Bob Thompson, certified pedorthist, executive director of the Institute for Preventive Foot Health (IPFH.org), has to say about the cause of feet hurting after prolonged sitting:
“Another, less likely reason for pain in the feet after sitting for a while is arthritis or a connective tissue problem such as fibromyalgia.
“Both can cause you to feel pain when you put weight on joints that have been inactive for extended periods of time.”
A pedorthist is a medical professional who specializes in designing footwear and devices to alleviate foot discomfort.
The Effects of Obesity
In addition to the above causes, obesity can lead to painful feet when seated and after standing following prolonged sitting.
This is due to increased pressure, inflammation and conditions that can be caused or worsened by obesity such as plantar fasciitis (pain in the heel or sole) or swollen ankles.
Extra weight strains foot structures, leading to aching, tenderness and swelling, especially after inactivity when blood flow changes.
This added stress can damage tissues, weaken arches and contribute to structural problems.
How can this problem be prevented?
In addition to working on weight loss of you’re overweight, Thompson explains that you should “try to avoid sitting for prolonged periods of time, and/or move the feet and legs while seated to help stimulate circulation.”

































































