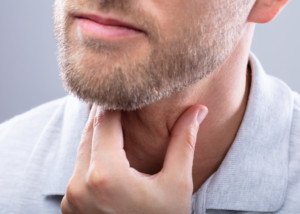
Swollen Neck, Face & Arms: Get to ER Immediately!

If you have a swollen neck, face and arms, this can mean a life-threatening condition that could result in brain death.
The expert source for this article about the cause of a swollen neck, face plus arms is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
“A swollen neck and arms is serious and should lead to immediate attention,” says Dr. Elefteriades.
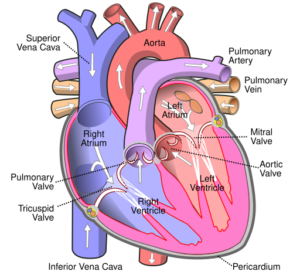
“This symptom complex may well mean that the ‘superior vena cava,’ or SVC, the great vein that drains the upper body, is narrowed or occluded.”
Occluded means blocked.
“If you do not seek immediate attention,” continues Dr. Elefteriades, “your brain may swell, leading to brain death.
“Such narrowing can be caused by tumors compressing the SVC, by blood clots in that area, or, rarely, by an aortic aneurysm compressing the vena cava.”
This situation is termed SVC syndrome.
The most common cause is cancer. Other causes besides blood clots from surgery, and (rarely) the aortic aneurysm, include syphilis and tuberculosis.
The swelling of the neck, face and arms develops gradually; it is not sudden or overnight. Shortness of breath may also be present.
Additional symptoms of SVC syndrome are a blue tinge to the skin, cough and chest pain.
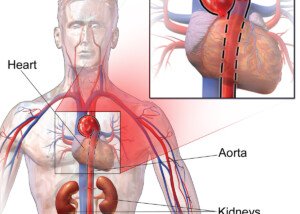
Treatment of the swollen face, neck and arms depends upon the underlying cause that’s disrupting the function of the superior vena cava (see diagram below of the SVC).

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Portnova Tatiana
Source: medicinenet.com/superior_vena_cava_syndrome/article.htm
Chest Pain with Trouble Swallowing: Dangerous & Benign Causes
The causes of chest pain combined with difficulty swallowing can be benign…or life-threatening.
The symptom duo of chest pain plus trouble swallowing is very frightening.
It can occur suddenly and at any time for people who have the life-threatening — or benign — conditions that would lead to this pairing of symptoms.
The expert source for this article about the causes of chest pain with trouble swallowing is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
This pair of symptoms is nothing short of alarming. “Trouble swallowing generally reflects problems with the esophagus, the swallowing tube,” says Dr. Elefteriades.
“These problems may be due to benign conditions, like reflux disease, or to tumors.
“Pain during swallowing reflects partial blockage impeding the contractile wave that propels food in the esophagus.”
Hopefully, chest pain with difficulty swallowing is not more serious than some acid reflux (gastroesophageal reflux disease).
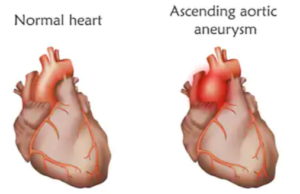
But Dr. Elefteriades adds, “An aortic aneurysm can, rarely, put pressure on the esophagus by virtue of its size and cause the symptom complex” of chest pain and trouble swallowing.
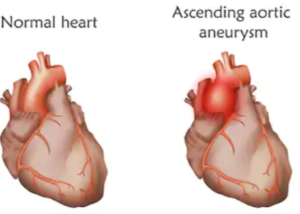
What is an aortic aneurysm?
- An aneurysm of the thoracic aorta is a portion of this great vessel that has abnormal enlargement.
- When an aortic aneurysm causes symptoms, it is time for surgical repair.
- Usually, these do not cause any symptoms, and most are discovered by accident during imaging for an unrelated issue.
Shutterstock/Veronika Zakharova
When an aortic aneurysm is asymptomatic and the patient does not have a connective tissue disorder, the aortic aneurysm is given a “watchful waiting” approach.
This protocol is to see if it gets big enough to warrant surgical repair; routine imaging tests are done to follow it.
Trouble swallowing along with chest pain can also be caused by a hiatal hernia, acid reflux or esophageal cancer.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/fizkes
Sources:
webmd.com/heartburn-gerd/understanding-hiatal-hernia-symptoms
mayoclinic.com/health/esophageal-cancer/DS00500/DSECTION=symptoms
Chest Pain with Neck Pain: May Be Heart Attack

A heart surgeon addresses the likely cause of chest and neck pain occurring at the same time.
Sudden chest pain, or gradually worsening and reaching severe proportions, is frightening enough.
But add neck pain to this symptom, and you have a pairing that can potentially mean a heart attack.
It’s one thing if your neck pain, ache or soreness is obviously occurring independent of a sudden onset of chest pain.
That’s entirely possible. Your neck could be sore from a kind you developed overnight.
Nevertheless, sudden severe chest pain still means you need to get checked out right away.
The expert source for this article about the causes of chest pain that is accompanied by neck pain is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
Sudden Pain in the Neck and Chest: Heart Trouble Possible
Dr. Elefteriades explains, “Chest and neck pain often accompanies a heart attack or an angina episode.”
Angina is a medical condition in which the heart is shorted of oxygen flow due to narrowed or constricted coronary arteries.
The obstruction in the arteries is caused by plaque buildup, which shrinks the diameter of these blood vessels or may cause a very narrowed section.
Angina may occur only upon physical exertion (and it doesn’t have to be a lot of exertion—may be only minor) and mental stress.
Or, it may occur spontaneously without any of these triggers, in which case it’s termed unstable angina, which can mean a near-future heart attack.
Dr. Elefteriades continues, “Every patient feels the (heart) attack differently. Chest pain is nearly ubiquitous, but only a minority of patients have what we call ‘radiation’ to the neck.”
If you’re in the ER for your chest with neck pain, and the blood test (repeated) for heart attack comes back negative each time — this doesn’t mean you’re heart is in the clear.
Chest pain with neck pain is also a possibility with an aortic dissection, which is a life threatening condition.
If this is what’s happening, it will NOT show up on the blood test (troponin) for heart attack.
An aortic dissection can also be missed on a chest X-ray.
An ER doctor will have a high suspicion for an aortic dissection if the patient has also been experiencing fainting or near-fainting episodes, back pain and if the chest pain is described as “ripping” or “tearing.”
An ER doctor should order a CT angiogram to investigate.
Chest and neck pain concurrently can also be caused by an esophageal spasm, which is a non-cardiac issue.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Deep, Throbbing Aching Chest Pain: Causes

Chest pain comes in many flavors, so what could it mean if it’s throbbing, deep and aching?
Three very serious conditions can cause what a patient might describe as a throbbing type of pain in the chest, or a sensation of being deep and aching.
Unfortunately, the first three explanations for these symptoms that come to mind for John A. Elefteriades, MD, are far from benign.
Dr. Elefteriades is the William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
Causes of Throbbing, Deep Aching Chest Pain
Dr. Elefteriades explains, “Chest pains or aches can be the result of coronary artery disease, valvular heart disease or aortic aneurysm. The descriptor ‘throbbing’ is uncommon.”
- Coronary artery disease. People can live to 90 or more with this condition. But if you don’t take measures to aggressively manage CAD, it can kill you long before you cash in your first pension check.
- People can live years with valvular heart disease, but it can also kill. The key is treatment, which (as with CAD) may require surgery.
It’s important to point out that there are also benign causes of chest pain or aches, such as non-serious arrhythmias, inflammation of the rib cartilage, and acid reflux disease. Even the side effects of some medications can be a cause.
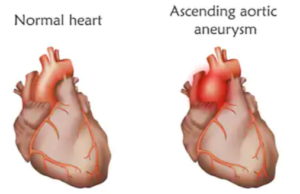
Aortic Aneurysm: Deadly and Stealthy
What very few people know is that a thoracic aortic aneurysm — though usually not causing any symptoms — can cause a very deep or penetrating chest pain — and quite suddenly.
Shutterstock/Veronika Zakharova
The imaging tests that a doctor will order to examine the heart, such as an X-ray (standard ER procedure) or an ultrasound (echocardiogram) will show the aneurysm.
An aneurysm that is producing symptoms like chest pain or aches can be surgically repaired.
If the bulge in the aorta ruptures, internal hemorrhaging will result. Mortality is high.
Other symptoms with a dissecting aortic aneurysm might be severe shoulder and/or back pain.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Chest Pain with a Cough: 3 Most Likely Causes

The three most likely causes of chest pain with cause can kill you, and two within minutes of getting the symptoms.
The expert source for this article about the causes of chest pain that is accompanied by a cough is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
There are three dangerous conditions that can cause chest pain WITH a cough.
If you suddenly develop a cough along with pain in your chest, this probably means one of three life-threatening conditions.
Dr. Elefteriades says, “Cough and chest pain are probably most commonly caused by pneumonia, pulmonary embolism or heart attack.”
Pneumonia
Now, when you first develop signs of pneumonia, your life is not in immediate danger, but you will need to seek medical treatment.
Untreated, pneumonia can be fatal.
A heart attack speaks for itself.
This event can cause chest pain, of course, but also a cough (along with pain in the jaw, neck, arm, shoulder or back, sweating, nausea, vomiting and/or shortness of breath). Get to the ER as soon as possible for evaluation).
Pulmonary Embolism
This has striking risk factors that don’t just occur out of the blue.
A pulmonary embolism is a blood clot in the lung, that originates from what is called a deep vein thrombosis.
A DVT usually develops in the lower extremities, but a DVT can also occur in the upper extremities.
Risk factors for a DVT/pulmonary embolism include prolonged periods of bed rest, sitting still on long airline flights or car rides, surgery, dehydration, elderly age, smoking and excess body fat.
However, no adult is immune to a DVT/PE.
Tennis champion Serena Williams, even, was treated for a pulmonary embolism (her biggest risk factors are believed to have been prolonged bed rest and a long airline flight following foot surgery).
The coughing that results from a pulmonary embolism typically comes with blood and sputum.
Other signs of a pulmonary embolism include clammy or blue-tinged skin, excessive sweating, unilateral leg swelling, lightheadedness, fainting and rapid/weak heartbeat.
Another Possible Cause of Chest Pain with a Cough
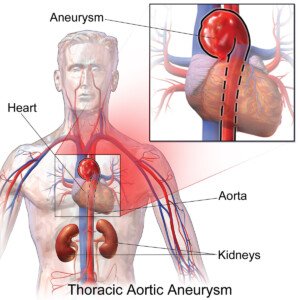
Dr. Elefteriades says “Aneurysm can cause these symptoms, but this is lower on the diagnostic list.”
In the ER, the first things that a doctor will check for is the possibility you had, or are having, a heart attack or pulmonary embolism.
The imaging involved in checking for these will reveal an aneurysm if this is the cause—and it would be a thoracic aortic aneurysm—an abnormally enlarged portion of the aorta, the body’s largest blood vessel.
Chest pain with a cough can also be caused by esophageal cancer.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Source: mayoclinic.com/health/esophageal-cancer/DS00500/DSECTION=symptoms
Causes of Chest & Back Pain with Hoarse Voice

Chest and back pain along with a hoarse voice can be caused by one of two life-threatening medical conditions.
The expert source for this article about the causes of a hoarse voice with chest and back pain is John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
Waste no time seeing a cardiologist if you have all three:
Chest pain
Back pain
And a hoarse voice.
They may very well be all connected, though not necessarily.
“Hoarse voice usually arises from vocal problems, either infection, overuse, or polyps or tumors,” says Dr. Elefteriades.
So if a hoarse voice is being caused by an infection or polyp, for example, and you also have chest and back pain that has seemingly coincided with the hoarse voice…then there’s at least two underlying causes, since a polyp or an infection of the vocal cords will not cause chest or back pain.
However, Dr. Elefteriades continues: “In some cases, hoarseness may be due to an aneurysm in the aortic arch or the descending aorta.”
The aorta is the body’s largest blood vessel, originating in the heart and supplying the body with blood.
An aneurysm is an abnormally enlarged or dilated section of a blood vessel.
The bigger an aneurysm gets, the higher the risk of it tearing, dissecting or bursting.
Source: BruceBlaus/CreativeCommons
A person can be dead within minutes from the massive internal bleeding that results.
“The recurrent laryngeal nerve runs right over the site where the aortic arch joins the descending aorta,” says Dr. Elefteriades.
“So, if there is severe aneurysmal dilatation of the aorta, the recurrent laryngeal nerve can be stretched — to the point where it stops working.
“When it stops working, the vocal cord on that side becomes immobile, leading to severe hoarseness.
“The accompanying aneurysm can produce chest or back pain from pressure on the chest wall by its very size.”
If a doctor suspects that this is what’s going on, he will order an image of the aorta, likely using MRI technology.
An aortic aneurysm that causes symptoms is one of the criteria for surgical repair.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/nednapa
Chest Tenderness: What Are the Likely Causes?
A heart surgeon addresses the likely causes of chest tenderness.
“Chest tenderness is not a typical presenting scenario,” says John A. Elefteriades, MD, William W.L. Glenn Professor of Surgery, and Director, Aortic Institute at Yale-New Haven, New Haven, CT.
“Chest tenderness is uncommon.”
Usually, when something is going on in this area of the body, it’s in the form of pain, pressure or tightness.
Dr. Elefteriades says that tenderness in the chest “can be seen after traumatic injury, from rib fractures or from something called costochondritis.”
This last cause is “inflammation (irritation) of the costal cartilages—the soft bone attachments that connect the ribs to the breastbone,” continues Dr. Elefteriades.
Costochondritis can also cause a considerable degree of pain, though it is a benign condition and not at all related to the heart.
Many bodybuilders or those who work out hard with weights are quite familiar with the chest tenderness or sometimes considerable pain that comes with “costo.”
Additional Cause of Tender Chest: Car Seatbelt
Yes, the seatbelt. The belt may be pressed too much against a person’s chest, and at the time this is happening, there may not even be any discomfort.
But a few hours later, or even the next day, one may begin noticing a subtle sensation in the area where the seatbelt crossed over — like a tenderness, not a pain.
One may not make the connection to the seatbelt, either.
But if you DO make this connection…don’t stop wearing your seatbelt!
Tender Chest from Getting Struck There

©Lorra Garrick
Finally, another possible cause of soreness in the chest area is getting struck there during sport, such as a martial arts sparring match or getting hit there by martial arts kicks during tournament.
This can cause bruising, though the bruising may be barely visible.
However, pressing the fingers into the chest area will bring out the feeling of tenderness.

Formerly the chief of cardiothoracic surgery at Yale University and Yale New-Haven Hospital, Dr. Elefteriades is working on identifying the genetic mutations responsible for thoracic aortic aneurysms. He is the author of over 400 scientific publications on a wide range of cardiac and thoracic topics.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: ©Lorra Garrick
Can Aspirin Prevent a DVT in an Immobile Patient?
A woman dies at home from a pulmonary embolism after lying on the floor of her house for four days following arm surgery, having not recovered from the general anesthesia.
A DVT developed during immobility.
The woman developed a pulmonary embolism (which begins as a deep vein thrombosis or “DVT”) at some point while lying immobile for four days on her bathroom floor, after her husband placed her there because it was too difficult for him to drag her from the bed to the toilet.
The hospital had discharged her the day after arm surgery even though she was still in an anesthesia-induced stupor and could not converse, ambulate, eat or drink even water.
Could Aspirin Have Helped?
I asked an expert in the field if aspirin could have helped prevent a deep vein thrombosis (even though, since this woman was not able to hold down water, I wondered how her husband would have gotten aspirin inside her).
“There is no data, as far as I know, that aspirin can prevent or treat DVT in a post-op non-ambulatory patient,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
I also wondered why the discharge instructions didn’t include giving this patient a more potent blood thinner, since the nurse knew that the patient was inert upon discharge.
Dr. Gashti, says, “Anticoagulation with coumadin and/or Lovenox (heparin) can be effective; but again I am not clear at all why this patient went home in the condition she was in.”
This story is the subject of a medical malpractice case, for which I had proofread one of its discovery deposition transcripts, and it’s a mystery to me as well, why a patient who’s not fully recovered from general anesthesia gets discharged.
There was obviously an adverse reaction to the general anesthesia, but she was sent home as though there were nothing wrong.
Well, there most certainly was. She lie immobile on the floor for four days; four days later she was dead from a pulmonary embolism, which begins as a DVT.
The DVT likely developed in her leg, but Dr. Gashti says, “You should also realize that we can also develop DVT in upper extremities as well which can then embolize.”
Upper extremity DVT involves blood clots that form in the veins of the arms, shoulders or neck.
Symptoms often include swelling in the affected arm or hand, pain or tenderness, and visible redness or warmth in the area.
Distension or protrusion of veins near the surface of the skin may also occur, making the condition noticeable.
Several factors can contribute to the development of upper extremity DVTs.
Prolonged immobility, trauma or injury to the arm or shoulder, and certain medical conditions that increase blood clotting, are common causes.
The presence of central venous catheters used for medical treatments can also elevate the risk.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sudden Racing Heart: Causes Other than Anxiety

A cardiologist explains what can cause your heart to suddenly race.
We all know that anxiety or fear can cause your heart to suddenly race, but what’s behind this in the absence of any fear, anxiety, stress or anger?
What if your heart suddenly begins racing while you’re relaxing in the bathtub listening to soothing music?
Sudden Racing Heart
“If it is of sudden onset, and not associated with stress or severe anxiety, it may be an abnormal heart rhythm,” says Robert M. Davidson, MD, a cardiologist with SignatureMD.
“The most common type, especially in younger, healthy people, is called SVT (supraventricular tachycardia),” continues Dr. Davidson.
“In older people, or people with heart disease, it may be atrial fibrillation, which is similar, but irregular (the SVT is regular). SVT is usually at a rate of 130-180 beats per minute, and starts and stops suddenly.
“Atrial fibrillation (AF) typically is at a rate of anywhere from 100-150, but can be faster.
“However, the most common cause of a rapid heart beat is just a speeding up of the normal heart rhythm (sinus tachycardia), and usually is more gradual in onset and offset.
“In order to differentiate between these, a doctor might suggest a portable monitoring device, such as a Holter monitor.”
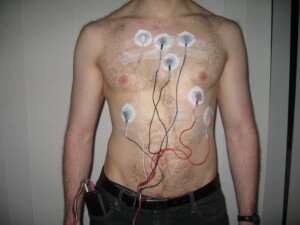
Holter monitor. Jason7825 at en.wikipedia
My mother wore a Holter monitor for 24 hours, but not because she had a sudden racing heart, but instead, to test for AF at some point following bypass surgery.
It’s a small device that’s easily hidden under one’s clothes, and involves several leads (the sticky things that a nurse places on your chest to get a heart rhythm reading).
The device detects abnormal rhythms and documents the time they occur.
My mother simply removed the device after the 24 hours and deposited it at the medical clinic, where her cardiologist later interpreted it.

Dr. Davidson is with the Division of Cardiology at Cedars-Sinai Medical Center, Los Angeles, and has been practicing for 30+ years. Areas of specialty include coronary artery disease, heart attack and palpitations.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/stefamerpik
Chest Tightness but No Trouble Breathing: Should You Worry?

A cardiologist addresses the issue of whether or not chest tightness, but no shortness of breath, should be worrisome.
Have you been experiencing tightness in your chest, but no problem breathing, no shortness of breath — and as a result, you’ve been trying to reassure yourself that there can’t be a problem with your heart?
As long as you can breathe just fine, you figure that your heart is okay?
Think again.
Robert M. Davidson, MD, says that “absolutely!” you SHOULD be concerned if you have any tightness in your chest, regardless of whether you can breathe just fine or have difficulty breathing.
Tightness in the chest is a concerning issue, “especially if it is associated with exertion or stress,” says Dr. Davidson, a cardiologist with SignatureMD.
“Exertional chest pressure is called angina pectoris.
“It is the most common symptom of coronary artery disease, and may be associated with shortness of breath, but not necessarily.”
If you have exertional chest pressure or tightness, but don’t seem to have any unusual difficulty in breathing that seems out of proportion for the amount of exertion, it’s crucial that you have a thorough examination with a cardiologist.
If you have coronary heart disease, the treatment may be only medication and a recommendation of a healthier diet, plus exercise and other healthy habits such as ditching the cigarettes.
Depending on test results, you may also need more pronounced intervention such as the placement of a stent in a narrowed coronary artery.
A stent is a small, mesh-like tube. During a stent placement, a catheter with a balloon is inserted into the narrowed artery.
The balloon is inflated to open up the vessel, and the stent is then permanently placed in the artery to keep it open.
Chest tightness is not normal. Get it checked out by a cardiologist.
WARNING
There is NO way a cardiologist can rule out severe coronary heart disease based on ONLY the following:
A normal stethoscope exam
A normal blood pressure reading
A normal pulse rate
A questionnaire about lifestyle habits in which the patient says they’re active and have a healthy diet.
The fact that the patient does not smoke.
Absence of diagnosed heart disease in family members
An EKG (electrocardiogram)
This is what happened to my mother!
Ten months later, as a result of worrisome symptoms, a few abnormal test results and a catheter angiogram that revealed severe coronary blockages, she had emergency quintuple bypass surgery plus mitral valve replacement and a pacemaker implant!

Dr. Davidson is with the Division of Cardiology at Cedars-Sinai Medical Center, Los Angeles, and has been practicing for 30+ years. Areas of specialty include coronary artery disease, heart attack and palpitations.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.