How Effective is Weight Loss for Arthritic Knee Pain?

Obesity is one of the leading risk factors for osteoarthritis knee pain; it stands to reason that weight loss will improve the condition.
If you have knee pain, particularly osteoarthritis, and are overweight, then weight loss will probably result in a notable reduction in pain — even though osteoarthritis of the knee can affect medium-built or thin individuals.
Just because thinner people suffer from osteoarthritis of the knee doesn’t mean that obesity isn’t a major risk factor.
The knee is not the most stable joint in the body. Most of one’s body weight is above this joint.
Losing weight will have its virtues for those with painful knees.
Don’t let deluded body-positive people on Instagram trick you into thinking that excess body fat cannot cause issues with quality of life.
- Thin people with knee problems are never told to gain weight for symptom relief.
- Plus size patients are routinely told to drop pounds for symptom relief.
Weight Loss Reduces Knee Pain: Study
Research at the Penn State College of Medicine shows that obese patients who had early-onset osteoarthritis of their knees experienced major improvement in symptoms after an average weight loss of 57 pounds.
Exercising with Knee Pain to Lose Weight
When I was a personal trainer I had overweight clients with knee pain. Losing weight is a must for these men and women.
Aerobic activity can assist with weight loss, but painful arthritic knees will interfere with how rigorous the exercise is.
However, upper body strength training can be done very intensely by overweight people with arthritic knees.
- Lying down bench press and dumbbell press
- Seated chest press with a machine
- Seated overhead dumbbell press or shoulder press with a machine
- Seated cable row
- Seated lat pull-down

Overhead Dumbbell Press

Seated Chest Press

Lying Triceps Extension
As for aerobics, some patients will get a clearance from their doctor for pedaling on a stationary bike or elliptical trainer, plus walking inclines on a treadmill, as long as the arthritis doesn’t cause any pain.
A combination of these aerobics plus weight workouts will facilitate fat loss, which will lead to an improvement in the symptoms of knee arthritis.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Hannamariah
Source: sciencedaily.com/releases/2011/02/110219160015.htm
Rotator Cuff Tear Diagnosis: MR Arthrography vs. Regular MRI
Find out which procedure, the MR arthrography or a standard MRI, is better at detecting a rotator cuff tear.
Diagnosing a rotator cuff tear or other type of tissue tear isn’t always as simple as a patient may think, even if the resulting shoulder pain is classical of this condition.
A study that was done at the Neuroskeletal Imaging in Merritt Island, Florida showed that magnetic resonance (MR) arthrography of the shoulder better identifies a rotator cuff tear, when compared to a regular MRI.
However, not all doctors will inform the patient that the MR arthrography is an option.
When a doctor wanted to figure out what was going on with my mother’s painful shoulder, the only imaging study that was mentioned was the regular MRI.
So if you have a painful shoulder or suspect a torn rotator cuff or some other tear (e.g., labral), be sure to inquire about the MR arthrography, which requires that a contrast dye be injected into the joint.
Says Thomas Magee, MD, the study’s lead author, in the report: “With MR arthrography we were able to see things with a high degree of accuracy in the shoulder.”
Dr. Magee explains that with a non-contrast procedure (3T MRI), the “resolution and picture quality” is high, “except for lesions that are hidden without distension (swelling) of the joint,” he says.
“During MR arthrography, distention of the joint allowed us to uncover lesions that could not be seen on conventional MRI.”
The MR arthrogram provides a “better road map for surgeons,” says Dr. Magee.
If you’ve had only an MRI, and your doctor recommends surgery, WAIT — first insist upon the MR arthrogram for a more accurate assessment.
It may determine you don’t even need surgery.
The report appears in the 2009 American Journal of Roentgenology.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Andrey_Popov
Source: sciencedaily.com/releases/2009/01/090106154410.htm
Torn Rotator Cuff Pain: Reverse Total Shoulder Replacement
If you have constant pain from a torn rotator cuff, the reverse total shoulder replacement may be a realistic option.
If you have a completely torn rotator cuff and suffer with constant shoulder pain, no amount of physical therapy or cortisone shots will subdue the pain to the extent where you can live a normal life—especially if you also have arthritis in this joint.
The rotator cuff refers to a group of four muscles and their tendons.
They are frequently the subject of some degree of injury, ranging from strain and overuse, to inflammation and impingement syndrome, to a partial or a complete tear.
However, other things can go wrong for which replacement of the shoulder joint is a viable option.
What is the reverse total shoulder replacement and whom is it for?
The shoulder joint is a “ball-and-saucer” structure. In osteoarthritis, there is bone on bone contact, which causes a lot of pain and is “usually associated with joint stiffness,” says Omer llhai, MD, orthopedic surgeon at The Methodist Hospital in Houston.
In osteoarthritis, there is a wearing down of the cartilage between the bones.
The job of this cartilage is to cushion the bones and to provide shock absorption.
When this cartilage deteriorates, the bones begin to rub against each other, leading to pain, stiffness and reduced joint mobility.
The loss of cartilage not only disrupts the joint’s smooth movement but also contributes to the formation of bone spurs and inflammation, exacerbating the discomfort and functional limitations associated with osteoarthritis.
The reverse total shoulder procedure is not designed to remedy a tear in a rotator cuff tendon.
Rather, this surgery is for the replacement of the warn-down saucer part of the joint with a metal ball.
And the worn-out ball part of the arthritic joint gets replaced with a device — this device contains a big plastic cup.
When the saucer is replaced with a metal ball, and the natural “ball” is replaced with the cup, this renders the shoulder joint no longer requiring an intact rotator cuff for motion or stability.
Hence, the patient’s shoulder joint, with proper post-op rehab and physical therapy, should then function normally.
Prevention of a Torn Rotator Cuff
One of the most effective ways to prevent a rotator cuff injury is through strengthening exercises that target the shoulder muscles — in combination with GOOD FORM.
Exercises that enhance the strength and flexibility of the rotator cuff and surrounding muscles can provide better support and stability to the shoulder joint.
Incorporating activities such as resistance training, stretching and range-of-motion exercises into your routine will help maintain shoulder health and prevent injury.
Proper technique and body mechanics during physical activities are crucial for preventing rotator cuff tears.
This includes using correct posture and alignment while lifting weights, participating in sports or performing repetitive tasks.
Reducing the odds of injury can also be achieved if you devote time to warming up your shoulder joints prior to any intense lifting of weights.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Leszek Glasner
Source: sciencedaily.com/releases/2009/03/090325190508.htm
Is Shoulder Surgery Safe for Elderly with Rotator Cuff Pain?

Find out what kind of shoulder surgery is safer for elderly patients suffering with debilitating rotator cuff pain.
An elderly person may be concerned about complications from shoulder surgery.
However, a Rush University Medical Center study shows that for the elderly, arthroscopic surgery is a safe bet, and it works to reduce pain and improve function. Arthroscopy is minimally invasive.
The paper states that for people over the age of 70 who want pain relief, this relief is a fairly predictable outcome of the surgery.
For those of advanced age, pain relief tends to be a higher priority over that of 100 percent restoration of shoulder function.
An example of function is that of being able to retrieve an item from a high shelf, requiring maximum overhead reach of the arms and hands.
Arthroscopy may not restore all the function in some patients, such as those with a large tear in their rotator cuff, but it will go a long way in relieving the pain.
In short, people over age 70 are not too old for shoulder arthroscopic surgery for the treatment of rotator cuff pain.
Tear in the Rotator Cuff
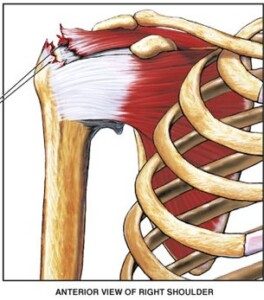
A tear in a rotator cuff tendon. Nucleus Communications, via Wikimedia Commons
“According to a systematic review in 2020, which looked at rotator cuff repair in patients over the age of 70 years, there was a high satisfaction rate with significant improvement in function and pain in this patient population,” says Marc F. Matarazzo, MD, a board certified orthopedic surgeon with Total MD Family Medicine & Urgent Care.
Tears in the rotator cuff occur to about 20 percent of people over age 65.
A surgeon might advise against an operation for elderly patients due to less resilient bone quality and circulation.
But for older people for whom conservative treatments were not effective, arthroscopy is their last hope.
Studies have followed rotator cuff repair patients long-term and found that not only was their pain greatly reduced, but in many cases, their range of motion had improved significantly.
This means being able to raise the surgical arm in front as well as rotate it to the side — motions that were impossible or difficult prior to the procedure.
Another area that the procedure can improve in the elderly is that of strength.
Ninety-four percent of the patients for the Rush University study said they’d have the surgery again if they had to do it over.
Why does arthroscopic shoulder surgery turn out so well for elderly patients?
There are newer surgical techniques, plus the patients’ commitment to post-operative rehab.
However, there will always be patients of elderly age whose rotator cuff tears are determined to be non-repairable, and hence, are not candidates for arthroscopic surgery.
 Dr. Matarazzo specializes in sports medicine and related injuries. He performs minimally invasive and complex reconstructions, and joint replacements, of the shoulder and knee. Dr. Matarazzo is certified in the MAKO robotic-assisted knee replacement system and has 20+ years of orthopedic experience. He has a special interest in cartilage restoration and preservation.
Dr. Matarazzo specializes in sports medicine and related injuries. He performs minimally invasive and complex reconstructions, and joint replacements, of the shoulder and knee. Dr. Matarazzo is certified in the MAKO robotic-assisted knee replacement system and has 20+ years of orthopedic experience. He has a special interest in cartilage restoration and preservation.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Dmytro Zinkevych
Frozen Shoulder Symptoms vs. Arthritis, Plus Treatment
Find out the difference between frozen shoulder and arthritis symptoms, and how to treat frozen shoulder without surgery.
The medical term for frozen shoulder is adhesive capsulitis, and it can be misdiagnosed as arthritis due to the similarity of symptoms.
In frozen shoulder, the tissue around the joint is chronically inflamed; this causes a thickening and tightening in the affected area.
Symptoms of Frozen Shoulder
Significant pain and restrictive movement. These symptoms are also common with other musculoskeletal conditions of the shoulder—such as arthritis.
The right diagnosis may require extensive investigation into one’s medical history.
“Adhesive capsulitis involves idiopathic [unknown cause] inflammation of the shoulder joint capsule, causing pain and decreased shoulder motion,” says Jessalynn Adam, MD, who specializes in primary care sports medicine with OrthoVirginia.
“There are three phases: freezing (the shoulder is painful and stiff), frozen (the shoulder is no longer very painful but motion is significantly restricted), and thawing (shoulder motion gradually returns to normal). This can be quite a prolonged process, up to 26 months.”
Is arthritis sometimes misdiagnosed as frozen shoulder syndrome?
“Perhaps, but age and other health conditions can help to differentiate the two,” says Dr. Adam.
“Frozen shoulder or adhesive capsulitis typically affects middle-aged women between the ages of 40-60.
“It is more common in those with autoimmune conditions such as diabetes, thyroid dysfunction, atherosclerotic/heart disease and Dupuytren’s contracture [a hand condition].”
Painful and Stiff Don’t Always Mean Frozen Shoulder
A report in the 2011 Journal of the American Academy of Orthopaedic Surgeons states that people who have a painful and stiff shoulder are often diagnosed with “frozen shoulder.”
But many things can cause motion loss in a joint.
Details of Frozen Shoulder Symptoms
- Inability to sleep on the affected side due to pain
- Movement so restricted that dressing is difficult, and other things as well like hair care such as shampooing.
- Pain will often decrease once the motion becomes quite restrictive, but pain will bite when the patient makes a sudden movement beyond the confinements of the stiffness.
This is because of microscopic tearing of the scar tissue.
Symptoms of Arthritis
When one tries to move the shoulder, there is often a ratchety or grinding sensation, which is not present with frozen shoulder syndrome.
An X-ray can show arthritis.
Treatment
“Physical therapy focused on capsular stretching, cortisone injected into the shoulder joint to reduce inflammation and pain, rest, time,” says Dr. Adam.
The stretching should be gentle and progressive over a period of weeks, even months sometimes.
“Most cases respond well to these treatments,” says Dr. Adam.
“Refractory cases can be treated with a high volume injection or manipulation of the joint under anesthesia.”
Surgery is a very last resort, but is rarely needed.
 Dr. Adam specializes in the care of athletes and active individuals of all ages, offering prevention, diagnosis and treatment of sports and exercise injuries. Dr. Adam’s care focuses on muscle injuries and biomechanics.
Dr. Adam specializes in the care of athletes and active individuals of all ages, offering prevention, diagnosis and treatment of sports and exercise injuries. Dr. Adam’s care focuses on muscle injuries and biomechanics.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/wavebreakmedia
Source: sciencedaily.com/releases/2011/09/110907132100.htm
Lisinopril Can Cause Blackouts and Here’s Why
Yes it’s true that the blood pressure drug Lisinopril can cause you to pass out.
That’s a tough situation to be in: hearing you have high blood pressure but that the medication for this can cause a blackout.
So imagine being told that you need a drug such as Lisinopril to lower your high blood pressure (or increase the “squeezing” ability of your heart) — but that this drug can also cause you to black out as a side effect.
“Yes, Lisinopril can cause blackouts if the person is very sensitive to the medication, meaning their blood pressure drops significantly in response to the medication, and such a precipitous drop can cause one to suddenly black out,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
It’s also possible that a person can seemingly be compatible with Lisinopril for a very long time — until the state of their body becomes compromised, making them more vulnerable to blacking out or fainting.
An example of that incompatibility would be recent major surgery.
This can make the body more sensitive to Lisinopril, causing a big drop in blood pressure when the patient quickly rises to a standing position — leading to a fainting episode or feeling like the room is “going black.”
How common is fainting from Lisinopril?
“This is not that common with Lisinopril, but can happen especially if the person is dehydrated or not eating or drinking enough, or is already on other BP medications.”
There’s no way to predict ahead of time with certainty whether a given patient will have this particular side effect.
Reducing the Chance of a Blackout
To reduce fainting risk on lisinopril at home, you should stay well-hydrated, first of all.
One way to ensure this is to get a very large thermos and fill to the top with water at the start of the day, with the goal of finishing all the water by bedtime — in addition to drinking water with your meals and snacks.
Next, be sure to rise slowly from sitting or lying positions; avoid sudden standing.
Also, limit alcohol (better yet, see if you can quit drinking altogether; it’s not good for the blood vessels), and monitor blood pressure regularly.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/forma82
Can Ejection Fraction Be Increased without Drugs?

What can you do to increase ejection fraction if you don’t want to take medications that might cause fainting?
“There are really no other good ways of increasing ejection fraction other than medications,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“Exercise may help to raise ejection fraction, but over the long term is not as proven or effective as ACE inhibitors like Lisinopril or beta blockers such as Carvedilol, which can both cause blackouts.”
If you don’t yet have what would be considered an abnormally low ejection fraction, then what you can do is lead a lifestyle that’s designed to prevent your ejection fraction from getting low enough to necessitate drugs.
Medications do not cure low ejection fraction; there is no cure. Low ejection fraction can lead to congestive heart failure.
Prevention or maximal delaying of this condition comes in the form of avoiding tobacco, engaging in rigorous cardio exercise and strength training, and sticking to an anti-inflammatory diet.

“Aldactone, which is an aldosterone blocking medication, is now also used to help increase ejection fraction after adequate beta blocker and ACE inhibitor doses are already being used,” says Dr. Sayeed.
“It usually does not cause blackouts and may be an option used alone if they cannot tolerate the other two meds.” Aldosterone is a hormone secreted by the adrenal glands.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
Constant Chest Pain & No Other Symptoms: 8 Causes

A cardiologist explains eight conditions that can cause constant chest pain but no other symptoms.
What can possibly cause constant chest pain and no other symptoms?
The most common cause is angina, says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
Angina is chest pain as a result of coronary artery disease.
Dr. Sayeed explains, “If the pain is constant, there is likely a severe flow-limiting coronary artery lesion that is causing persistent inadequate blood flow and ischemia [impaired oxygen supply] to a portion of the heart, resulting in constant chest pain which will usually not abate unless medication is administered or percutaneous intervention as in a stent or angioplasty is performed.
“Or if enough time passes, that portion of the heart will either scar over and the pain will go away, or collateral circulation will develop and the pain will be relieved.”
Collateral circulation is when new coronary vessels develop and transport blood.
If you think you have angina, do NOT assume it will eventually scar over or collateral circulation will solve the problem. You may need a stent or even bypass surgery.
Other causes of constant chest pain without other symptoms:
Pericarditis—inflammation of the sac that surrounds the heart.
This “can cause a constant chest pain that is sometimes resolved with high dose NSAIDS or Colchicine, but sometimes is not relieved and can be constant until the inflammation of the pericardium subsides over time,” says Dr. Sayeed.
“Another cause of constant chest pain is musculoskeletal chest pain. This can be due to inflammation or soreness of the chest muscles themselves, similar to what occurs in other muscle groups of the body.

Shutterstock/Zeljko Matic
“Or it can be due to inflammation of the joint between the ribs and breast bone, causing an arthritis type pain of these joints similar to other joints of the body, resulting in constant chest pain that may or may not be relieved by NSAIDS or other pain meds.”
This last condition goes by the name of costochondritis, and it’s hardly unheard of in the bodybuilding world.
“Another cause of chest pain that tends to be more common in women is nerve related and involves the nerve fibers innervating the chest and the heart,” says Dr. Sayeed.
“These can become oversensitive and cause severe chest pain that cannot be explained by most cardiac tests, as these people often have a normal angiogram and stress testing and no muscle or chest wall or rib-breast bone joint tenderness.
“They are often helped by a pain management specialist.”
More Causes Yet
Dr. Sayeed continues, “Other causes of constant chest pain can be hiatal hernia which is when the stomach herniates [enters] into the chest cavity.”
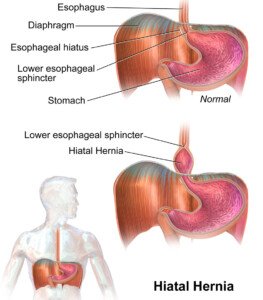
BruceBlaus/CC
The next condition shouldn’t be a surprise, what with all the TV ads about it: gastroesophageal reflux disease (GERD), “due to reflux of gastric acid into the esophagus, causing lower chest pain.”
Next on the list is an esophageal spasm. The esophagus is actually a muscle (though not skeletal muscle).
These spasms tend “to cause very painful constant chest pain.”
Finally, Dr. Sayeed says, “Certain lung conditions causing excessive coughing will also cause constant chest pain.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ANN PATCHANAN
Chest Pain Caused By Muscle Spasm from Stress

Yes, stress and anxiety can cause chest muscles to spasm, resulting in scary “chest pain.”
Chest pain has many causes, including a heart attack in progress, clogged coronary arteries, and muscle spasms induced by stress or anxiety.
“Yes, in extreme cases of stress and anxiety, the chest muscles can tighten just like other muscles in the body in a very anxious and stressed-out person,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“The chest muscles when they do spasm can cause wavering chest pain that can sometimes be mistaken for chest pain related to the heart, and can make people panic and make a trip to the ER.”
If this seems to be happening to you, get a complete exam by a cardiologist to make sure that any symptoms you’re having are not related to your heart.
Stress and anxiety can also cause chest pain as a result of a condition called angina pectoris:
The anxiety or stress increases the body’s oxygen demands, forcing the heart to pump harder.
“Due to constricted arteries (because they’re clogged with plaque), oxygen flow is compromised, resulting in “chest pain,'” says Dr. Sayeed.
COMPARISONS
“The differentiation between muscular and real chest pain can be made by pressing on the chest muscles which may be tender or may be relieved with pressure, whereas this would not occur with real chest pain,” explains Dr. Sayeed.
So next time you experience this symptom, see what happens by stretching your pec muscles.
This can be done by placing both forearms against the outer portion of a door frame and leaning forward.
Another thing to do is to flap the arms back and forth while holding them in a horizontal position, palms facing forward. These motions may make the symptom disappear or diminish.
However, Dr. Sayeed adds, “Also, having the person move or twist their upper body and their arms can sometimes worsen such spasm pain, whereas real cardiac chest pain would not change.”

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Robert Kneschke
Cause of a Stabbing Severe Chest Pain but All Tests Are Normal

Wait till you find out the likely cause of sharp, stabbing chest pain when all your heart tests keep coming back normal.
If you’ve been having sharp, stabbing or otherwise severe chest pain, but the doctors “can’t find what’s wrong” after giving you all sorts of tests, don’t assume nothing is wrong.
That’s because … something probably is wrong.
Probable Cause of Severe Chest Pain when Tests Come Back Normal
“This type of stabbing, ripping chest pain with normal tests is seen with acute pericarditis, especially in younger people,” says Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“This is an inflammation of the sac that surrounds the heart, and when it gets irritated classically causes stabbing chest pain,” continues Dr. Sayeed.
Acute pericarditis can be missed.
“Oftentimes, lab tests, EKG, chest x-ray, echo are all normal, particularly very early in the course,” says Dr. Sayeed.
“The symptoms can be anywhere from mild and brief up to a day or two, to more severe and long-lasting up to several months.”
The sharp stabbing pain may be in the middle of the chest (behind the breastbone or sternum) and/or on the left side.
Of note, the pain isn’t always of a piercing or stabbing nature. It may also be dull or aching.
In either case it may radiate to the left shoulder and even the neck. The discomfort, wherever it is located, may get worse when you inhale deeply, cough or lie down.
Other symptoms may be swelling in the stomach or a leg, weakness or fatigue, and shortness of breath which may be worse upon lying down.
If symptoms last longer than three months, the situation is considered chronic.
Treatment for Acute Pericarditis
Dr. Sayeed says, “It is usually treated with high dose NSAIDS for one month. ” A NSAID is a non-steroidal anti-inflammatory drug.
If not treated in a timely manner, it’s possible for this condition to result in a fatal heart arrhythmia or permanent scarring of the pericardium.
Though a person may prefer that any sharp or stabbing chest pain be the result of pericarditis rather than a heart attack, one must never take the mindset of “It’s just pericarditis.”