Causes of Itchy, Flaky Skin on Your Face
Are you worried that cancer could be causing that unexplained itching and flaking on your face?
The causes of itchy, flaky facial skin are many.
Eczema. “Scaling on the face can be as simple as eczema (atopic dermatitis)—this occurs in children and adults when the barrier function of the skin is altered and the skin is hypersensitive,” says Dr. Rebecca Tung, MD, a
“Oftentimes it is very itchy and may even become infected in patients who aggressively scratch their skin.
“Minimizing the itch-scratch cycle is the cornerstone of treatment — oral antihistamines, topical or oral steroids, and topical medicines that reduce the hyperactive immune response.”
Contact dermatitis. “A specific type of dermatitis called contact dermatitis can cause similar symptoms,” says Dr. Tung.
“However, the culprit is some product or ingredient that is applied to the skin such as a fragrance in a facial cream, preservative in lotion, or even a particular antibacterial agent like neomycin in an over-the-counter wound healing ointment.”
Dr. Tung has even seen flaking on the skin from applying body glitter, which contains nickel, the allergen.
“Even some types of chemical sunscreens can bring on scaly, red, itchy patches on the face. Finding the cause is critical to cure.
“This is accomplished with specialized allergy testing (patch testing)—no needles involved under the guidance of a dermatologist.”
Seborrheic dermatitis. Dr. Tung explains, “Other times infection with a specific type of yeast (Malassezia species) can bring on a case of facial redness and scaling, particularly around the eyebrows, nose and ears as well as is the scalp (dandruff).
“Treatment is successful when the yeast are killed (anti-fungals—topical or oral) and inflammation is minimized (topical steroid).
Others causes of itchy, flaking skin on the face.
“Sometimes if the redness and scaling is accompanied by sun sensitivity—facial redness can signify an autoimmune condition like lupus or dermatomyositis.
“Your dermatologist may order blood tests or perform a skin biopsy to confirm the diagnosis.”
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Causes of Anal Lumps Include Cancer
A dermatologist says there are several causes of anal lumps, and one is cancer.
Most causes of anal lumps are not related to cancer, but cancer can be a cause.
“Lesions around the anus can be as harmless as hemorrhoids (except of course if these hemorrhoids are painful or bleeding—this requires surgical treatment with a colorectal surgeon),” says Dr. Rebecca Tung, MD, a
Skin tags can be another cause of anal lumps, though they won’t really look like true lumps, but they may feel like them against your fingertips. Skin tags are collections of extra tissue.
Other Benign Causes of Anal Lumps
Dr. Tung adds that a skin infection that causes genital warts can be a culprit.
Cancer
Squamous cell carcinoma is a type of skin cancer that can cause anal lumps, says Dr. Tung.
“Fortunately, appearances of each of these conditions are fairly specific, so a skin biopsy is only needed when the look is not typical.
“Skin tags can be numbed with a topical anesthetic and then snipped and cauterized.
“Skin cancers require surgical and possibly additional medical treatment.
“Warts can be treated with freezing (cryotherapy—liquid nitrogen application ), topical medicine application or other minimally invasive procedures like spot chemical peeling, electrical cautery or laser surgery.”
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Can White Pimples on Penis Be Caused by Cancer?
A dermatologist names some causes of white bumps or pimple-like growths on the penis.
White pimples, bumps or small growths can appear on one’s penis; what are some causes?
“The most benign condition that causes flesh colored lesions on the penis is called pearly penile papules—not precancerous or caused by infection—just benign non-cancerous growths that can form a ring around the shaft,” says a
“Other flesh colored lesions could be genital warts (condyloma). Since they are caused by a virus, early treatment is a good idea to get rid of current lesions and prevent spread of new lesions.
“Other white bumps on the penis can be simple cysts (called milia)—harmless and do not require treatment unless bothersome.”
It is extremely unlikely that a white “pimple” or “bump” on the penis can be skin cancer or any kind of cancer.
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sheff
Can a Red Spot on the Lip Be Cancer?

A dermatologist lists many causes of a red spot the lip; find out if cancer is one.
What can cause a red spot on the lip?
Can cancer be a cause?
Rebecca Tung, MD, explains that often, a red spot(s) on one’s lip can be “small collections of blood vessels going by names such as telangiectasia, angioma or venous lake.”
These are benign and can also appear elsewhere on the body.
“Most often there is no particular cause and can be easily treated with a vascular laser,” continues Dr. Tung, a
More Serious Causes of a Red Spot on the Lip
“However, if there are sprays of blood vessels (broken capillaries) on the lips and face/body — this may signal a more serious condition called hereditary hemorrhagic telangiectasia,” says Dr. Tung.
“Affected people are at risk for nosebleeds, acute bleeding in the gut and other internal organs.
“Treatments circles around reducing bleeding from blood vessel lesions.
“Another condition where you can see widespread vascular lesions and thickening of the skin is called scleroderma.
“A particular type of this autoimmune disease is called CREST syndrome—calcinosis (calcium deposits in the skin).”
If you have scleroderma, you’ll have other symptoms far more troubling than a red spot on your lip.
Another condition that can cause red spots on the lip is Raynaud’s syndrome, a vascular disease that affects the legs and other parts of the body.
Dr. Tung names more conditions: “Esophageal dysmotility (cannot swallow properly), sclerodactyly (finger skin becomes abnormally thickened and easily forms ulcers—very painful).
“Fortunately, medicines which adjust the body’s immune response are often helpful.”
As you can see, cancer did not make the list of conditions that can cause a red spot to appear on the lip.
However, if you’re still concerned, ask a dermatologist to inspect it with a dermatoscope, a handheld lighted lens.
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/wavebreakmedia
Can Cancer Cause Red Patches on the Tongue?
Find out if cancer can cause the tongue to develop red patches.
Have you noticed red patches on your tongue and are afraid it might be cancer?
Well, here is some very reassuring news for you…
The most likely cause of red patches on the tongue is a condition called geographic tongue.
What on earth is geographic tongue?
“Geographic tongue describes an inflammatory condition of the tongue that manifests as discolored taste buds,” explains Dr. Rebecca Tung, MD, a
This condition has nothing to do with cancer and will not increase the risk for cancer.
“The red patches are often bordered by white rims—burning and stinging can also be present,” continues Dr. Tung.
The condition looks and feels bad, but is actually benign.
What are the causes and risk factors?
Dr. Tung explains, “Common causes include certain foods, mouth preparations like mouthwash. Also, people with a past history of allergies, hay fever, asthma may have geographic tongue.
“Other risk factors are juvenile diabetes, hormonal shifts in a woman’s cycle or pregnancy or nutritional deficiencies (like having a low level folate or B12 in your body).
“Even patients with the skin disease psoriasis (scaly areas on the forearms near the elbows and knees) also have a high incidence of geographic tongue.”
If you tend to have anxiety over cancer of the tongue (perhaps you’re a tobacco user or for whatever reason have fixated on this body part), this would be one more reason to see your dentist on a regular basis.
Many dentists will do a thorough oral cancer screening as part of the routine exam.
They may charge an extra fee for it, but the fee isn’t that much, and it’s well worth it for patients with tongue and mouth cancer anxiety.
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/antoniodiaz
13 Causes of Burning Lips Explained by Dermatologist

There’s tons of causes of burning lips, and one of them is a pre-cancerous change.
“Burning lips or its cousin burning mouth syndrome can result from a number of causes,” says Dr. Rebecca Tung, MD, a
“Many times it can signal underlying medical conditions such as autoimmune disease (a condition called Sjogren’s disease which can also cause dry eyes); endocrine disorder like diabetes, thyroid disease or menopause; drug reaction; neurologic condition (the nerves that service the mouth are altered); sun damage or precancerous change; infection (a condition called perleche — where the most common culprit is yeast — these patients often get cracking of the skin at the corners of the mouth.”
More Causes of Burning Lips
“Another infection that can affect the lips and cause pain are cold sores or herpes,” says Dr. Tung.
The herpes virus causes cold sores. Cold sores often begin with a tingling sensation in the area where the sore will start forming.
But the tingling may then turn into a burning feeling once the sore is visibly obvious.
If there’s a lingering pink mark where the sore had been after it had scabbed up and fallen off, this is nothing to worry about.
The pink mark may remain for two weeks, but in uncommon cases, it could linger for many weeks — again, this is harmless.
Dr. Tung continues, “Stress, sunlight and even medical or dental procedures around the mouth can bring on an attack of the herpes virus.” So can the common cold.
Many more causes of a burning sensation of the lips are possible, such as poorly fitting dentures, and vitamin and mineral deficiencies,” says Dr. Tung.
These can especially refer to B vitamins, zinc and iron.
“Some patients with burning lips may have allergies to topical products (lipsticks, metal or toothpaste or whitener ingredients). In other patients, the exact cause may not be clear.”
If your lips are burning, see a dermatologist to get a thorough physical exam — of not just your mouth but of all of your skin. This is important, says Dr. Tung.
“Sometimes a patient may have lesions on the mouth, eyes and genital areas as well as on the skin of the body, which can point to a severe but treatable condition which produces fragile blisters and ulcerations called pemphigus.
“Sometimes the dermatologist may take a sample (biopsy) of the affected skin on the lips or order blood work to find the correct diagnosis and develop a treatment plan.
“Depending on the cause, a course of therapy can be started which can help heal the skin and minimize pain.”
Dr. Tung’s specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
specialties include general dermatology with skin cancer surveillance, moles, melanoma, surgery (Mohs micrographic, laser, skin cancer reconstruction) and cosmetic dermatology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Sergey Golenko
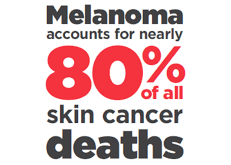
Why Is Melanoma Survival Rate Higher for Stage 0 vs. Stage 1?

What’s different in the stage 0 melanoma patient than the stage 1 patient such that 10-year survival rate is higher?
The earlier that melanoma is caught (or staged), the higher the survival rate when projected 5-10 years out.
So for stage 0 melanoma, the 10-year survival rate is about 99 percent.
For stage 1A melanoma the 10-year survival rate is 95 percent; for stage 1B it’s 86 percent.
What’s going on here? All of these tumors are “thin” and not penetrated into the dermis layer of the skin.
“My own sense of this is as follows,” begins Judith Hellman, MD, Associate Clinical Professor of Dermatology, Mt. Sinai Hospital, NY, who has a private practice in Manhattan.
‘When a melanoma is treated, we follow guidelines in the treatment, and excise some extra skin around the melanoma according to the stage it is.”
That extra-excised skin is normal, as a precaution that in case any tumor cells have strayed, they too get removed.
“In theory, this should be a good measure to know that there will be no mets [spread],” continues Dr. Hellman.
“However, sometimes random melanoma cells can escape the confines of a lesion and the margins of a surgical excision.”
This is more likely to be the case with a deeper (though still confined) tumor. Stage 0 isn’t as deep as stage 1A isn’t as deep as stage 1B, and so on.
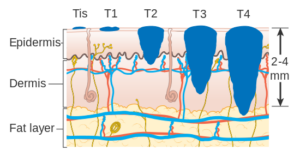
Melanoma stages. Cancer Research UK
“These cells can certainly survive, multiply and find their way to other parts of the body,” says Dr. Hellman.
“Nothing in nature is 100%, so there can always be some undetected cells that can make their own way and grow at a different site.
“I think this is pretty rare in an in situ lesion [the most superficial form of melanoma] or one that hasn’t penetrated very deep.
“It’s also possible that a second, unrelated primary melanoma pops up at some other place.
“We know that anyone with a primary skin cancer is more likely to develop more of the same or other type of skin cancer.
“So I think, ultimately, some cells fly under the radar of the immune system, which polices irregular cells in the body, and manage to develop into a lesion.”
Some cancer cells evade the immune system by mimicking normal cells or producing signals that suppress immune responses.
Additionally, the tumor microenvironment can become immunosuppressive, further shielding cancer from detection.
These strategies allow cancer such as melanoma to grow undetected, complicating treatment and requiring targeted immunotherapies to overcome.
 Dr. Hellman practices medical dermatology and also specializes in laser surgery, anti-aging skin treatments and dermatologic surgery.
Dr. Hellman practices medical dermatology and also specializes in laser surgery, anti-aging skin treatments and dermatologic surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/wavebreakmedia
Source: BigAppleSkin.com
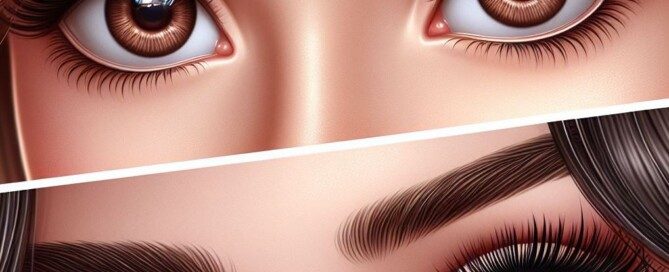
Melanoma Risk with Fair Skin, Brown Eyes vs. Blue Eyes

Find out if there’s a difference in melanoma risk in someone with fair skin and brown eyes vs. fair skin and blue.
Lists of melanoma risk factors often include “fair/light skin and blue eyes.” Sometimes, the list says, “blue or green eyes.”
Melanoma risk lists always name fair or light skin, or Northern European descent—which implies very light tone.
This all begs the question: Is melanoma risk higher in a person with light skin and blue eyes, when compared to an individual with light tone and brown eyes?
“I don’t believe there was ever a statistical difference found (or even investigated) regarding the color of eyes in a person who is fair skinned, as related to their risk of developing melanoma,” says Judith Hellman, MD, Associate Clinical Professor of Dermatology, Mt. Sinai Hospital, NY, who has a private practice in Manhattan.
“It is clear that the lighter the color of a person’s skin, the less protection it has against sun damage,” continues Dr. Hellman.
“A lighter color of hair and/or blue eyes probably just signal that the propensity of that person’s body is to produce less melanin, which is what provides the dark color of the skin, and which is what protects the skin from UV radiation.”
In other words, the more melanin in a person’s skin, the darker the tone will be, and of course, the more likely they will have brown eyes.
However, the color of brown may have nothing to do with the risk of this deadly cancer, and instead, brown is merely a marker for how much melanin a person’s body produces.
Keep in mind that many light or fair people have brown eyes, including Asians and Northern Europeans.
However, a person with dark pigment who has green eyes has a lower risk of melanoma (when basing risk on skin tone) than the Asian or Northern European with very light skin who has dark brown eyes.

Light skin and brown eyes vs. light with blue eyes, and the melanoma risk.
Dr. Hellman explains, “So while the risk may be a tad higher, I don’t believe it’s something that a study would demonstrate.
“Common sense dictates that the lighter the skin, hair and eye color, the more a person should be aware of the risk of melanoma and be vigilant about getting regular skin exams.”
 Dr. Hellman practices medical dermatology and also specializes in laser surgery, anti-aging skin treatments and dermatologic surgery.
Dr. Hellman practices medical dermatology and also specializes in laser surgery, anti-aging skin treatments and dermatologic surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: BigAppleSkin.com
Benign Cause of Brief Stabbing Pains in Breast

Find out a most unlikely, but harmless, cause of sudden-onset, brief stabbing pains in a breast; and it’s not a tight bra.
- Have you developed sudden-onset, stabbing, sharp or piercing pains in a breast?
- And do these stabbing pains in your breast last maybe one to 10 seconds?
- Do they come on with seemingly no provocation? No particular position (walking, jogging, bending over, stretching, reaching) brings them on?
Ask yourself this question: Has your arm been pressing up against the breast lately? This is what happened to me. I developed very brief shooting, severe pains in my breast.
I immediately suspected what I call “compression.” This is when my arm “compresses” the breast by leaning or pressing into it.
In the past, this would happen when I slept overnight on my parents’ couch when staying over. The couch isn’t wide enough for me to lie on my back with both arms straight out at my sides on the couch.
The right arm is forced by the couch’s back support to go up on my tummy. When this happens, the upper portion of the arm presses into the outer quadrant of my breast.
Later on in the day I’d notice on and off, or fleeting sensations or aches in that area of the breast. But they were never stabbing or sharp kinds of pain.
However, when I took to massaging my elbow a certain way (I have golfer’s elbow), I began getting shooting piercing jolts in that outer quadrant, as well as middling through vertically.
I’d lean back into my sofa. The arm of my massaging hand was draped over the breast and pressing into it, in order for my fingers to get a firm grasp on the opposite elbow area; the arm being massaged would rest in the sofa.
During these sessions, there was no breast discomfort. But soon after I’d begin feeling some discomfort coming and going.
One day it escalated like mad and took my breath away. I’m talking JOLTING, BOLTS of pain that lasted one to 10 seconds.
I immediately backed off on the particular massaging position, and predictably, the pain began dissipating. But then I’d be back to the positioning, and the problem kicked up again.
Finally, I decided to abandon the position altogether and massage the elbow another way.
The breast pain completely disappeared, but it took about 10 days, dwindling with each day as far as frequency and severity.
When I went in for my routine physical, I mentioned this to the doctor. She wasn’t the least bit concerned.
She did NOT say anything like, “Gee, we’d better get the breast imaged right away,” or, “I don’t like the way that sounds,” or, “That’s likely a sign of something bad.”
No sir. Her demeanor was as though I were describing pain from a first-degree burn from the stove. I asked her what about the “compression” could cause stabbing pain in the first place?
The doctor wasn’t able to offer an explanation as far as the dynamics, other than to say it could have involved nerves and sensitive breast tissue.
She didn’t think it involved ligaments, but DID say it could have involved the chest muscle. She likened the situation to the pain some women get when wearing an underwire bra.
The sharp, stabbing pain in my breast has disappeared, coinciding with cessation of the compression positioning.
Take a good look at your position habits and see if at any time your arm is pressing into your breast.
The resulting pain can be delayed by hours. If the problem persists despite making a correction to your positioning, see your doctor.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/jcomp
Bilateral Ankle Edema: Causes when Tests Are Normal

A doctor explains what can cause swelling (edema) in both ankles when your heart, liver, kidney and other key tests are normal and you’re not obese.
The following can cause swelling (edema) in both (bilateral) ankles: heart, liver and kidney failure; low thyroid; celiac disease; kidney stones; PMS; excessive sitting or standing; hot weather; varicose veins; high salt (sodium) intake; old age.
Tests for heart, liver, kidney and thyroid function, as well as a blood test for celiac disease, can easily be taken. What if they’re normal?
Does that mean there can’t be other causes of bilateral ankle edema?
“Ankle swelling in general is common, and when painless can be caused by such simple things as gravity, such as when one is on their feet for long time,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “The Fatigue and Fibromyalgia Solution.”
“Low thyroid will also be a common cause, despite normal thyroid tests.” So if your thyroid test was normal and there seems to be no other cause to the swelling in both your ankles, what should you do?
“Relying on thyroid testing misses over 50% of people who need and would benefit from thyroid hormone,” continues Dr. Teitelbaum.
“In this situation, however, there will also be fluid in the fingers, which would not be especially noticeable except for causing rings to be tight.
“The key discriminant factor also is whether the swelling in the ankles is gone in the morning after one has been lying down for an extended period (i.e., with gravity draining their legs),” says Dr. Teitelbaum.
“If this is the case, there is a greater likelihood of the issue being benign. If the swelling is persisting even through the night, or swelling is very marked even just during the day, I would consider a CAT scan of the pelvis and abdomen looking for evidence of venous obstruction – especially from tumors.”
Keep in mind, though, that bilateral ankle swelling is not a more common symptom of cancer, and it’s not even listed by Mayoclinic.com as a symptom of liver, kidney, lung, colon, stomach (esophageal), ovarian or cervical cancer.
However, Mayoclinic.com lists “swelling in the legs” as a symptom of prostate cancer, which also can yield many other symptoms.
A tumor that obstructs lymphatic flow can cause edema in the ankles, but it’s very unlikely that this would be bilateral.
Periomenopause is associated with bilateral ankle edema. Of course, pregnancy can cause this. But what about menopause?

Shutterstock/fizkes
Menopause and the timeline soon after, during which women can still experience annoying symptoms related to menopause, can cause fluid retention in the body.
Edema in both ankles has been associated with menopause.
The key is determining when you think you began developing the edema, and if this coincides with the timeline right before you began menopause, or during menopause.
If “all the tests” have come back normal regarding the cause of your bilateral ankle edema, consider that pulmonary hypertension can cause this symptom.
However, this condition yields other troublesome symptoms such as dizziness, chest pain and fatigue.
Venous insufficiency can cause swelling in both ankles, but this is usually accompanied by leg pain as well.
Sometimes, the cause of bilateral ankle edema is never found.
Dr. Teitelbaum is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
is a board certified internist and nationally known expert in the fields of fibromyalgia, chronic fatigue syndrome, sleep and pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.